
Global epidemiological trends in prostate cancer burden: a comprehensive analysis from Global Burden of Disease Study 2021
Highlight box
Key findings
• Prostate cancer incidence increased by 161.53%, while mortality declined by 0.83%, reflecting improved treatment, but persistent late-stage diagnoses in low-socio-demographic index (SDI) regions.
• Age 70+ years group (individuals aged 70 years and older): accounted for 68% of disability-adjusted life years, underscoring the disease’s association with aging populations.
• Countries like Bermuda, Antigua, and Barbuda exhibited significant intra-regional inequalities despite high SDI.
What is known and what is new?
• SDI is inversely correlated with mortality-to-incidence ratios, as seen in prior Global Burden of Disease studies.
• High-income inequities: revealed unexpected disparities in high-SDI nations, where marginalized subgroups face barriers to advanced therapies.
What is the implication, and what should change now?
• The findings highlight the need for precision public health strategies to address regional disparities and improve outcomes, particularly in aging populations.
• Economic development alone is insufficient to reduce disability burden, emphasizing the importance of targeted interventions in high-burden regions.
Introduction
Prostate cancer (PC) is one of the most common malignancies among men worldwide. The disease ranked second among common men cancers after lung cancer and accounted for 14.1% of newly diagnosed cancers in men globally (1-4). As a leading cause of cancer-related morbidity and mortality, PC presents a major public health challenge, particularly as global populations age (5,6). The disease’s burden is characterized not only by its rising incidence but also by substantial geographic and socio-demographic disparities in its impact. Furthermore, the global incidence and mortality rates of PC exhibit substantial variations across ethnic and geographic populations. The disease is significantly more prevalent in high-income regions, such as North America, Western and Northern Europe, and Australia, where a higher Human Development Index (HDI) and gross domestic product contribute to increased life expectancy and greater access to diagnostic services (3). Notably, men of African descent, including those from Afro-Caribbean, sub-Saharan African, and African American populations, experience the highest PC mortality rates, underscoring potential disparities in genetic susceptibility, healthcare access, and disease management (7). These disparities are influenced by factors such as access to healthcare, early detection programs, and treatment effectiveness, as well as regional differences in lifestyle and environmental exposures.
In 2001, the Urologic Diseases in America project was initiated to systematically assess the burden of urologic diseases in the United States, encompassing both their medical and economic impact (8,9). More recently, the Global Burden of Disease (GBD) studies have provided extensive epidemiological data on the global burden of these conditions, serving as a crucial foundation for evidence-based health policy development and resource allocation (10). PC imposes a significant burden on patients, families, and society, necessitating substantial medical care, financial resources, and caregiving efforts. However, an updated assessment of its global, regional, and national impact is still needed. This study utilizes data from the GBD study, a comprehensive international effort that synthesizes epidemiological data from 204 countries and territories to evaluate health losses across 328 diseases (11). By analyzing key indicators such as incidence, prevalence, mortality, and disability-adjusted life years (DALYs), this study aims to provide a detailed understanding of PC trends. Special attention is given to temporal and geographical variations, as well as age-related patterns, particularly in regions with aging populations where the disease burden is rising. These insights will help inform healthcare strategies and policy decisions aiming at mitigating the impact of PC worldwide. In addition to global and regional disparities, socio-demographic factors, such as income levels and healthcare infrastructure (12,13), contribute to the uneven distribution of PC burden. High-income regions, with their advanced healthcare systems, generally exhibit higher rates of diagnosis and treatment (14,15), which may explain the higher prevalence observed in these areas. However, this also highlights the significant challenges faced by low- and middle-income regions, where limited access to healthcare and early detection programs exacerbate the disease burden.
The objective of this study is to examine the trends in PC incidence, prevalence, mortality, and DALYs between 1990 and 2021, using GBD Study 2021 data. By analyzing the relationship between these trends and socio-demographic factors, such as the socio-demographic index (SDI), we aim to provide insights into the factors driving the global PC burden. Additionally, the study explores the regional differences and gender-specific trends in PC burden, with an emphasis on regions with the highest burden. The findings of this study will help inform the development of targeted public health interventions and strategies aiming at reducing the global impact of PC.
Methods
Data collection
We extracted annual data on incident cases, deaths, DALYs, age-standardized incidence rates (ASIRs), age-standardized death rates (ASDRs), and age-standardized prevalence rates (ASPRs) for PC from 1990 to 2019 using the Global Health Data Exchange (GHDx) query tool (http://ghdx.healthdata.org/gbd-results-tool). This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The analyses were based on publicly available, de-identified data from the GBD Study 2021, which does not require ethical approval. The dataset encompasses 204 countries and territories, which are classified into five SDI regions and 21 GBD geographical regions. The methodology for the GBD Study 2021 is described in detail elsewhere. Briefly, incidence estimates were generated using DisMod-MR 2.1, a Bayesian meta-regression tool that synthesizes heterogeneous epidemiological data through a compartmental model structure. Mortality estimates were derived using the Cause of Death Ensemble Modeling (CODEm) approach, which selects models and covariates based on out-of-sample predictive performance. DALYs were calculated as the sum of years of life lost (YLLs) due to premature death and years lived with disability (YLDs).
Frontier analysis
To explore the relationship between the burden of PC and sociodemographic development, we applied frontier analysis, a quantitative method designed to estimate the lowest theoretically achievable age-standardized DALYs rate based on SDI. Statistical analyses were conducted using SAS Enterprise Guide 7.1, while geographic distributions were visualized with ArcGIS 10.5.1 (ESRI, Redlands, CA, USA).
Joinpoint regression analysis
Joinpoint regression modeling was employed to quantify temporal trends in ASIR, ASDR, ASPR, and DALYs for PC cancers from 1990 to 2021 at the global level. The model identifies significant inflection points where the trend changes, utilizing a least squares regression approach to minimize subjectivity. The optimal number and location of joinpoints were determined by minimizing the sum of squared residuals between observed and estimated values. The analysis was performed using Joinpoint software (version 4.9.1.0), which applies a piecewise linear regression model to detect statistically significant trend shifts.
In addition to the disease burden metrics, socioeconomic data, including the SDI and the Universal Health Coverage Index (UHCI) for 2021, were obtained from the GHDx database. The SDI is a composite measure of development status, strongly correlated with health outcomes. It is calculated as the geometric mean of three indicators: lag-distributed income per capita, average years of schooling for individuals aged 15 and older, and the total fertility rate for women under age 25 years. An SDI value of 0 represents the lowest theoretical level of development, while a value of 1 indicates the highest possible level.
Statistical analysis
To evaluate regional and temporal variations in the burden of PC cancer, we calculated age-standardized rates (ASRs) and estimated annual percentage changes (EAPCs). Given the necessity of standardization for cross-population and longitudinal comparisons, the ASIR and ASDR were computed per 100,000 population using the following formula:
where αk represents the weight of the reference population in age group k, and βk denotes the corresponding age-specific rate.
To quantify ASR trends over time, we derived EAPC along with 95% confidence intervals (CIs) using log-linear regression:
where y represents the natural logarithm of ASR, x denotes the calendar year, and β is the estimated trend coefficient. An increasing trend was indicated when the lower bound of the CI exceeded 0, while a decreasing trend was signified when the upper bound was below 0.
Results
Global trends in urological cancers mortality and incidence
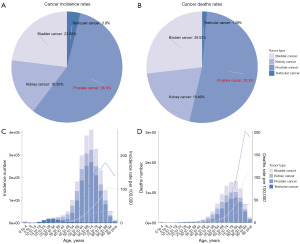
Our analysis of 2021 global cancer incidence and mortality data underscored the significant burden of PC (Figure 1), which accounted for the largest proportion of cases (56.5%) and deaths (52.3%) among the four major urologic cancers (Figure 1A,1B). In comparison, bladder cancer represented 23.1% of cases and 26.8% of deaths, kidney cancer accounted for 16.6% of cases and 19.5% of deaths, and testicular cancer comprised 3.9% of cases and 1.4% of deaths. This highlighted the disproportionately high impact of PC on cancer-related mortality worldwide, making it a critical area of focus for future research and healthcare strategies. Additionally, PC incidence and mortality exhibited a clear age-related trend. Both incidence rates and total cases increased progressively with age, peaking between 60 and 74 years, with incidence rates ranging from 23.3 to 50 per 100,000 male population. The highest average incidence rate of PC occurred in the 60–64 years age group, with 74,592 total cases, and continued to rise in older age groups, reaching 66.9 in the 80–84 years age group, which had 58,632 total cases (Figure 1C). Mortality rates of PC also increased with age, with the highest death rate of 85.8 observed in the 90–94 years age group, accompanied by 15,354 total deaths, and a close second in the 95+ years age group (85.5, 4,661 deaths). In the 70–74 years age group, both incidence (50.0) and total number of cases [102,830] rose notably, along with an increase in mortality (14.7) and total deaths [30,343] (Figure 1D). These findings emphasized the importance of focusing on PC in the context of aging populations, given its high incidence and mortality rates in older age groups.
Age-related burden and global temporal trends in PC: insights from 1990 to 2021
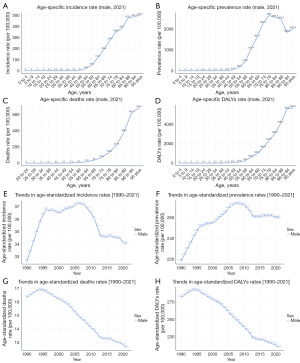
In 2021, individuals aged 70 years and above (70+ years age group) accounted for 86.58% of the incidence (Figure 2A), 80.64% of the prevalence (Figure 2B), 97.13% of mortality (Figure 2C), and 91.86% of DALYs (Figure 2D). The incidence and mortality rates peaked in the 75–79 years age group, whereas DALYs and prevalence showed a significant increase among those aged 80 years and older. Between 1990 and 2021, the ASIRs demonstrated a marginal annual percentage change (APC) of 0.14%, showing a non-significant upward trend (P=0.36) (Figure 2E), indicating that the incidence rate remained relatively stable during the study period. Conversely, the prevalence rate showed a significant increase (R2=0.49, P<0.001) with an APC of 0.57% (Figure 2F), reflecting extended survival times likely driven by advancements in early diagnosis and treatment. Notably, DALYs and mortality rates experienced significant declines, with APCs of −0.75% and −0.83% (Figure 2G,2H), respectively (both R2=0.94, P<0.001). These reductions indicate substantial progress in mitigating health losses and reducing mortality associated with PC, likely attributable to improved treatment efficacy and enhanced disease management.
Regional disparities in PC burden [1990–2021]
Between 1990 and 2021, the EAPC in the ASIR, ASPR, DALYs, and ASDR for PC exhibited significant regional and sex-based variations (Figure 3 and Table 1). Eastern Europe consistently demonstrated the highest EAPC values across all indicators, with the ASIR EAPC reaching 3.27 in males and the highest ASPR EAPC observed in North Africa and the Middle East (3.86). In contrast, high-income North America recorded the lowest EAPC values for ASIR and ASPR, at −1.25 and −0.856, respectively (Figure 3A,3B and Figure S1A,S1B). For DALYs and ASDR, Australasia exhibited the most pronounced decline, with the lowest EAPC values of −2.67 and −2.74, respectively (Figure 3C,3D and Figure S1C,S1D). Moreover, we employed Pearson correlation analysis to examine the relationship between EAPC and SDI across four key indicators: incidence, prevalence, mortality, and DALYs. The results showed weak negative correlations for incidence (r=−0.046) and prevalence (r=−0.092), while stronger negative correlations were observed for mortality (r=−0.436) and DALYs (r=−0.419) (Figure S2). These findings suggest that regions with higher SDI tend to exhibit lower EAPC values for mortality and DALYs, indicating a potentially greater reduction in disease burden over time.
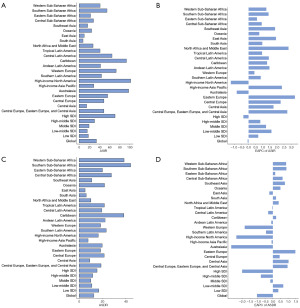
Table 1
| Location | ASIR | ASDR | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Num_1990 (95% CI) | ASIR_1990 (95% CI) | Num_2021 (95% CI) | ASIR_2021 (95% CI) | Num_change (95% CI) (%) | EAPC_CI (95% CI) (%) | Num_1990 (95% CI) | ASDR_1990 (95% CI) | Num_2021 (95% CI) | ASDR_2021 (95% CI) | Num_change (95% CI) (%) | EAPC_CI (95% CI) (%) | ||
| Global | 506,405 (480,851 to 524,697) | (30.86 to 33.86) | 1,324,383 (1,217,321 to 1,400,222) | 34.05 (31.27 to 36.00) | 161.53 (153.16 to 166.86) | −0.06 (−0.2 to 0.08) | 211,972 (194,222 to 224,328) | (15.02 to 17.28) | 432,463 (381,873 to 463,645) | 12.63 (11.16 to 13.55) | 104.02 (96.62 to 106.68) | −1.05 (−1.14 to −0.95) | |
| High SDI | 339,224 (324,610 to 348,526) | (70.21 to 75.85) | 694,561 (647,353 to 727,638) | 70.92 (66.29 to 74.22) | 104.75 (99.42 to 108.78) | −0.36 (−0.52 to −0.21) | 105,149 (99,286 to 108,363) | (24.06 to 26.61) | 154,423 (138,844 to 163,655) | 15.35 (13.8 to 16.27) | 46.86 (39.84 to 51.02) | −2.02 (−2.14 to −1.91) | |
| High-middle SDI | 83,918 (79,122 to 87,907) | (21.31 to 23.86) | 268,333 (238,028 to 291,706) | 30.36 (26.96 to 33.04) | 219.75 (200.84 to 231.84) | 0.83 (0.63 to 1.03) | 43,452 (40,562 to 45,902) | (13.2 to 15.09) | 90,323 (79,773 to 98,854) | 11.73 (10.33 to 12.86) | 107.87 (96.67 to 115.36) | −0.79 (−0.97 to −0.62) | |
| Middle SDI | 46,618 (39,994 to 51,526) | (10.8 to 13.93) | 228,112 (194,580 to 258,723) | 19.43 (16.51 to 22.07) | 389.32 (386.52 to 402.12) | 1.23 (1.05 to 1.41) | 31,439 (26,222 to 35,880) | (8.57 to 11.64) | 99,769 (82,565 to 115,535) | 10.03 (8.30 to 11.6) | 217.34 (214.87 to 222.01) | −0.17 (−0.35 to 0.01) | |
| Low-middle SDI | 23,185 (18,103 to 26,835) | (7.46 to 11.07) | 95,746 (79,599 to 111,125) | 15.90 (13.29 to 18.51) | 312.97 (339.7 to 314.11) | 1.61 (1.48 to 1.74) | 19,448 (14,791 to 22,961) | (6.78 to 10.39) | 57,756 (46,941 to 68,429) | 10.92 (9.02 to 12.93) | 196.98 (217.37 to 198.02) | 0.68 (0.55 to 0.81) | |
| Low SDI | 12,828 (8,389 to 16,190) | (9.59 to 18.27) | 35,707 (23,034 to 44,175) | 18.14 (11.84 to 22.34) | 178.36 (174.58 to 172.85) | 0.69 (0.62 to 0.75) | 12,124 (7,907 to 15,319) | (9.92 to 19) | 29,431 (18,998 to 36,227) | 16.8 (10.86 to 20.59) | 142.75 (140.26 to 136.49) | 0.36 (0.29 to 0.42) | |
| Andean Latin America | 2,234 (1,801 to 2,784) | (21.28 to 32.23) | 11,257 (8,196 to 15,488) | 42.16 (30.78 to 57.66) | 403.98 (355.18 to 456.23) | 1.47 (1.33 to 1.62) | 1,839 (1,503 to 2,258) | (18.8 to 27.69) | 5,632 (4,181 to 7,475) | 22.26 (16.58 to 29.52) | 206.18 (178.21 to 231.06) | −0.11 (−0.25 to 0.04) | |
| Australasia | 11,155 (10,153 to 11,895) | (100.67 to 117.87) | 25,373 (21,471 to 29,884) | 97.88 (82.70 to 115.15) | 127.46 (111.47 to 151.24) | −0.83 (−1.47 to −0.19) | 3,641 (3,317 to 3,843) | (36.91 to 43.16) | 5,314 (4,491 to 6,099) | 19.76 (16.71 to 22.7) | 45.96 (35.40 to 58.71) | −2.74 (−3.06 to −2.43) | |
| Caribbean | 7,122 (6,577 to 7,884) | (55.66 to 66.69) | 23,251 (19,899 to 26,780) | 93.77 (80.45 to 108.03) | 226.45 (202.54 to 239.66) | 1.3 (1.11 to 1.5) | 3,779 (3,479 to 4,245) | (32.02 to 39.05) | 9,258 (7,967 to 10,783) | 38.35 (32.98 to 44.63) | 144.99 (128.99 to 154.03) | 0.21 (0.05 to 0.38) | |
| Central Asia | 1,859 (1,733 to 1,976) | (10.46 to 11.95) | 4,640 (4,157 to 5,157) | 14.9 (13.51 to 16.48) | 149.62 (139.91 to 160.93) | 1.76 (1.43 to 2.09) | 1,268 (1,180 to 1,346) | (7.84 to 8.97) | 2,405 (2,183 to 2,652) | 9.12 (8.32 to 10.01) | 89.74 (84.98 to 97.05) | 1.03 (0.75 to 1.31) | |
| Central Europe | 14,514 (13,747 to 15,354) | (23.35 to 26.18) | 47,883 (43,406 to 52,544) | 48.9 (44.40 to 53.65) | 229.9 (215.75 to 242.23) | 2.27 (2.04 to 2.49) | 9,399 (8,918 to 10,003) | (16.69 to 18.84) | 19,779 (18,084 to 21,356) | 21.49 (19.56 to 23.19) | 110.44 (102.79 to 113.49) | 0.45 (0.25 to 0.64) | |
| Central Latin America | 12,882 (12,256 to 13,391) | (34.18 to 37.51) | 72,325 (62,261 to 83,103) | 65.04 (56.10 to 74.53) | 461.43 (408.01 to 520.6) | 1.43 (1.1 to 1.76) | 6,188 (5,851 to 6,434) | (18.1 to 20.11) | 20,037 (17,440 to 22,606) | 19.52 (17.03 to 21.95) | 223.79 (198.09 to 251.36) | −0.31 (−0.54 to −0.09) | |
| Central sub-Saharan Africa | 1,504 (965 to 1,987) | (13.81 to 28.59) | 4,528 (2,737 to 6,191) | 28.26 (17.17 to 39.13) | 201 (183.53 to 211.65) | 0.93 (0.77 to 1.09) | 1,449 (939 to 1,937) | (14.74 to 31.44) | 3,722 (2,246 to 5,110) | 27.7 (16.75 to 38.72) | 156.96 (139.11 to 163.76) | 0.64 (0.51 to 0.77) | |
| East Asia | 14,814 (11,139 to 18,813) | (3.93 to 6.62) | 97,024 (71,372 to 129,638) | 9.90 (7.39 to 13.06) | 554.95 (540.73 to 589.1) | 1.93 (1.78 to 2.09) | 11,218 (8,527 to 14,514) | (3.73 to 6.48) | 39,955 (30,356 to 53,029) | 5.05 (3.80 to 6.62) | 256.16 (256.00 to 265.36) | −0.24 (−0.46 to −0.01) | |
| Eastern Europe | 20,795 (19,663 to 21,764) | (21.55 to 23.82) | 76,061 (68,014 to 83,466) | 56.28 (50.56 to 61.65) | 265.77 (245.89 to 283.51) | 3.27 (3.08 to 3.47) | 9,430 (8,926 to 9,818) | (11.45 to 12.67) | 22,103 (19,833 to 24,513) | 18.39 (16.54 to 20.34) | 134.39 (122.19 to 149.69) | 1.48 (1.39 to 1.57) | |
| Eastern sub-Saharan Africa | 5,387 (3,232 to 6,870) | (11.12 to 23.18) | 14,544 (9,313 to 18,607) | 22.55 (14.67 to 28.24) | 169.97 (188.15 to 170.82) | 0.59 (0.54 to 0.65) | 5,035 (3,042 to 6,387) | (11.43 to 23.73) | 11,477 (7,401 to 14,590) | 20 (13.03 to 25.16) | 127.96 (143.32 to 128.43) | 0.15 (0.12 to 0.19) | |
| High-income Asia Pacific | 10,827 (10,155 to 11,450) | (13.61 to 15.46) | 65,589 (57,663 to 72,526) | 28.74 (25.29 to 31.7) | 505.79 (467.83 to 533.41) | 2.35 (1.83 to 2.87) | 4,841 (4,547 to 5,100) | (6.58 to 7.47) | 18,864 (16,674 to 20,318) | 7.65 (6.80 to 8.23) | 289.65 (266.73 to 298.36) | −0.09 (−0.37 to 0.2) | |
| High-income North America | 198,196 (189,549 to 204,981) | (124.25 to 134.72) | 316,171 (297,652 to 329,966) | 101.92 (95.89 to 106.4) | 59.52 (57.03 to 60.97) | −1.25 (−1.38 to −1.12) | 41,725 (39,200 to 43,302) | (27.8 to 31.16) | 49,580 (44,576 to 52,487) | 16.43 (14.70 to 17.43) | 18.83 (13.71 to 21.21) | −2.4 (−2.55 to −2.26) | |
| North Africa and Middle East | 8,445 (6,245 to 10,445) | (9.1 to 15.41) | 55,934 (39,217 to 67,925) | 27.39 (19.27 to 33.39) | 562.32 (527.96 to 550.29) | 2.81 (2.72 to 2.91) | 5,196 (3,874 to 6,602) | (6.62 to 11.58) | 16,720 (11,802 to 20,203) | 10.05 (7.09 to 12.18) | 221.81 (204.68 to 206.02) | 0.38 (0.3 to 0.46) | |
| Oceania | 198 (137 to 271) | (13.9 to 27.26) | 670 (427 to 931) | 24.56 (15.95 to 34.27) | 237.97 (212.12 to 243.22) | 0.76 (0.72 to 0.8) | 162 (111 to 224) | (13.29 to 26.87) | 507 (321 to 719) | 21.76 (13.86 to 30.59) | 212.48 (188.42 to 221.43) | 0.5 (0.44 to 0.55) | |
| South Asia | 11,974 (8,454 to 14,641) | (3.63 to 6.31) | 48,150 (39,400 to 65,765) | 7.60 (6.26 to 10.42) | 302.12 (366.03 to 349.17) | 0.97 (0.83 to 1.12) | 11,086 (7,835 to 13,661) | (3.69 to 6.42) | 34,073 (28,061 to 46,489) | 6.03 (4.98 to 8.26) | 207.36 (258.16 to 240.3) | 0.21 (0.07 to 0.35) | |
| Southeast Asia | 8,733 (6,067 to 10,199) | (6.59 to 11.07) | 43,150 (28,221 to 53,091) | 16.72 (10.97 to 20.71) | 394.13 (365.18 to 420.57) | 1.87 (1.81 to 1.93) | 7,107 (4,948 to 8,378) | (6.03 to 10.11) | 24,286 (15,953 to 29,602) | 10.86 (7.10 to 13.36) | 241.71 (222.45 to 253.34) | 0.79 (0.71 to 0.88) | |
| Southern Latin America | 6,297 (5,629 to 7,020) | (29.78 to 37.11) | 16,821 (14,362 to 19,465) | 44.06 (37.83 to 50.95) | 167.14 (155.16 to 177.26) | 0.86 (0.48 to 1.24) | 4,685 (4,226 to 5,209) | (24.27 to 29.84) | 8,446 (7,276 to 9,581) | 23.26 (20.04 to 26.33) | 80.26 (72.18 to 83.93) | −0.45 (−0.78 to −0.13) | |
| Southern sub-Saharan Africa | 3,428 (2,471 to 4,573) | (26.81 to 48.8) | 10,873 (8,115 to 12,871) | 55.12 (40.52 to 64.65) | 217.17 (181.45 to 228.36) | 1.41 (1.27 to 1.55) | 2,964 (2,165 to 3,918) | (26.02 to 46.01) | 7,418 (5,391 to 8,681) | 44.25 (31.48 to 51.79) | 150.30 (148.97 to 121.57) | 0.89 (0.69 to 1.09) | |
| Tropical Latin America | 10,380 (9,809 to 10,873) | (26.85 to 30.11) | 45,434 (42,311 to 48,150) | 41.32 (38.45 to 43.85) | 337.71 (331.34 to 342.83) | 0.95 (0.6 to 1.31) | 6,897 (6,497 to 7,214) | (20.13 to 22.69) | 21,747 (19,995 to 23,132) | 21.62 (19.72 to 23.06) | 215.33 (207.77 to 220.65) | −0.03 (−0.36 to 0.3) | |
| Western Europe | 145,847 (138,955 to 151,805) | (58.11 to 63.5) | 314,970 (285,543 to 338,632) | 73.05 (66.40 to 78.43) | 115.96 (105.49 to 123.07) | 0.41 (0.08 to 0.75) | 64,658 (61,244 to 67,382) | (27.81 to 30.88) | 86,450 (76,255 to 93,367) | 18.36 (16.26 to 19.81) | 33.7 (24.51 to 38.56) | −1.85 (−1.99 to −1.72) | |
| Western sub-Saharan Africa | 9,814 (5,638 to 12,926) | (17.1 to 37.82) | 29,735 (15,634 to 40,053) | 41.46 (21.70 to 55.16) | 202.99 (177.27 to 209.87) | 1.25 (1.2 to 1.31) | 9,405 (5,452 to 12,334) | (18 to 39.67) | 24,689 (13,076 to 32,847) | 38.56 (20.37 to 50.45) | 162.5 (139.83 to 166.31) | 0.87 (0.83 to 0.92) | |
Data are presented as absolute numbers or ASRs (per 100,000 person-years). APC, annual percentage change; ASDR, age-standardized death rate; ASIR, age-standardized incidence rate; ASR, age-standardized rate; CI, confidence interval; EAPC, estimated annual percentage change; Num_change, number change; SDI, socio-demographic index; PC, prostate cancer.
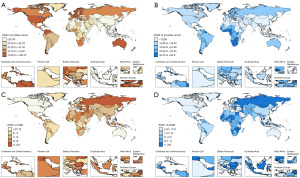
Analysis of global EAPC trends in PC burden across 204 countries
This study, based on the 2021 GBD data, analyzed the ASIR, ASPR, DALYs, and ASDR of PC across 204 countries and territories, with global geographical distribution maps generated for visualization (Figure 4). The results revealed substantial regional disparities in the ASIR of PC, with quintile grouping indicating a range from <20.39 per 100,000 to 74.62–196.12 per 100,000 (Figure 4A). Countries with the highest ASIR were predominantly located in North America, Western Europe, and parts of Oceania, whereas those with the lowest ASIR were mainly in sub-Saharan Africa and certain Asian regions. The global ASPR of PC also exhibited significant geographical variation, ranging from <92.63 per 100,000 in the lowest quintile to 555.67–1,527.67 per 100,000 in the highest quintile (Figure S3A). Similar to incidence patterns, the highest ASPR values were observed in high-income regions, whereas lower prevalence rates were mainly concentrated in low-SDI countries. The burden of PC, as measured by DALYs, also varied across regions, with the lowest quintile having an ASR of DALYs <193.41 per 100,000 (Figure S3B), while the highest quintile reached 562.62–1,542.79. Countries with a high DALY burden often exhibited correspondingly high mortality rates. The ASDR further demonstrated significant geographical disparities, ranging from <10.98 per 100,000 in the lowest quintile to 32.55–93.9 per 100,000 in the highest quintile (Figure 4B). Higher mortality rates were primarily observed in sub-Saharan Africa and the Caribbean, whereas lower mortality rates were concentrated in developed countries, underscoring the impact of healthcare accessibility, screening programs, and treatment advancements on PC outcomes. Additionally, analysis of the estimated EAPC in ASIR, ASPR, DALYs, and ASDR from 1990 to 2021 revealed heterogeneous trends across different countries. Some nations exhibited increasing ASIR and ASPR, whereas others showed stable or declining incidence rates (Figure 4C,4D and Figure S3C,S3D), likely due to improvements in screening and diagnostic practices. Meanwhile, trends in ASR of DALYs and ASDR may reflect advancements in PC management and treatment strategies.
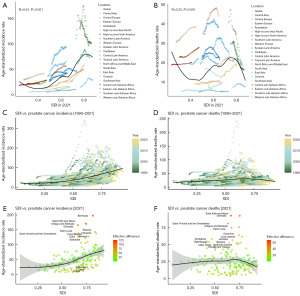
SDI and global disparities in PC burden
Analyses of incidence and mortality rates highlighted distinct geographical trends (Figure 5). Bermuda exhibited the highest effective difference in ASIR (125.80 per 100,000) (Figure 5A), while Grenada recorded the largest difference in mortality rates (67.45 per 100,000) (Figure 5B). Moreover, the analysis of PC burden revealed significant geographical variations in incidence, prevalence, DALYs, and mortality rates (Figure S4). A linear regression model identified a strong positive correlation between the SDI and ASPR (R2=0.3895, P<0.001) (Figure S4A,S4B), with high-SDI regions, such as Bermuda, Antigua, and Barbuda, showing the greatest prevalence discrepancies, recording effective differences of 1,020.70 and 673.13 per 100,000, respectively. Conversely, regression analysis for age-standardized DALYs rates demonstrated a much weaker correlation with SDI (R2=0.0136, P<0.001), indicating substantial disparities in countries such as Grenada, Saint Kitts, and Nevis, where effective differences reached 1,088.84 and 1,047.60 per 100,000, respectively.
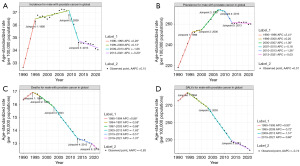
Global trends in PC burden from 1990 to 2021
This study, based on the GBD Study 2021 data, analyzed the annual average percentage change (AAPC) in global male PC incidence from 1990 to 2021 and provided an in-depth exploration of four key indicators: incidence, mortality, DALYs, and prevalence. The results indicated that global male PC incidence and prevalence showed increases of 0.150% and 0.568% (Figure 5C and Figure S4C), respectively, reflecting the rise in screening and diagnostic rates for PC. In contrast, mortality decreased by −0.83% (Figure 5D). DALYs also exhibited a decline of −0.736% (Figure S4D), which may have been associated with enhanced medical interventions and improvements in patients’ quality of life. Further regional comparisons revealed that while global incidence and prevalence increased, and mortality and disease burden decreased, some regions (Figure 5E,5F and Figure S4E,S4F), such as Eastern Europe and South Asia, still bore a higher PC burden, possibly due to differences in local healthcare resources and the level of early screening implementation. Moreover, the analysis highlighted significant regional variations, with notable improvements in PC treatment outcomes in Western Europe and North America, while other regions, like Eastern Europe and South Asia, required more public health interventions. Finally, the breakpoint analysis revealed several keys turning points, illustrating the changing trends of PC across different time periods. Overall, this study provided detailed data support for global PC trends and offered scientific evidence for the development of targeted public health strategies.
AAPC in PC incidence and mortality [1990–2021]
From 1990 to 2021, global trends in PC incidence, mortality, prevalence, and DALYs exhibited notable variations (Figure 6). Specifically, the ASIR of PC showed multiple joinpoints, with APCs of 0.2% [1990–1996], 1.05% [2000–2007], −0.184% [2007–2010], −1.36% [2010–2013], and −0.03% [2013–2021], resulting in an overall AAPC of 0.89% (Figure 6A). This indicated a modest overall increase in global PC incidence over the study period. Regarding prevalence, the ASPR exhibited a steady upward trend, with APCs of 2.26% [1990–1995], 0.13% [1995–2009], −1.66% [2009–2013], and −0.20% [2013–2021], leading to an overall AAPC of 0.15% (Figure 6B). This suggested a sustained rise in global PC prevalence, albeit at a slower rate in recent years. The ASDR demonstrated several joinpoints, with APCs of 0.88% [1990–1994], −0.58% [1994–1997], −0.88% [1997–2003], −1.63% [2003–2013], −0.51% [2013–2019], and −1.37% [2019–2021], culminating in an overall AAPC of −0.83% (Figure 6C). This reflected a relatively stable mortality trend, with a more pronounced decline in recent years, likely due to advancements in treatment and healthcare improvements. Similarly, the burden of DALYs for PC exhibited a downward trend, with APCs of 0.90% [1990–1994], −0.72% [1994–2003], −1.51% [2003–2013], and −0.60% [2013–2021], yielding an overall AAPC of −0.74% (Figure 6D). These findings indicated that although PC incidence and prevalence had been rising, the decline in DALY burden suggests improved survival outcomes and better disease management over time.
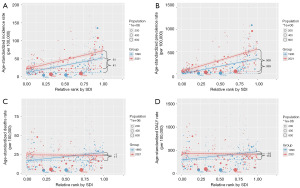
Growing health inequalities in the global burden of PC from 1990 to 2021
To begin with, a clear positive correlation was observed between the incidence rate and SDI, with regions characterized by higher SDI consistently exhibiting significantly higher incidence rates (Figure 7). This trend became increasingly pronounced between 1990 and 2021, indicating a steady rise in PC incidence in high-SDI regions (Figure 7A). A strong positive correlation was found between the prevalence rate and SDI (Figure 7B), with a marked increase in prevalence observed in high-SDI regions throughout the study period. In contrast, the relationships between mortality and DALY rates with SDI were comparatively weaker. Although a modest increase in mortality was noted in high-SDI regions (Figure 7C,7D), the overall trend was less pronounced when compared to the incidence rates. These findings suggest that the higher prevalence rates in wealthier regions are likely attributable to longer survival times, facilitated by advances in healthcare infrastructure and early detection programs.
Discussion
PC was the second most common cancer among men globally, accounting for 14.1% of all cancer cases and 6.8% of all cancer-related deaths in men in 2020 (1). However, the incidence and mortality rates varied significantly by geographical region (16). This study offers a thorough analysis of global PC trends, emphasizing marked regional disparities in incidence, prevalence, mortality, and DALYs based on the 2021 GBD data. Our results demonstrate clear epidemiological patterns that are strongly shaped by socio-demographic factors, healthcare infrastructure, and the effectiveness of early screening initiatives.
The global incidence and prevalence of PC have shown an increasing trend, with AAPC of 0.150% and 0.568%, respectively. These trends likely reflect advancements in diagnostic capabilities and increased awareness leading to higher detection rates. In contrast, mortality and DALYs have declined by −0.83% and −0.736%, respectively, suggesting improvements in treatment efficacy and patient management. However, the overall trends mask substantial regional variations in disease burden. High-income regions, such as Australasia and North America, have demonstrated reductions in mortality and DALYs, largely attributable to the widespread implementation of early screening programs, access to innovative therapies, and enhanced patient care. Conversely, regions such as Eastern Europe and South Asia continue to experience a higher PC burden, as evidenced by elevated effective EAPC across multiple indicators. These disparities likely stem from insufficient healthcare resources, limited access to early diagnostic services, and variations in healthcare policies. We utilized Pearson correlation analysis to explore the relationship between EAPC and SDI, identifying a more pronounced association between SDI and mortality as well as DALYs. However, we acknowledge that EAPC variations are influenced by multiple factors beyond SDI, including healthcare accessibility, disease screening, genetic predisposition, and environmental exposures. Therefore, we do not consider SDI as the sole determinant of EAPC changes but rather as a potential contributing factor to global cancer burden trends. Future research should incorporate multivariate analytical approaches, such as generalized linear models or machine learning techniques, to further investigate the complex interplay among these variables.
In particular, the significantly higher EAPC in Eastern Europe suggests a growing disease burden, underscoring the need for targeted interventions to enhance screening, diagnosis, and treatment access. The persistently higher incidence, prevalence, and mortality rates in these regions highlight ongoing challenges in PC management despite global advancements. These findings are consistent with previous studies indicating that disparities in healthcare accessibility and resource allocation contribute to regional variations in cancer outcomes (17-19). In contrast, high-income regions have benefited from long-term investments in healthcare systems, enabling reductions in both mortality and disease burden. These trends underscore the critical role of healthcare investments in reducing PC mortality and improving patient prognosis. The rising global burden of PC, particularly in high-SDI regions, underscores the critical need for region-specific public health strategies (7). While incidence rates have surged in wealthier areas, likely driven by improved diagnostic capabilities and healthcare infrastructure, mortality and DALY rates exhibit weaker correlations with SDI, suggesting that factors such as early detection, treatment access, and healthcare quality play significant roles in moderating outcomes. These findings emphasize the importance of addressing regional disparities in healthcare access to reduce the growing burden of PC, especially in regions with higher socio-economic development.
Aging remains a crucial factor in PC burden (20), with individuals aged 50 years and older, particularly those over 80 years, experiencing disproportionately high mortality rates. Given the expected rise in the aging population, there is an urgent need for age-specific screening strategies and personalized cancer care approaches (21,22). Future public health initiatives should prioritize tailored interventions for elderly patients (23), including improved palliative care services and optimized treatment strategies that balance efficacy with quality-of-life considerations. However, the absence of histopathological stratification, such as Gleason grading, in global disease burden estimates limits the precision of risk assessment and policy recommendations. Given ongoing debates over the classification of low-risk PC, particularly Gleason 6, refining epidemiological data to incorporate disease severity would enhance the development of evidence-based screening and treatment strategies.
Additionally, the analysis of EAPC trends across countries highlights substantial progress in PC control in high-income nations such as Canada, whereas low- and middle-income countries, such as Georgia, continue to face significant disease burdens. The faster increase in prevalence compared to incidence suggests improved patient survival, likely due to advancements in medical interventions. Concurrent declines in DALYs and mortality indicate overall progress in PC management; however, the extent of these improvements varies significantly across regions. These disparities necessitate further investigation to identify specific barriers to effective disease control, particularly in resource-limited settings (17,24). Addressing these challenges will require concerted efforts to improve early diagnosis, expand access to treatment, and enhance healthcare infrastructure.
Conclusions
This study highlights the global disparities in PC burden and its association with socio-demographic factors. The findings underscore the need for targeted public health strategies to address regional and age-related variations. Beyond SDI, future research should explore additional determinants such as healthcare accessibility and genetic factors. Strengthening international collaboration and optimizing healthcare resources will be crucial in reducing disparities and improving outcomes worldwide.
Acknowledgments
None.
Footnote
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-2025-103/prf
Funding: This study was supported by
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-2025-103/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Filho AM, Laversanne M, Ferlay J, et al. The GLOBOCAN 2022 cancer estimates: Data sources, methods, and a snapshot of the cancer burden worldwide. Int J Cancer 2025;156:1336-46. [Crossref] [PubMed]
- Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024;403:2100-32. [Crossref] [PubMed]
- Culp MB, Soerjomataram I, Efstathiou JA, et al. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur Urol 2020;77:38-52. [Crossref] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Alfaro T, Martinez-Folgar K, Stern D, et al. Variability and social patterning of cancer mortality in 343 Latin American cities: an ecological study. Lancet Glob Health 2025;13:e268-76. [Crossref] [PubMed]
- Blas L, Shiota M, Onozawa M, et al. Primary management of prostate cancer by universal health coverage effective coverage index. World J Urol 2025;43:146. [Crossref] [PubMed]
- Zi H, Liu MY, Luo LS, et al. Global burden of benign prostatic hyperplasia, urinary tract infections, urolithiasis, bladder cancer, kidney cancer, and prostate cancer from 1990 to 2021. Mil Med Res 2024;11:64. [Crossref] [PubMed]
- Miller DC, Saigal CS, Litwin MS. The demographic burden of urologic diseases in America. Urol Clin North Am 2009;36:11-27. v. [Crossref] [PubMed]
- Guo J, Jiao W, Xia S, et al. The global, regional, and national patterns of change in the burden of chronic kidney disease from 1990 to 2021. BMC Nephrol 2025;26:136. [Crossref] [PubMed]
- Wyper GMA. The global burden of disease study and Population Health Metrics. Popul Health Metr 2024;22:35. [Crossref] [PubMed]
- Global Burden of Disease Cancer Collaboration. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol 2019;5:1749-68. [Crossref] [PubMed]
- Washington CG, Deville C. Health Disparities and Inequities in the Utilization of Proton Therapy for Prostate Cancer. Cancers (Basel) 2024;16:3837. [Crossref] [PubMed]
- Ruan Y, Heer E, Warkentin MT, et al. The association between neighborhood-level income and cancer stage at diagnosis and survival in Alberta. Cancer 2024;130:563-75. [Crossref] [PubMed]
- Strömberg U, Berglund A, Carlsson S, et al. Socioeconomic inequality in prostate cancer diagnostics, primary treatment, rehabilitation, and mortality in Sweden. Int J Cancer 2024;155:637-45. [Crossref] [PubMed]
- Alba C, Zheng Z, Wadhera RK. Changes in Health Care Access and Preventive Health Screenings by Race and Ethnicity. JAMA Health Forum 2024;5:e235058. [Crossref] [PubMed]
- Cai Q, Chen Y, Zhang D, et al. Estimates of over-time trends in incidence and mortality of prostate cancer from 1990 to 2030. Transl Androl Urol 2020;9:196-209. [Crossref] [PubMed]
- Global fertility in 204 countries and territories, 1950-2021, with forecasts to 2100: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet 2024;403:2057-99. [Crossref] [PubMed]
- Liu C, Reger M, Fan H, et al. Dietary intake of isoflavones and coumestrol and risk of pancreatic cancer in the prostate, lung, colorectal, and ovarian cancer screening trial. Br J Cancer 2025;132:266-75. [Crossref] [PubMed]
- Chen AM. Barriers to health equity in the United States of America: can they be overcome? Int J Equity Health 2025;24:39. [Crossref] [PubMed]
- Diao X, Guo C, Jin Y, et al. Cancer situation in China: an analysis based on the global epidemiological data released in 2024. Cancer Commun (Lond) 2025;45:178-97. [Crossref] [PubMed]
- Safiri S, Shamekh A, Hassanzadeh K, et al. The burden of prostate cancer in the North Africa and Middle East Region from 1990 to 2021. Sci Rep 2025;15:1853. [Crossref] [PubMed]
- Forecasting the effects of smoking prevalence scenarios on years of life lost and life expectancy from 2022 to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Public Health 2024;9:e729-44. [Crossref] [PubMed]
- Global, regional, and national progress towards the 2030 global nutrition targets and forecasts to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 2025;404:2543-83. [Crossref] [PubMed]
- Song B, Liang R. Integrating artificial intelligence with smartphone-based imaging for cancer detection in vivo. Biosens Bioelectron 2025;271:116982. [Crossref] [PubMed]


