
GreenLight photoselective laser vaporisation versus transurethral resection of the prostate for large prostates: systematic review and meta-analysis
Highlight box
Key findings
• This systematic review and meta-analysis found that GreenLight photoselective vaporisation of the prostate (PVP) is non-inferior to transurethral resection of the prostate (TURP) in patients with benign prostatic hyperplasia (BPH) and large prostate volumes (≥70 mL).
• PVP showed significantly shorter postoperative hospital stay and catheterization time, although it had a longer operative time compared to TURP.
• No significant differences were found between PVP and TURP in symptom relief [measured by the International Prostate Symptom Score (IPSS)], maximum urinary flow rate (Qmáx), postvoid residual volume (Vres), or complication rates.
What is known and what is new?
• Prior studies and meta-analyses have established the safety and efficacy of PVP in patients with small to medium-sized prostates.
• This study uniquely focuses on patients with large prostates (≥70 mL), a subgroup often underrepresented in previous analyses.
• The findings expand the evidence base by supporting the viability of PVP as an effective alternative to TURP in this specific population.
What is the implication, and what should change now?
• Given its favorable perioperative profile, including reduced catheterization and hospitalization time, PVP may enhance postoperative recovery and patient satisfaction.
• Current clinical guidelines may consider incorporating PVP more explicitly as an option for large prostates, particularly when shorter recovery is prioritized.
• Further randomized controlled trials with larger cohorts are needed to confirm these findings and evaluate long-term outcomes and cost-effectiveness.
Introduction
Benign prostatic hyperplasia (BPH) represents the most prevalent benign neoplasm among elderly men, significantly contributing to lower urinary tract symptoms (LUTS) (1). The escalating annual incidence, ranging from 41% to 90%, in histologically diagnosed BPH underscores its paramount importance (2). While various interventions exist for BPH treatment, transurethral resection of the prostate (TURP) stands out as a primary surgical approach, introduced in 1943 as an endoscopic procedure to excise the inner prostate portion compressing the urethra. Despite TURP’s historical prominence, the landscape of BPH treatment has evolved with remarkable technological strides, particularly in surgical advancements such as laser therapies, notably photoselective vaporisation of the prostate (PVP). PVP holds promise as a potential replacement for TURP, ushering in a new era of BPH management.
In the latest European Association of Urology (EAU) guidelines (3), TURP, transurethral incision of the prostate (TUIP) or even open prostatectomy are recommended for moderate to severe LUTS in men with a prostate size of 30–80 mL. Laser-based techniques, including PVP, are suggested as alternatives for BPH and LUTS. However, concerns linger in the medical literature about the efficacy in large prostates and the unknown long-term effects of laser surgery. Aligning with that, according to the American Urology Association (AUA) guideline (4), TURP remains the benchmark for BPH treatment, though other techniques are considered feasible based on surgeon experience. Thus, current guidelines collectively favor the traditional technique, TURP, over newer approaches like PVP due to the established scientific foundation of TURP over the years.
Previous meta-analyses, notably Ding et al. (5) and Lai et al. (6), consistently demonstrated the effectiveness and safety of PVP compared to TURP. In patients with small prostates (<70 mL), Ding found PVP to be as effective as TURP, with a superior safety profile, including reduced bleeding and shorter hospital stays. Lai’s broader study confirmed these results across different prostate sizes, highlighting PVP’s non-inferiority to TURP and fewer complications (7).
Unlike previous meta-analyses focusing on small or medium-sized prostates, our study uniquely targets a critical gap by systematically reviewing and analyzing the treatment landscape for BPH in patients with prostates ≥70 mL. This understudied subgroup, often overlooked in existing literature, poses distinct challenges in clinical decision-making. Our research offers a valuable contribution to understanding optimal interventions for larger prostates in BPH patients. We present this article in accordance with the PRISMA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-2025-111/rc).
Methods
Search strategy
This systematic review and meta-analysis was performed and reported in accordance with the Cochrane Collaboration Handbook for Systematic Review of interventions and the Preferred reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) Statement guidelines (8). We searched MEDLINE, Embase, Scopus, Web of Science and Google Scholar from its inception to November 2023 for trials that compared GreenLight Photoselective Laser Vaporisation with TURP, two different techniques routinely used to treat BPH.
Our search strategy in short was: (“Photoselective Laser Vaporisation”) AND (“Transurethral Resection of the Prostate”). We did not use any kind of filter during our search, when regarding about language of publication, year of publication or type of studies.
The references from all included studies, previous systematic reviews and meta-analyses were also searched manually for any additional studies. The prospective meta-analysis protocol was registered on PROSPERO under protocol CRD42023458234.
Eligibility criteria for study selection
The authors included studies that directly compared TURP and GreenLight PVP in adult patients with BPH and prostate volumes ≥70 mL. By focusing exclusively on this specific population, the review aimed to address an important gap in the literature, as large prostate glands are often underrepresented in comparative analyses. Studies were selected regardless of their design (randomised or non-randomised), provided they reported relevant clinical outcomes.
Endpoints
The primary endpoint assessed was the IPSS score (International Prostate Symptom Score), which was compared through 3, 6 and 12 months of follow-up. Secondarily we assessed the maximum urinary flow rate (Qmáx) (3, 6 and 12 months), postvoid residual volume (Vres) (3, 6 and 12 months), operative time, catheterization time, postoperative hospital stay, and the complications. Complications were assessed by Clavien-Dindo (CD) classification (9), and in order to better present the data, we subdivided the results in CD1, CD2 and CD3.
Screening
After deduplication, where we used Endnote online™ 20 (Clarivate, Philadelphia, PA, USA), two independent researchers (B.C.P. and B.C.B.) screened the studies by title and abstract, and disagreements were solved by a third (J.A.S.d.C.). Following this process, full text screening was performed.
Data extraction and quality assessment
Two authors (B.C.P. and B.T.C.) independently extracted the data based on a predefined protocol and disagreements were solved by a third (J.A.S.d.C.). Risk of bias was assessed in randomized studies using version 2 of the Cochrane Risk of Bias assessment tool (RoB 2) (10). Non-randomized studies were assessed with the Risk of Bias in Non-randomized Studies of Interventions (ROBINS-I) tool (11). Two independent authors completed the risk of bias assessment (B.C.P. and B.T.C.). Disagreements were resolved through a consensus after discussing reasons for discrepancy. For every included study, we collected all data available for each of our outcomes.
Statistical analysis
Continuous outcomes are presented as a mean difference (MD) with 95% confidence interval (CI). Dichotomous data are presented as odds ratio (OR) with 95% CI. Pooled estimates were calculated with the random-effects model, considering that the patients came from different populations.
Review Manager 5.4 (The Cochrane Collaboration, Denmark, Copenhagen) was used for statistical analysis.
Results
Study selection and characteristics
After performing our screening, we retrieved 2,380 articles. Following the deduplication and screening process, 5 articles (12-16) were deemed relevant and included in our analysis (Figure 1). For a comprehensive overview of the patient demographics across all included studies, please refer to Table S1. Regarding the design of the included studies, 3 of them were randomized controlled trial (RCT), while the remaining 2 were non-RCT. Combining the data from these articles, we analyzed a total of 159 patients who underwent GreenLight and 159 patients that were submitted to TURP. The mean age of all patients was 70.2 years old. Regarding the potency of the laser used, Horasanli and Tasci used a visible green light at a wavelength of 532 nm, with a potency of 130 W for cutting and 80 W for coagulation. Similarly, in the Mu et al.’s trial (12), the bipolar system controller operated at 280-W cutting power and 80-W coagulation power. As Bachmann et al. (16) and Sarica et al. (15) studies are conference abstract, we could not address the potency of the laser used in the PVP approach.
Meta-analysis
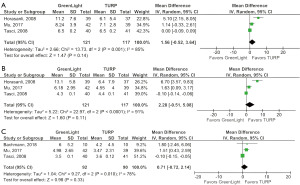
When comparing the IPSS after both surgical interventions, Greenlight and TURP, no differences were seen between groups in 3 months (MD 1.56; 95% CI: −0.52 to 3.64; P=0.14; I2=85%) (Figure 2A), 6 (MD 2.28; 95% CI: −0.12 to 5.08; P=0.11; I2=91%) (Figure 2B) or 12 months (MD 0.71; 95% CI: −0.72 to 2.14; P=0.33; I2=78%) (Figure 2C).
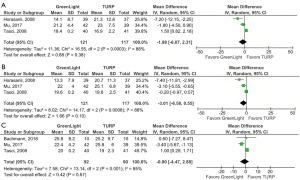
Regarding the secondary outcomes, no notable distinctions were observed in the Qmáx rate in any of the periods analyzed, 3 months (MD −1.88; 95% CI: −6.07 to 2.31; P=0.38; I2=88%) (Figure 3A), 6 months (MD −3.01; 95% CI: −6.58 to 0.55; P=0.10; I2=86%) (Figure 3B), 12 months (MD −0.80; 95% CI: −4.47 to 2.88; P=0.67; I2=85%) (Figure 3C); nor were significant the Vres values obtained, 3 months (MD 19.19; 95% CI: −5.57 to 43.96; P=0.13; I2=96%) (Figure 4A), 6 months (MD 17.51; 95% CI: −8.92 to 43.94; P=0.19; I2=94%) (Figure 4B), 12 months (MD 1.09; 95% CI: −0.91 to 3.10; P=0.29; I2=0%) (Figure 4C).
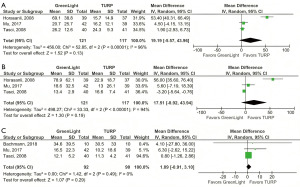
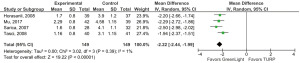
At the same time, we could see a reduced operative time in TURP branch (MD 30.35; 95% CI: 11.26 to 49.44; P=0.002; I2=96%) (Figure 5), while the catheterization time (MD −2.22; 95% CI: −2.44 to −1.99; P<0.001; I2=1%) (Figure 6) and the postoperative hospital stay (MD −2.20; 95% CI: −2.69 to −1.72; P<0.001; I2=75%) (Figure 7) were lower in patients who underwent GreenLight.
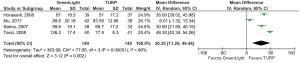

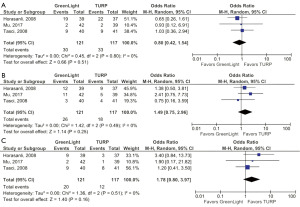
Regarding the postoperative complications, no differences were seen between groups in CD1 (OR 0.80; 95% CI: 0.42 to 1.54; P=0.51; I2=0%), CD2 (OR 1.49; 95% CI: 0.75 to 2.96; P=0.25; I2=0%) or CD3 (OR 1.78; 95% CI: 0.80 to 3.97; P=0.16; I2=0%) grades (Figure 8A-8C, respectively). As a matter of fact, no study included presented patients with complications graded as CD4.
We should point that our primary endpoint, IPSS, included data from all the included studies except for Sarica et al. As for the secondary endpoints, the Qmáx rate and the mean Vres were again not assessed in Sarica trial; operative time, catheterization time and postoperative hospital stay included all, with the exception of the Bachmann cohort; and finally, the complications were assessed only in Horasanli, Mu and Tasci cohorts.
Quality assessment
The two non-RCT studies were assessed by ROBINS-I score, and while Mu et al. (12) presented a low risk, the work conducted by Tasci et al. (13) showed a high risk of bias, primarily due to bias in selection of participants into the study (Figure 9A). On the other hand, the 3 RCT trials here included were assessed by Rob-2 tool. The cohort from Horasanli (14) presented a low overall score of bias, while the Sarica (15) and Bachmann (16) trials showed a high risk of bias (Figure 9B). This bias is mainly due to missing outcome data since both studies are conference abstracts.

Discussion
Our meta-analysis comparing GreenLight PVP versus TURP in male BPH patients with large prostates revealed no significant differences in key efficacy parameters, including IPSS, Qmáx, and Vres. Despite a longer operative time for PVP, it demonstrated advantages in lower catheterization time and postoperative hospital stay. No disparities in complication rates (CD1, CD2, CD3) were observed between the two procedures.
As previously mentioned, current guidelines maintain reservations regarding the widespread adoption of PVP. The AUA, for instance, recommends, with an evidence level B, considering PVP as an option using 120 or 180 W platforms for the treatment of LUTS or BPH (4). Nevertheless, they express skepticism about the effectiveness of PVP compared to TURP for large prostates (≥70 mL), primarily citing studies indicating a higher retreatment rate for PVP than TURP (17). In contrast, the EAU supports the comparable improvements in symptom scores and urinary flow achieved by PVP over the years in comparison to TURP. Despite endorsing PVP for patients on anticoagulants and those desiring to preserve ejaculation, surgeons are hesitant to recommend this technique broadly due to lingering concerns about the unknown long-term effects of laser surgery (3).
Regarding our primary outcome of interest, the IPSS score revealed no significant differences at 3, 6, or 12 months post-intervention between PVP and TURP. This suggests a non-inferiority of PVP compared to TURP, the established treatment for BPH. Notably, these results were unexpected, as initial use of PVP was associated with more common storage symptoms during the early postoperative period (18). However, recent studies highlight independent predictors of storage symptoms, such as advanced age, baseline symptom severity, and prolonged operative time (19,20). Furthermore, storage symptoms are anticipated to continuously improve up to the 12-month follow-up (21).
Concerning operative time, our analysis indicated a longer total operative time with the GreenLight approach, differing by approximately 30 minutes compared to TURP. This disparity is likely attributable to the prolonged time required for tissue vaporization in PVP compared to the removal of excess prostate tissue in TURP. Additionally, both catheterization time and postoperative hospital stay were shorter in PVP, attributed to reduce bleeding during prostate tissue vaporization. The instant absorption of laser light by the blood facilitates quick vaporization and removal, resulting in minimal blood loss, reduced postoperative discomfort, and a shorter hospital stay (22,23).
Qmáx and Vres rates were evaluated between both groups, but no statistically significant differences were observed in either outcome. This lack of significance suggests the non-inferiority of neither technique evaluated in this study.
Comparing complications by magnitude, the PVP group exhibited 24.7% CD1, 21.5% CD2, and 16.5% CD3, while the TURP group displayed 28.2% CD1, 15.3% CD2, and 10.2% CD3. Notably, no statistical differences were found when comparing CD1, CD2, and CD3 overall. These results underscore the comparable safety profiles of both PVP and TURP, reinforcing the notion that neither procedure significantly outperforms the other in terms of complication rates.
In general, the primary distinctions between TURP and PVP revolve around TURP’s status as a more established technique, having predated PVP, and being considered the gold standard for BPH treatment. TURP offers the advantage of providing anatomical-pathological specimens, enabling the straightforward diagnosis of additional conditions such as prostate cancer (4). However, PVP gains prominence in endourological surgery by ensuring minimal blood loss through the vaporization of prostate tissue, and it avoids causing hyponatremia, even with an extended operative time. Additionally, from an economic standpoint, while TURP is presently a more cost-effective option, the increasing adoption of newer urological techniques, including PVP and Holmium laser enucleation of the prostate (HoLEP) surgery, may make laser devices more attractive for the next generation of urologists (24).
The efficacy comparison between PVP and TURP has been explored by other authors, though none have specifically assessed large prostates as in the present study. For example, Lai et al. (6) conducted a meta-analysis involving 2,665 patients assessing PVP versus TURP in BPH patients. While no significant differences were found in IPSS, Qmáx, and Vres, PVP exhibited a longer operative time, shorter catheterization time, and reduced complications, including bleeding, urethral strictures, urinary incontinence, and transurethral resection syndrome, when compared to TURP. Another meta-analysis by Ding et al. (5), involving 1,398 patients, demonstrated less morbidity, increased operative time, and a shorter hospital stay in the PVP group, particularly in the analysis of small prostates (<70 mL). These results align with and substantiate the findings presented above, reinforcing the consistent trends observed in the comparative efficacy of PVP and TURP across various studies.
Highlighting the ongoing evolution of lasers in endourology is crucial. Historically, lasers operated at lower power settings (34 W), but as techniques evolved and research expanded, power settings increased to around 80 to 120 W for prostate vaporization (25). The safety of laser use hinges on proper training, and precautions are imperative to prevent adverse events for both patients and operators (26). Furthermore, the continuous advancements in laser technology may impact the analyzed outcomes (IPSS, Qmáx, and Vres) in the future, underlining the dynamic nature of this field.
Our study has notable limitations. Firstly, the small patient sample was influenced by the limited number of studies evaluating these procedures in patients with large prostates (≥70 mL). Secondly, due to the scarcity of literature on this topic, the five studies varied in design, ranging from RCTs to non-RCTs, potentially limiting the generalizability of meta-analysis results. Two of the included studies, specifically Sarica et al.’s and Bachmann et al.’s studies, were conference abstracts, which constrained our analysis and information extraction. Thirdly, our study presented an increased risk of bias primarily due to the inclusion of two conference abstract trials since bias regarding missing outcome data was detected in Sarica and Bachmann trials. Fourthly, the absence of a formal cost-effective analysis contributes to the study’s limitations, as choosing PVP over TURP currently represents a higher economic burden. Fifthly, our findings are subject to the evolving landscape of urologic techniques. Notably, emerging alternatives like HoLEP and Thulium laser enucleation of the prostate (ThuLEP) are challenging the established gold standard, showing comparable efficacy to TURP and the ability to address prostates of nearly any size.
Addressing open questions in the literature, direct comparisons of GreenLight PVP versus TURP versus HoLEP and assessments in higher cohorts are essential. Evaluating not only the effectiveness but also the economic viability of these techniques for each case would provide comprehensive insights. Looking ahead, future research on PVP, particularly through RCTs, holds promise. Whether due to the cost-effectiveness of this technique, which is still inaccessible in many centers, or improved surgeon training with this equipment, such investigations could yield more promising results and contribute significantly to refining treatment strategies for BPH.
Conclusions
In summary, our meta-analysis comparing GreenLight PVP and TURP in BPH patients with large prostates (≥70 mL) indicates non-inferiority efficacy of PVP, particularly in post-surgical parameters (IPSS, Qmáx, and Vres). While a complete significant analysis was not achieved, PVP showed improved efficacy over the benchmark TURP, with added benefits such as shorter hospital stay and catheterization time, potentially enhancing patient compliance and satisfaction.
Given the limited patient sample, further research and larger-scale RCTs are needed to validate and build upon these findings, contributing to the development of more robust BPH treatment guidelines.
Acknowledgments
The abstract has been presented as a poster in the International Student Congress of (Bio) Medical Sciences (2024), the 41st World Congress of Endourology and Uro-Technology (2024), the Congresso Médico Universitário da Faculdade de Medicina da USP (2024), and the XVIII Congresso Paulista de Urologia (2024) .
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-2025-111/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-2025-111/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-2025-111/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Langan RC. Benign Prostatic Hyperplasia. Prim Care 2019;46:223-32. [Crossref] [PubMed]
- Devlin CM, Simms MS, Maitland NJ. Benign prostatic hyperplasia - what do we know? BJU Int 2021;127:389-99. [Crossref] [PubMed]
- de la Rosette JJ, Alivizatos G, Madersbacher S, et al. EAU Guidelines on benign prostatic hyperplasia (BPH). Eur Urol 2001;40:256-63; discussion 264. [Crossref] [PubMed]
- Sandhu JS, Bixler BR, Dahm P, et al. Management of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia (BPH): AUA Guideline Amendment 2023. J Urol 2024;211:11-9. [Crossref] [PubMed]
- Ding H, Du W, Lu ZP, et al. Photoselective green-light laser vaporisation vs. TURP for BPH: meta-analysis. Asian J Androl 2012;14:720-5. [Crossref] [PubMed]
- Lai S, Peng P, Diao T, et al. Comparison of photoselective green light laser vaporisation versus traditional transurethral resection for benign prostate hyperplasia: an updated systematic review and meta-analysis of randomised controlled trials and prospective studies. BMJ Open 2019;9:e028855. [Crossref] [PubMed]
- Reich O, Gratzke C, Bachmann A, et al. Morbidity, mortality and early outcome of transurethral resection of the prostate: a prospective multicenter evaluation of 10,654 patients. J Urol 2008;180:246-9. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. PLoS Med 2021;18:e1003583. [Crossref] [PubMed]
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:l4898. [Crossref] [PubMed]
- Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355:i4919. [Crossref] [PubMed]
- Mu XN, Wang SJ, Chen J, et al. Bipolar transurethral enucleation of prostate versus photoselective vaporization for symptomatic benign prostatic hyperplasia (>70 ml). Asian J Androl 2017;19:608-12. [Crossref] [PubMed]
- Tasci AI, Tugcu V, Sahin S, et al. Photoselective vaporization of the prostate versus transurethral resection of the prostate for the large prostate: a prospective nonrandomized bicenter trial with 2-year follow-up. J Endourol 2008;22:347-53. eng. [Crossref] [PubMed]
- Horasanli K, Silay MS, Altay B, et al. Photoselective potassium titanyl phosphate (KTP) laser vaporization versus transurethral resection of the prostate for prostates larger than 70 mL: a short-term prospective randomized trial. Urology 2008;71:247-51. [Crossref] [PubMed]
- Sarica K. Photoselective vaporization (PVP) versus transurethral resection of the prostate (TURP) for prostates >80g: a prospective randomized trial. Eur Urol Suppl 2007;6:163. [Crossref]
- Bachmann A, Tubaro A, Barber N, et al. Greenlight (GL) 180-W XPS PVP and transurethral resection of the prostate (the Goliath study): one year follow-up by prostate size. J Urol 2014;191:e796. [Crossref]
- Elshal AM, Soltan M, El-Tabey NA, et al. Randomised trial of bipolar resection vs holmium laser enucleation vs Greenlight laser vapo-enucleation of the prostate for treatment of large benign prostate obstruction: 3-years outcomes. BJU Int 2020;126:731-8. [Crossref] [PubMed]
- Al-Ansari A, Younes N, Sampige VP, et al. GreenLight HPS 120-W laser vaporization versus transurethral resection of the prostate for treatment of benign prostatic hyperplasia: a randomized clinical trial with midterm follow-up. Eur Urol 2010;58:349-55. [Crossref] [PubMed]
- Song WH, Park J, Cho SY, et al. Predictors of Improvement in Storage Symptoms at Three Years After 120W GreenLight High Performance System Laser Treatment for Benign Prostate Hyperplasia. J Endourol 2017;31:666-73. [Crossref] [PubMed]
- Elkoushy MA, Elshal AM, Elhilali MM. Postoperative Lower Urinary Tract Storage Symptoms: Does Prostate Enucleation Differ from Prostate Vaporization for Treatment of Symptomatic Benign Prostatic Hyperplasia? J Endourol 2015;29:1159-65. [Crossref] [PubMed]
- De Nunzio C, Miano R, Trucchi A, et al. Photoselective prostatic vaporization for bladder outlet obstruction: 12-month evaluation of storage and voiding symptoms. J Urol 2010;183:1098-103. [Crossref] [PubMed]
- Kirby R. GreenLight photoselective vaporisation of the prostate. Prostate Cancer Prostatic Dis 2007;10:S1. [Crossref]
- Stafinski T, Menon D, Harris K, et al. Photoselective vaporization of the prostate for the treatment of benign prostatic hyperplasia. Can Urol Assoc J 2008;2:124-34. [PubMed]
- Pirola GM, Maggi M, Castellani D, et al. A Cost-Benefit Analysis of Bipolar TURP for the Treatment of Bladder Outflow Obstruction. Res Rep Urol 2021;13:487-94. [Crossref] [PubMed]
- Zarrabi A, Gross AJ. The evolution of lasers in urology. Ther Adv Urol 2011;3:81-9. [Crossref] [PubMed]
- Pietropaolo A, Mani M, Hughes T, et al. Role of low- versus high-power laser in the treatment of lower pole stones: prospective non-randomized outcomes from a university teaching hospital. Ther Adv Urol 2022;14:17562872221097345. [Crossref] [PubMed]



