The epidemiology of premature ejaculation
Introduction
Vast advances have occurred over the past decade with regards to understanding the epidemiology, pathophysiology and management of premature ejaculation (PE) (1); however, we still have much to learn about this common sexual problem. As a standardized evidence-based definition of PE has only recently been established (2), the reported prevalence rates of PE prior to this definition have been difficult to interoperate. As a result, a large range of conflicting prevalence rates have been reported (Table 1). In addition to the lack of a standardized definition and operational criteria, the method of recruitment for study participation and method of data collection have obviously contributed to the broad range of reported prevalence rates. Controversy regarding the specific criteria comprising the disease of PE has not only hindered the ability to determine true prevalence rates, but also to conduct evidence-based research on the treatment of the disease. Understanding the clinical significance of a reported sexual dysfunctions also remains a challenge (41).
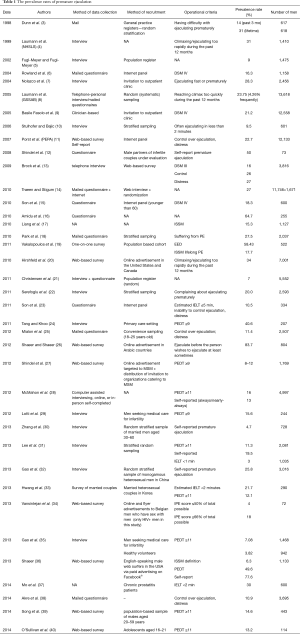
Full table
In an attempt to remedy the disparity among reported prevalence rates, the International Society for Sexual Medicine (ISSM) developed an evidence-based definition and established set operational criteria (2). The American Psychiatric Association also recently revised their definition of PE, including a 1-minute cut off latency and the criterion of “ejaculation before desired” and “significant clinical distress” (42). Both of these definitions include three main parameters: ejaculatory latency time, distress and ejaculating before desired. A recent interesting statistical analysis took all three of these operational criteria into account and found that modifying each individual operational criterion could significantly alter the prevalence rates of PE (43). Thus, adherence to these criteria aims to allow for a better understanding of the prevalence of PE, according to each specific definition.
Some of the first to recognize the need for a specific definition of PE were Waldinger and Schweitzer, who hypothesized that the true prevalence of patients actually seeking treatment for PE was much less than previously reported prevalence rates (44,45). They proposed a new classification system of PE (46). Based on their classification system, two separate observational, cross-sectional surveys from two different continents found that the overall prevalence of the complaint of PE to be 19.8% and 25.80% (22,32) (Table 2). Further stratifying these complaints into the classifications defined, the complaint of lifelong PE was seen at rates of 2.3% and 3.2%, while the rates of acquired PE were 3.9% and 4.5%, variable PE were 8.5% and 11.4% and subjective PE were 5.1% and 6.4% (22,32). Interestingly both of these studies found that men with acquired PE were more likely to seek treatment when compared to men with lifelong PE. Treatment seeking behavior may contribute to errors in the previously reported rates of PE, as it is possible that men with lifelong PE come to terms with their problem and not seek treatment. The additional psychological burden of a new change in ejaculatory latency in acquired PE, on the other hand, may prompt more frequent treatment seeking behaviors (47). Thus, it is likely that a disparity exists between the incidence of various PE sub-types in the general community and in men actively seeking treatment for PE (48,49). This disparity could be a further barrier to understanding the true incidence of each sub-type of PE.
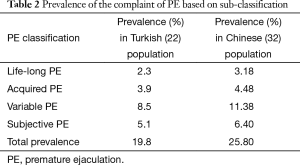
Full table
Several recent studies applying up-to-date definitions and operational criteria have examined the prevalence of PE in men with other associated urologic complaints. Zhang et al. (50) completed an investigation regarding the association of the International Prostate Symptom Score (IPSS) to the four various PE syndromes, and found that men complaining of ejaculating prematurely also reported worse IPSS than men without PE complaints. Another cross-sectional study was conducted to determine the prevalence of PE among adult male participants with lower urinary tract symptoms (LUTS) and found that among the participants consulted with LUTS, 27% also had concomitant PE (51). Recently, Li and Kang (52) performed a meta-analysis of sexual dysfunctions that included a total of 11,189 men diagnosed with chronic prostatitis and chronic pelvic pain syndrome, and found the prevalence of PE to be 40% in these men. The results from these studies are promising with regards to developing an understanding of the true prevalence of PE according to the newly adapted definitions.
Conclusions
The new criteria and classification of PE will allow for continued research into the diverse phenomenology, etiology and pathogenesis of the disease to be conducted (53). Although the pathogenesis of lifelong and acquired PE differs, the presence of shared dimensions, such as a lack of ejaculatory control and the presence of negative personal consequences, suggest a potential for a single unifying definition of both lifelong and acquired PE (54). While the absolute pathophysiology and true prevalence of PE remains unclear, developing a better understanding of the true prevalence of the disease will allow for the completion of more accurate analysis and treatment of the disease.
Acknowledgements
None.
Footnote
Conflict of Interest: The authors have no conflicts of interest to declare.
References
- Saitz TR, Serefoglu EC. Advances in understanding and treating premature ejaculation. Nat Rev Urol 2015;12:629-40. [Crossref] [PubMed]
- Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second international society for sexual medicine ad hoc committee for the definition of premature ejaculation. Sex Med 2014;2:41-59. [Crossref] [PubMed]
- Dunn KM, Croft PR, Hackett GI. Sexual problems: a study of the prevalence and need for health care in the general population. Fam Pract 1998;15:519-24. [Crossref] [PubMed]
- Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. JAMA 1999;281:537-44. [Crossref] [PubMed]
- Fugl-Meyer K, Fugl-Meyer AR. Sexual disabilities are not singularities. Int J Impot Res 2002;14:487-93. [Crossref] [PubMed]
- Rowland D, Perelman M, Althof S, et al. Self-reported premature ejaculation and aspects of sexual functioning and satisfaction. J Sex Med 2004;1:225-32. [Crossref] [PubMed]
- Nolazco C, Bellora O, Lopez M, et al. Prevalence of sexual dysfunctions in Argentina. Int J Impot Res 2004;16:69-72. [Crossref] [PubMed]
- Laumann EO, Nicolosi A, Glasser DB, et al. Sexual problems among women and men aged 40-80 y: prevalence and correlates identified in the Global Study of Sexual Attitudes and Behaviors. Int J Impot Res 2005;17:39-57. [Crossref] [PubMed]
- Basile Fasolo C, Mirone V, Gentile V, et al. Premature ejaculation: prevalence and associated conditions in a sample of 12,558 men attending the andrology prevention week 2001--a study of the Italian Society of Andrology (SIA). J Sex Med 2005;2:376-82. [Crossref] [PubMed]
- Stulhofer A, Bajic Z. Prevalence of erectile and ejaculatory difficulties among men in Croatia. Croat Med J 2006;47:114-24. [PubMed]
- Porst H, Montorsi F, Rosen RC, et al. The Premature Ejaculation Prevalence and Attitudes (PEPA) survey: prevalence, comorbidities, and professional help-seeking. Eur Urol 2007;51:816-23. [Crossref] [PubMed]
- Shindel AW, Nelson CJ, Naughton CK, et al. Premature ejaculation in infertile couples: prevalence and correlates. J Sex Med 2008;5:485-91. [Crossref] [PubMed]
- Brock GB, Benard F, Casey R, et al. Canadian male sexual health council survey to assess prevalence and treatment of premature ejaculation in Canada. J Sex Med 2009;6:2115-23. [Crossref] [PubMed]
- Traeen B, Stigum H. Sexual problems in 18-67-year-old Norwegians. Scand J Public Health 2010;38:445-56. [Crossref] [PubMed]
- Son H, Song SH, Kim SW, et al. Self-reported premature ejaculation prevalence and characteristics in Korean young males: community-based data from an internet survey. J Androl 2010;31:540-6. [Crossref] [PubMed]
- Amidu N, Owiredu WK, Woode E, et al. Prevalence of male sexual dysfunction among Ghanaian populace: myth or reality? Int J Impot Res 2010;22:337-42. [Crossref] [PubMed]
- Liang CZ, Hao ZY, Li HJ, et al. Prevalence of premature ejaculation and its correlation with chronic prostatitis in Chinese men. Urology 2010;76:962-6. [Crossref] [PubMed]
- Park HJ, Park JK, Park K, et al. Prevalence of premature ejaculation in young and middle-aged men in Korea: a multicenter internet-based survey from the Korean Andrological Society. Asian J Androl 2010;12:880-9. [Crossref] [PubMed]
- Vakalopoulos I, Dimitriadis G, Varnava C, et al. Prevalence of ejaculatory disorders in urban men: results of a random-sample survey. Andrologia 2011;43:327-33. [Crossref] [PubMed]
- Hirshfield S, Chiasson MA, Wagmiller RL Jr, et al. Sexual dysfunction in an Internet sample of U.S. men who have sex with men. J Sex Med 2010;7:3104-14. [Crossref] [PubMed]
- Christensen BS, Gronbaek M, Osler M, et al. Sexual dysfunctions and difficulties in denmark: prevalence and associated sociodemographic factors. Arch Sex Behav 2011;40:121-32. [Crossref] [PubMed]
- Serefoglu EC, Yaman O, Cayan S, et al. Prevalence of the complaint of ejaculating prematurely and the four premature ejaculation syndromes: results from the Turkish Society of Andrology Sexual Health Survey. J Sex Med 2011;8:540-8. [Crossref] [PubMed]
- Son H, Song SH, Lee JY, et al. Relationship between premature ejaculation and depression in Korean males. J Sex Med 2011;8:2062-70. [Crossref] [PubMed]
- Tang WS, Khoo EM. Prevalence and correlates of premature ejaculation in a primary care setting: a preliminary cross-sectional study. J Sex Med 2011;8:2071-8. [Crossref] [PubMed]
- Mialon A, Berchtold A, Michaud PA, et al. Sexual dysfunctions among young men: prevalence and associated factors. J Adolesc Health 2012;51:25-31. [Crossref] [PubMed]
- Shaeer O, Shaeer K. The Global Online Sexuality Survey (GOSS): ejaculatory function, penile anatomy, and contraceptive usage among Arabic-speaking Internet users in the Middle East. J Sex Med 2012;9:425-33. [Crossref] [PubMed]
- Shindel AW, Vittinghoff E, Breyer BN. Erectile dysfunction and premature ejaculation in men who have sex with men. J Sex Med 2012;9:576-84. [Crossref] [PubMed]
- McMahon CG, Lee G, Park JK, et al. Premature ejaculation and erectile dysfunction prevalence and attitudes in the Asia-Pacific region. J Sex Med 2012;9:454-65. [Crossref] [PubMed]
- Lotti F, Corona G, Rastrelli G, et al. Clinical correlates of erectile dysfunction and premature ejaculation in men with couple infertility. J Sex Med 2012;9:2698-707. [Crossref] [PubMed]
- Zhang H, Yip AW, Fan S, et al. Sexual dysfunction among Chinese married men aged 30-60 years: a population-based study in Hong Kong. Urology 2013;81:334-9. [Crossref] [PubMed]
- Lee SW, Lee JH, Sung HH, et al. The prevalence of premature ejaculation and its clinical characteristics in Korean men according to different definitions. Int J Impot Res 2013;25:12-7. [Crossref] [PubMed]
- Gao J, Zhang X, Su P, et al. Prevalence and factors associated with the complaint of premature ejaculation and the four premature ejaculation syndromes: a large observational study in China. J Sex Med 2013;10:1874-81. [Crossref] [PubMed]
- Hwang I, Yang DO, Park K. Self-Reported Prevalence of and Attitudes toward Premature Ejaculation in a Community-Based Study of Married Couples. World J Mens Health 2013;31:70-5. [Crossref] [PubMed]
- Vansintejan J, Janssen J, Van De Vijver E, et al. The Gay Men Sex Studies: prevalence of sexual dysfunctions in Belgian HIV(+) gay men. HIV AIDS (Auckl) 2013;5:89-96. [Crossref] [PubMed]
- Gao J, Zhang X, Su P, et al. Relationship between sexual dysfunction and psychological burden in men with infertility: a large observational study in China. J Sex Med 2013;10:1935-42. [Crossref] [PubMed]
- Shaeer O. The global online sexuality survey (GOSS): The United States of America in 2011 Chapter III--Premature ejaculation among English-speaking male Internet users. J Sex Med 2013;10:1882-8. [Crossref] [PubMed]
- Mo MQ, Long LL, Xie WL, et al. Sexual dysfunctions and psychological disorders associated with type IIIa chronic prostatitis: a clinical survey in China. Int Urol Nephrol 2014;46:2255-61. [Crossref] [PubMed]
- Akre C, Berchtold A, Gmel G, et al. The evolution of sexual dysfunction in young men aged 18-25 years. J Adolesc Health 2014;55:736-43. [Crossref] [PubMed]
- Song SH, Choi WS, Son H, et al. Validity of the Premature Ejaculation Diagnostic Tool in four subgroups of premature ejaculation syndrome: data from the Korean Internet Sexuality Survey - part 1. Sex Health 2014;11:73-80. [Crossref] [PubMed]
- O'Sullivan LF, Brotto LA, Byers ES, et al. Prevalence and characteristics of sexual functioning among sexually experienced middle to late adolescents. J Sex Med 2014;11:630-41. [Crossref] [PubMed]
- Mitchell KR, Jones KG, Wellings K, et al. Estimating the Prevalence of Sexual Function Problems: The Impact of Morbidity Criteria. J Sex Res 2015.1-13. [Crossref] [PubMed]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5™ 5th ed. Arlington, VA: American Psychiatric Publishing Inc., 2013.
- Rowland DL, Kolba TN. Understanding the effects of establishing various cutoff criteria in the definition of men with premature ejaculation. J Sex Med 2015;12:1175-83. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part I--validity of DSM-IV-TR. J Sex Med 2006;3:682-92. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. Changing paradigms from a historical DSM-III and DSM-IV view toward an evidence-based definition of premature ejaculation. Part II--proposals for DSM-V and ICD-11. J Sex Med 2006;3:693-705. [Crossref] [PubMed]
- Waldinger MD, Schweitzer DH. The use of old and recent DSM definitions of premature ejaculation in observational studies: a contribution to the present debate for a new classification of PE in the DSM-V. J Sex Med 2008;5:1079-87. [Crossref] [PubMed]
- Serefoglu EC, Yaman O, Cayan S, et al. The comparison of premature ejaculation assessment questionnaires and their sensitivity for the four premature ejaculation syndromes: results from the Turkish society of andrology sexual health survey. J Sex Med 2011;8:1177-85. [Crossref] [PubMed]
- Serefoglu EC, Cimen HI, Atmaca AF, et al. The distribution of patients who seek treatment for the complaint of ejaculating prematurely according to the four premature ejaculation syndromes. J Sex Med 2010;7:810-5. [Crossref] [PubMed]
- Lei L, Wang J, Zhang Z, et al. Lipopolysaccharide-induced apoptosis in a murine intestinal endocrine cell line by modulation of Bcl-2, Bax and caspase-3. Mol Med Rep 2013;8:1649-54. [PubMed]
- Zhang X, Tang D, Xu C, et al. The relationship between self-estimated intravaginal ejaculatory latency time and International Prostate Symptom Score in middle-aged men complaining of ejaculating prematurely in China. J Sex Med 2015;12:705-12. [Crossref] [PubMed]
- Silangcruz JM, Chua ME, Morales ML Jr. Prevalence and factor association of premature ejaculation among adult Asian males with lower urinary tract symptoms. Prostate Int 2015;3:65-9. [Crossref] [PubMed]
- Li HJ, Kang DY. Prevalence of sexual dysfunction in men with chronic prostatitis/chronic pelvic pain syndrome: a meta-analysis. World J Urol 2016;34:1009-17. [Crossref] [PubMed]
- Althof SE, McMahon CG, Waldinger MD, et al. An Update of the International Society of Sexual Medicine's Guidelines for the Diagnosis and Treatment of Premature Ejaculation (PE). Sex Med 2014;2:60-90. [Crossref] [PubMed]
- Serefoglu EC, McMahon CG, Waldinger MD, et al. An evidence-based unified definition of lifelong and acquired premature ejaculation: report of the second International Society for Sexual Medicine Ad Hoc Committee for the Definition of Premature Ejaculation. J Sex Med 2014;11:1423-41. [Crossref] [PubMed]


