Vesicoureteral reflux and bladder dysfunction
Introduction
When Hinman and Baumann first described the relationship of bladder dysfunction and VUR back in 1976, they suggested that reflux may be secondary to vesical incoordination and that a technically well-performed repair of the reflux can result in persistent infection, malfunction of the UVJ and more damage to the upper urinary tract (1-7). It is widely accepted that bladder dysfunction can lead to increased risk of UTI, the risk getting even higher if there is reflux present. Many clinicians incorporate evaluation and treatment of voiding dysfunction when treating VUR either medically or surgically. In this article, the influence of bladder dysfunction on VUR and vice versa will be discussed along with its effect on renal scarring.
Bladder dysfunction and vesicoureteral reflux
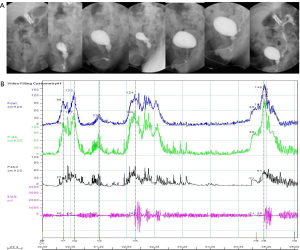
The reported prevalence of bladder dysfunction in a VUR population varies. When diagnosed using invasive urodynamic investigations, higher figures were generally found (38-75%) in contrast to what was seen when nonurodynamic investigations such as questionnaires were used (18-52%) (8) Through a retrospective review of urodynamic studies in 75 infants with primary VUR, Chandra suggested that high intravesical pressures contribute to the development and severity of VUR, and that high voiding detrusor pressure in some infants with primary VUR may be related to inadequate relaxation of the external urethral sphincter (9). In a normal immature bladder, maximum voiding pressure is higher than maturity and asynchronous detrusor/sphincter activity is quite often noted (Figure 1). The detrusor contraction against a partially opened or closed urethral sphincter results in high bladder pressure and might affect the occurrence of VUR depending on the competence of the UVJ. However, such dyscoordination in the infant bladder is not considered as true bladder dysfunction since it is literally under maturation and explains why many infants grow out of their VUR.
After bladder control, bladder dysfunction is characterized by functional obstruction during voiding due to voluntary constriction of the urinary sphinter during bladder contraction and this is believed to be an abnormal, learned response to uncontrolled bladder contractions (10). Functional obstruction and resultant elevation in bladder pressure can lead to changes in the anatomy and function of the bladder and ureterovesical junction, resulting in production and persistence of VUR.
Many reports suggest that isolated overactive bladder (OAB) may be a dysfunction with little influence on spontaneous VUR resolution, implicating that OAB is a milder lower urinary tract dysfunction than voiding phase problems. But in some children, involuntary detrusor contractions during bladder filling may cause intermittent VUR while reflux does not occur during voiding (Figure 2). When children with VUR grade III-IV were investigated for LUT function by noninvasive methods, Sillen et al. noted that voiding phase problems at follow up were associated with persistent VUR in children with lower urinary tract dysfunction, as noted previously in studies of older children with dysfunctional elimination syndrome, dysfunctional voiding and dilated bladder dysfunction but not isolated OAB (1).
In terms of surgical outcome, the rate of cure following endoscopic therapy is reported to be less in children with than without bladder bowel dysfunction (BBD) but there is no difference for open surgery (2). However, in review of the literature, one can find numerous reports that ureteral reimplantation into an abnormally functioning bladder can be unsuccessful, probably due to same reasons that cause abnormality of the UVJ and VUR (11). The rate of postoperative UTI is also known to be greater in children with (22%) than without (5%) BBD (2). Such study results strongly support that urodynamic evaluation can provide valuable information regarding the diagnosis, treatment and prognosis of children with VUR, especially in older children who might have learned to compensate and control symptoms of bladder dysfunction. Koff et al. found that up to 30% of children with uninhibited bladder contractions do not present incontinence because they contract their sphincters strong enough, but at the expense of increased intravesical pressure. Simultaneous treatment for bladder dysfunction consisting of pharmacotherapy or biofeedback can be effective in the spontaneous resolution of VUR or in achieving optimal results of anti-reflux surgery.
Bladder dysfunction and urinary tract infection
It is well known that bladder dysfunction is associated with increased rate of UTI with and without reflux.
Urodynamic study in 52 children with febrile UTI with photopenic lesions on renal scintigraphy but no evidence of VUR on voiding cystourethrogram showed abnormalities such as high filling pressures, high pressure uninhibited contractions, high voiding pressures and discoordinated voiding in 93% (12).
Increased rate of breakthrough infections in spite of continuous antibiotic prophylaxis have been documented in children with VUR and bladder dysfunction.
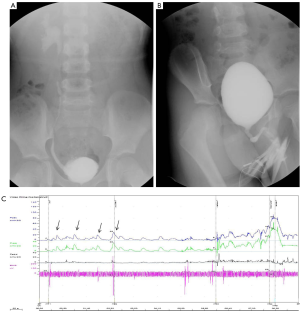
Girls with dysfunctional voiding are a subset of patients who can be predisposed to the development of UTI. Dysfunctional voiding is characterized by increased sphincter activity during the voiding phase which can cause ‘milk-back’ of bacteria into the bladder and subsequent UTI (3). Moreover, beak sign and after contraction are quite often found on video urodynamic studies of patients with UTI and/or voiding dysfunction. Another finding that can be seen in girls is partial coverage of the urethral meatus which deflects the urine stream towards the clitoris (Figure 3). Such phenomenon can cause dysfunctional voiding by contraction of the sphincter along with the pelvic muscles as a result of direct stimulation of the clitoris or by refluxing urine back into the vagina after hitting the clitoris.

In addition to milk-back of urine, involuntary contractions or excessive sphincter contraction during voiding results in increased intravesical pressure which may be responsible for mucosal ischemia (13). This can lead to decrease in mucosal immunity and thus increase the risk of UTI. Increased incidence of cystitis has been reported in children with dysfunctional voiding even after spontaneous disappearance or surgery of reflux (14).
Another risk factor for UTI in bladder dysfunction is residual urine. Even small volumes of residual urine can increase the risk of UTI and make treatment more difficult in adults, as well as in children with symptomatic bacteriuria and Lidefelt and co-workers have noted significant difference in residual urine volumes between children with acute cystitis and healthy controls (15). In patients with high grade reflux, the amount of refluxed urine returning to the bladder can be significant. However, it is not clear whether residual urine is a cause or a consequence of UTI, but it certainly seems to be associated with increased risk of recurrent UTI.
Bladder dysfunction and renal scarring
VUR with UTI and bladder dysfunction
The cause-and-effect relationship is not absolutely clear but it is unanimous that VUR, UTI and bladder dysfunction all play a role in the development of renal scars. Increased bladder pressure transmitted to the kidney in the presence of reflux can be crucial in the pathogenesis of reflux nephropathy. Correlations between the appearance or severity of renal scarring and urodynamically detected bladder dysfunction in children with VUR have been reported (16,17). Breakthrough infection defined as development of an infection during antibiotic prophylaxis can cause new scarring, even when the infection is afebrile and asymptomatic according to some reports. The incidence of breakthrough infection is more common in children with voiding dysfunction up to four times when compared to those without history of voiding dysfunction (18,19), suggesting the need for double antibiotic prophylaxis.
From the literature, it seems that dysfunctional voiding is more closely related to renal scarring than overactive bladder. Griffiths reported that in children with poor voiding contraction and urethral sphincter overactivity, the reflux is usually bilateral in spite of the stable bladder and reflux nephropathy was relatively common (20).
UTI without VUR
Whether sterile VUR under antibiotic chemoprophlaxis affects the development or aggravation of renal scars has been under debate. The report of the International Reflux Study Committee seems to add weight to the fact that renal scarring is almost always associated with urinary tract infection in clinical studies (21). On the contrary, McLorie et al. have concluded that renal parenchymal injury can occur while children are under surveillance and prophylactic antibiotics in their analysis of observational therapy in high grade VUR (22). Moreover, experimental studies by Hodson in porcine models showed that sterile reflux can lead to renal scars via intrarenal reflux (23). The exact role of intrarenal reflux is still controversial as many authors including Roberts et al. have reported that in surgically produced high pressure VUR, intrarenal reflux itself did not cause decrease in renal function in absence of UTI (24). But in study of infant monkeys which may have incompetent ureter opposed to the adult animal models, Mendoza et al. have found that high pressure reflux occurring in functional or mechanical outlet obstruction of the bladder was sufficient for the deterioration of renal function by means of increased tubular pressure and subsequent decrease in glomerular filtration pressure and blood flow to the efferent arterioles (4). The significance of intrarenal reflux in the absence of UTI is yet to be elucidated.
Another controversial is renal scarring as a result of UTI in association with bladder dysfunction without evident VUR. In a review of infants aged <1 year, Preda et al. noted among 149 patients with abnormal DMSA scans VUR was not detected in 105 (71%) (25). Possible theories include the hematogenous spread of infection, ascending pyelonephritis in the absence of reflux that could be seen in experimental studies with monkeys (26) and transient VUR that occurs during acute infection (27). Abnormal bladder function may be accompanied in these conditions, acting as one of the causal factors in the development of renal scar.
Bladder dysfunction and renal scar
Embryologically, VUR and renal anomaly can be induced by an anomaly in the ureteric bud region. Since the bladder outlet is also formed by such embryological structures, the dysfunction of the bladder might theoretically have the same origin (27) Studies have suggested DD genotype of angiotensin converting enzyme gene as a genetic susceptibility factor contributing to parenchymal damage (28,29). Kostic and co-workers found that some children may have genetic predisposition to renal scar development and found ACE I/D gene polymorphism as an independent determinant for the development of parenchymal damage in patients with bladder dysfunction (30). However, evidence is scarce and further research is needed to determine the direct genetic association between the two conditions.
VUR as a cause of bladder dysfunction
Vesicoureteral reflux has been recently suggested as a causative factor for bladder dysfunction which means that treatment of the reflux may cure bladder dysfunction in some patients. According to Lackgren’s report, bladder dysfunction was resolved in 29 (59%) of 54 VUR patients with associated bladder dysfunction following injection therapy alone (5). Bladder dysfunction was determined through questionnaire and charts in this study. But as previously mentioned, not all bladder dysfunction are symptomatic and the percentage of resolved bladder dysfunction may turn out to be lower if urodynamic studies were performed. Although VUR can be speculated as the cause of bladder dysfunction, it certainly cannot be applied to all patients who have both conditions and additional data will be needed to explain those in whom bladder dysfunction persists in spite of disappearance of reflux.
Conclusions
The fact that bladder dysfunction could develop and affect the resolution of VUR has been established by many authors. However, one should always be aware that bladder dysfunction may cause UTI and subsequent renal scarring even without VUR. Meanwhile, aggressive anti-reflux treatment should not be hesitated if the child fails to stay UTI-free since VUR in combination with UTI are the main causes of renal scarring, especially in patients with bladder dysfunction. Surveillance of bladder dysfunction even after spontaneous or surgical resolution of VUR is warranted.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sillén U, Brandström P, Jodal U, et al. The Swedish reflux trial in children: v. Bladder dysfunction. J Urol 2010;184:298-304. [PubMed]
- Peters CA, Skoog SJ, Arant BS Jr, et al. Summary of the AUA guideline on management of primary vesicoureteral reflux in Children. J Urol 2010;184:1134-44. [PubMed]
- De Paepe H, Hoebeke P, Renson C, et al. Pelvic-floor therapy in girls with recurrent urinary tract infections and dysfunctional voiding. Br J Urol 1998;81:109-13. [PubMed]
- Mendoza JM, Roberts JA. Effects of sterile high pressure vesicoureteral reflux on the monkey. J Urol 1983;130:602-6. [PubMed]
- Läckgren G, Sköldenberg E, Stenberg A. Endoscopic treatment with stabilized nonanimal hyaluronic acid/dextranomer gel is effective in vesicoureteral reflux associated with bladder dysfunction. J Urol 2007;177:1124-8. [PubMed]
- Hinman F, Baumann FW. Vesical and ureteral damage from voiding dysfunction in boys without neurologic or obstructive disease. Trans Am Assoc Genitourin Surg 1972;64:116-21. [PubMed]
- Hinman F Jr, Baumann FW. Complications of vesicoureteral operations from incoordination of micturition. J Urol 1976;116:638-43. [PubMed]
- Sillén U. Bladder dysfunction and vesicoureteral reflux. Adv Urol 2008.815472. [PubMed]
- Chandra M, Maddix H. Urodynamic dysfunction in infants with vesicoureteral reflux. J Pediatr 2000;136:754-9. [PubMed]
- Koff SA. Relationship between dysfunctional voiding and reflux. J Urol 1992;148:1703-5. [PubMed]
- Noe HN. The role of dysfunctional voiding in failure or complication of ureteral reimplantation for primary reflux. J Urol 1985;134:1172-5. [PubMed]
- Vega-P JM, Pascual LA. High-pressure bladder: an underlying factor mediating renal damage in the absence of reflux? BJU Int 2001;87:581-4. [PubMed]
- O’Brien WM, Gibbons MD. Pediatric urinary tract infections. Am Fam Physician 1988;38:101-12. [PubMed]
- Koff SA, Wagner TT, Jayanthi VR. The relationship among dysfunctional elimination syndromes, primary vesicoureteral reflux and urinary tract infections in children. J Urol 1998;160:1019-22. [PubMed]
- Lidefelt KJ, Erasmie U, Bollgren I. Residual urine in children with acute cystitis and in healthy children: assessment by sonography. J Urol 1989;141:916-7. [PubMed]
- Lee JH, Son CH, Lee MS, et al. Vesicoureteral reflux increases the risk of renal scars: a study of unilateral reflux. Pediatr Nephrol 2006;21:1281-4. [PubMed]
- Shimada K, Matsui T, Ogino T, et al. Renal growth and progression of reflux nephropathy in children with vesicoureteral reflux. J Urol 1988;140:1097-100. [PubMed]
- Smith EM, Elder JS. Double antimicrobial prophylaxis in girls with breakthrough urinary tract infections. Urology 1994;43:708-12. [PubMed]
- Snodgrass W. The impact of treated dysfunctional voiding on the nonsurgical management of vesicoureteral reflux. J Urol 1998;160:1823-5. [PubMed]
- Griffiths DJ, Scholtmeijer RJ. Vesicoureteral reflux and lower urinary tract dysfunction: evidence for 2 different reflux/dysfunction complexes. J Urol 1987;137:240-4. [PubMed]
- Medical versus surgical treatment of primary vesicoureteral reflux: report of the International Reflux Study Committee. Pediatrics 1981;67:392-400. [PubMed]
- McLorie GA, McKenna PH, Jumper BM, et al. High grade vesicoureteral reflux: analysis of observational therapy. J Urol 1990;144:537-40. [PubMed]
- Hodson CJ, Maling TM, McManamon PJ, et al. The pathogenesis of reflux nephropathy (chronic atrophic pyelonephritis). Br J Radiol 1975.Suppl 13:1-26. [PubMed]
- Roberts JA, Fischman NH, Thomas R. Vesicoureteral reflux in the primate IV: does reflux harm the kidney? J Urol 1982;128:650-2. [PubMed]
- Preda I, Jodal U, Sixt R, et al. Normal dimercaptosuccinic acid scintigraphy makes voiding cystourethrography unnecessary after urinary tract infection. J Pediatr 2007;151:581-4. [PubMed]
- Roberts JA, Suarez GM, Kaack B, et al. Experimental pyelonephritis in the monkey. VII. Ascending pyelonephritis in the absence of vesicoureteral reflux. J Urol 1985;133:1068-75. [PubMed]
- Godley ML, Ransley PG. Reflux and other ureteral abnormalities. In: Gearhart GP, Rink RC, Mouriquand PD, editors. Pediatric Urology. 2 ed. Saunders,2010:283-300.
- Hohenfellner K, Hunley TE, Brezinska R, et al. ACE I/D gene polymorphism predicts renal damage in congenital uropathies. Pediatr Nephrol 1999;13:514-8. [PubMed]
- al-Eisa A, Haider MZ, Srivastva BS. Angiotensin-converting enzyme gene insertion/deletion polymorphism and renal damage in childhood uropathies. Pediatr Int 2000;42:348-53. [PubMed]
- Kostić M, Stanković A, Zivković M, et al. ACE and AT1 receptor gene polymorphisms and renal scarring in urinary bladder dysfunction. Pediatr Nephrol 2004;19:853-7. [PubMed]


