
Efficacy and safety evaluation of the scrotal skin transfer method in the treatment of pediatric concealed penis: a six-month follow-up data
Highlight box
Key findings
• The scrotal skin transfer method shows remarkable efficacy without apparent complications and results in a penis that is fully exposed and aesthetically pleasing.
What is known and what is new?
• In pediatric concealed penis, the penis body is restricted in its ability to stretch. If not treated in a timely manner, it will affect penis development and the psychological health of children.
• Following a review of previous treatment experiences, we have adopted a new treatment method, namely, removing most of the inner foreskin plate and covering the missing skin on the ventral side of the penis with a scrotal skin transfer instead of the outer foreskin plate.
What is the implication, and what should change now?
• The surgical treatment of pediatric concealed penis by scrotal skin transfer instead of the outer foreskin plate method is a satisfactory surgical solution to the problem of limited skin on the outer plate of the concealed penis.
Introduction
Concealed penis, also known as buried penis, is a disease with congenital developmental anomaly, and the incidence was approximately 0.68% (1). It manifests as a short penis with a narrow foreskin mouth and an upward beak-like or dome-shaped appearance. The penises of patients are short at birth, with a tapered or “dome-shaped” appearance, and the exposed length of the penis at rest is less than 50% of the actual length of the penis body (2,3). The penis is hidden under the skin, but a normal-sized penis body can be seen when the skin of the penile root is pulled back, and it quickly retracts upon release (1,2). The penis body of concealed penis patients is developmentally normal but buried under the skin, with an excess of inner plate foreskin and insufficiency of outer plate foreskin.
In pediatric concealed penis, the penis body is restricted in its ability to stretch, and this will affect penis development and the psychological health of the child if not treated in a timely manner (4). Surgery is a common treatment for pediatric concealed penis. Up to now, there are various surgery approaches for concealed penis. Which technique is preferred and how to make improvements has been hotly debated among scholars in the field. Although there is no unified fixed surgical method for the concealed penis, the purpose of surgical is the same: that is to release the foreskin narrow ring, remove the fibrotic penile meatus tissue, make the penile body completely exposed, and solve the problem of lack of penile skin (5). However, most surgical methods tend to retain too much of the inner foreskin plate, leading to large differences in color between the inner and outer penile skin plates post-surgery, an unsatisfactory appearance, and complications such as penile retraction and recalcitrant foreskin edema (6). Meanwhile, the inner plate skin is prone to edema, and the swelling is slow or even impossible to resolve, resulting in foreskin bloating and a postoperative penile appearance with a “rubber band” effect (7,8), which seriously affects the aesthetics of the penis and the psychological health of the child (9).
After reviewing previous treatment outcomes, we have adopted a new method that involves removing most of the inner foreskin plate and covering the missing skin on the ventral side of the penis with a scrotal skin transfer instead of the outer foreskin plate. Our aim has been to protect and make use of the outer plate of the foreskin as much as possible and use less of the inner plate to avoid a significant difference in the color of the penis and to reduce postoperative foreskin recalcitrant edema, penile retraction, and other complications (10). In this study, we investigated the safety and efficacy of scrotal skin transfer method in the treatment of pediatric concealed penis. We present the following article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-22-852/rc).
Methods
Ethical statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Anhui Provincial Children’s Hospital (No. mr-34-21-010291) and informed consent was taken from all the patients’ guardians.
General information
Sixty children with concealed penis admitted to our department from June 2020 to June 2022 were selected for inclusion in this study. They were randomly divided into the Improved group (n=30) and General group (n=30). The inclusion criteria were as follow: (I) aged 3–9 years; (II) the children had a typical concealed penis; (III) children did not undergo surgery for concealed penis. The exclusion criteria were as follow: (I) genital system and genital anomalies, such as epispadias, cryptorchidism and hypospadias; (II) idiopathic small penis; (III) have the history of penile trauma; (IV) combination of other major systemic diseases.
Surgical method
Surgical procedures of General group
The children were treated with the traditional Shiraki procedure (11). Under the combined intravenous-inhalation anesthesia, the children were placed in supine position, routinely disinfected and draped, the foreskin orifice was bluntly dilated with vascular forceps, the foreskin was turned over to expose the glans, and the smegma was cleaned. The outer foreskin was then circumferentially cut along the orifice of the foreskin and an incision was made longitudinally at 2, 6 and 10 points on the inner foreskin and 4, 8 and 12 points on the outer foreskin, with attention to the length of the incision of the outer foreskin, the longest should be less than 1.5 cm, the proximal foreskin of the penis was dissociated to the root, the white membrane of the penis root subcutaneously was sutured and fixed, and finally the triangular skin flap insertion suture was performed.
Surgical procedures of Improved group
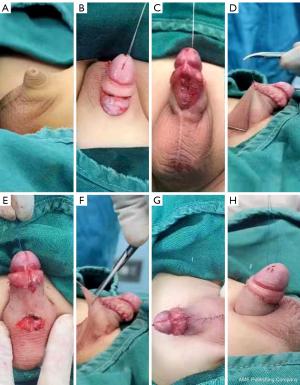
The patient was placed in a supine position after a combined intravenous and inhalation anesthesia (CIIA). Routine disinfection of the surgical site was performed, and sterile sheets were placed accordingly. The foreskin mouth was bluntly dilated with vascular forceps, the foreskin was turned over to expose the glans, and the prepuce was cleaned We made a circumferential incision of the penile skin at the junction of the inner and outer plates of the foreskin and a longitudinal incision of the skin at the 6 o’clock position on the ventral side of the penis toward the scrotum to release the narrow ring of penile skin. The skin of the penis was desheathed along the surface of Buck’s fascia to the penile root, and the abnormal fibrous connective tissue was excised. The skin of the external plate was left intact without excision, and the white membrane of the penis was sutured to the dermis of the penile root using 4-0 prolene sutures at the 2 and 10 o’clock direction dorsal to the penile root to shape the pubic angle of the penis. A circumferential incision of 5–8 mm from the coronal sulcus was made to remove all excess inner foreskin plate. The length of the incision was based on the circumference of one circle of the outer skin and the circumference of one circle of the retained inner foreskin, usually reaching the penile root. The inner and outer plate skin was intermittently sutured from the 12 o’clock position on the dorsal side of the penis to both sides with 5-0 absorbable thread until the inner and outer plate skin was sutured with tension (most of which corresponded to the 3 and 9 o’clock positions) and the missing outer plate skin on the ventral side was visible. The scrotal meatus and the penile space were appropriately dissected, and the top angle of the ventral external skin incision of the penis was lifted and sutured to the inner foreskin plate at the midline of the prepuce tether so that the scrotal skin could be lifted without tension to cover the ventral trauma of the penile body. The internal and external skin of the penis was intermittently sutured on both sides and the ventral side (the external skin being the scrotal skin that was lifted and transferred) at the 6 o’clock position, at which time the scrotal skin was pulled up and shaped like a webbed penis. The webbed scrotal skin was incised transversely in full at the penile root, and the scrotum was subluxated. The scrotal subcutaneous tissue was fixed to the white membrane of the penile root with 4-0 prolene sutures to shape the scrotal angle of the penis. The scrotal skin on the ventral side of the penis was resected, and the scrotal incision was closed longitudinally to cover the ventral trauma of the penis and form the penile scrotal angle, which enabled the length of the penis to be fully exposed. After surgery, the penis appeared similar to a post-circumcision penis. Figure 1 is display the surgical steps. Operative time and incision bleeding volume of all patients were collected.
Postoperative treatment
After surgery, a catheter was routinely left in place, and a penile elastic bandage was used with moderate pressure. After 3–5 days, the dressing and catheter were removed, and the local skin was kept dry and clean until the wound was completely healed.
Observation indicators
Before surgery, we collected the clinical information including age and penile length. During surgery, the operation duration and the amount of surgical bleeding were recorded. The post-operative penile length and of children in both groups were also observed and compared. The penile lengthening length was calculated by subtracting the pre-operative length from the post-operative length.
Follow-up
All patients were followed up at 6 months’ post-surgery by outpatient interview. The postoperative complications (penile retraction, penile skin edema), postoperative penile appearance and length, and degree of parental satisfaction were collected during follow-up. The questionnaires were applied to collected the penile appearance and degree of parental satisfaction. Follow-up questionnaires were jointly completed by doctors and parents of patients.
Statistical analysis
SPSS 20.0 was used for statistical analysis. The data was expressed as mean ± standard deviation (SD). The age of patients was expressed in median. T-test was used for the comparison between groups. The comparison of the intergroup enumeration data used chi-square test (α=0.05). P<0.05 indicates statistical difference.
Results
The clinical baseline characteristics of patients
The children in the improved group were aged from 3 to 8 years and 7 months, the median age was 5 years and 9 months, the preoperative penis length were 1.5±0.5 cm. In the General group, children were aged from 3 years to 9 years and 3 months, the median age was 6 years, preoperative penis length were 1.6±0.5 cm. There was no statistically significant difference between the two groups in terms of age and preoperative penis length (P>0.05).
Comparison of penile length between two groups
There was no statistically significant difference in the penile length between the General and Improve groups before surgery (P>0.05). The two different operations significantly increase penis length of children (P<0.05). Compared with General group, the post-operative penis length and the penile lengthening length in Improve group was significantly increased (P<0.05) (Table 1).
Table 1
| Group | Pre-operative penis length (cm) | Post-operative penis length (cm) | Penile lengthening length (cm) |
|---|---|---|---|
| Improved group (n=30) | 1.5±0.5 | 4.3±0.6* | 2.8±0.5 |
| General group (n=30) | 1.6±0.5 | 3.7±0.7* | 2.1±0.4 |
| P | 0.4417 | 0.007 | <0.0001 |
Data are presented as mean ± standard deviation. *, P<0.05 vs. pre-operative penis length.
Comparison of surgical indicators and complications between two groups
The operation duration of the Improved group was shorter than that of the General group (P<0.05). There was no significant difference in the amount of surgical bleeding between the two groups (P>0.05) (Table 2).
Table 2
| Group | Average operation duration (min) | Bleeding amount (mL) | Penis retraction | Foreskin severe edema | Incision infection | Penis skin discoloration | Complication rate |
|---|---|---|---|---|---|---|---|
| Improved group (n=30) | 22.7 | 4.5±2 | 0 | 2 | 0 | 0 | 2 (0.07%) |
| General group (n=30) | 26.4 | 5±2 | 1 | 7 | 0 | 11 | 19 (0.63%) |
Data are presented as mean ± standard deviation, n, or n (%).
Among the 60 children with concealed penis, the surgical incision was completely healed after 6 months of follow-up. The children in the Improved group had no residual circumcision constriction ring, the scrotal angle of the penis and the pubic angle of the penis were completely established, the penile body was all exposed, and there was no obvious color difference of the penile skin. The appearance of the penis resembled that after circumcision, with an aesthetic appearance and a high parental satisfaction.
In the Improved group, no complications including penis retraction, incision infection and penis skin discoloration was observed, and two cases presented with edema (Table 2). In General group, one patient had penile retraction, 7 patients had edema, and 11 patients had penis skin discoloration. The complication rate in Improve group was lower than that in General group (Table 2).
Discussion
Concealed penis is a pediatric urological disease, mainly caused by embryonic penile skin membrane dysplasia fibrosis and abnormal attachment to the distal penile body. Pulling the penis causes penile body retraction and concealment, affecting the development of the penile skin and resulting in the penis being “curled up” under the skin (12,13). Concealed penis often requires surgery, but the timing of surgery is contentious. Based on previous clinical experience, school age was the best time for concealed penis surgical treatment (14,15). In this study, we designed a novel surgical method for concealed penis based on the past surgical experience and reference to the previous study (16). 3–9 years old children with concealed penis were performed scrotal skin transfer, and achieved good therapeutic effect.
Currently, there are various surgery approaches for concealed penis, and no unified fixed surgical method in the treatment. However, these methods often leave too much inner foreskin plate, and are prone to complications such as edema, resulting in foreskin bloating and a postoperative penile appearance with a “rubber band” effect (7,8). In this study, our aim was to protect and make use of the outer plate of the foreskin as much as possible and use less of the inner plate to avoid a significant difference in the color of the penis and to reduce postoperative complications. The effects of this method were similar to the circumcision. The improved surgical method did not observe the difference of penis color, penile retraction and infection during the follow-up. But 2 cases developed edema, swelling resolved at follow-up.
The treatment of concealed penis should not only meet the functional needs of the patient but also be aesthetically pleasing postoperatively (17,18). Our surgical approach for concealed penis perfectly solves the problems, including shortage of outer foreskin plate, postoperative edema of the inner foreskin plate, and the large difference in color of the inner and outer foreskin plates. We keep all the skin of the outer plate of the foreskin. Meanwhile, we use a scrotal septum skin transfer below the penile root to replace the skin tissue of the ventral side of the penis. Only one circle of the inner plate of the foreskin is left, with the width of circumcision about 5–8 mm. This technology can solve the problems of skin shortage on the outer plate of the penis, and the color difference. Given the skin texture, color and hairiness, the cosmetic results associated with some scrotal skin transfers may be poor. We selected scrotal skin with a similar color to the ventral skin of the penis for transplant. The ventral side of the penis is not a visual surface and not easily visible. In addition, a small amount of hair does not affect the appearance of the penis, because it is a common phenomenon in normal adults. If the patients have a large amount of hair on the ventral side of the scrotum after development, laser hair removal can completely achieve the effect to inhibiting the growth of hair.
The development of penis involves appearance and function. Our method ensured the consistency of skin color, and the difference of skin color will be further weakened with the development of patients. The operation did not affect the function of the penis, but only lengthened the length of the penis from the appearance. This improved method establish a good penile scrotal angle and penile pubic bone angle so that the penile body is completely exposed. Additionally, the suture fixation of the subcutaneous tissue at the dorsal penile root with the penile white membrane ensures a good penile pubic angle and not only allows the complete exposure of the penile body but also prevents the retraction of the penis, reduces postoperative complications, and has an aesthetically pleasing appearance. In Improved group, the penis length of patients after surgery were increased significantly, and no patients presented with penile retraction. It displayed that the improved surgical method significantly prolongs the length of the penis.
We conclude that the following points should be noted for this procedure: (I) the outer plate skin should not be incised but retained, and the inner plate skin should be retained only in a circle of 5–8 mm from the coronal sulcus, without using the inner plate skin to cover the penile body to reduce the possibility of postoperative foreskin bloating. (II) The length of the scrotal midline split should be such that the circumference of the outer plate circle is the same as the circumference of the retained inner plate circle of the foreskin to ensure that the inner plate skin is aligned with the outer plate skin and has an aesthetic appearance. (III) The scrotal skin can be pulled up without tension to cover the ventral side of the penile body. (IV) The penile scrotal angle can be formed by transverse incision and longitudinal suturing, but attention should be paid to the width of the transverse incision; if the transverse incision is too wide, a narrow ring will be formed after longitudinal suturing, causing edema; if the transverse incision is too short, the penile scrotal angle will not be established perfectly, and the penis will easily retract. At the same time, the ventral scrotal subcutaneous tissue should also be fixed with the ventral white membrane of the penis by suturing, which is conducive to the establishment of the penile scrotal angle and prevents the penis from retraction. (V) Fixing the dorsal penile subcutaneous tissue to the penile white membrane must be done at the penile root to establish a good penile pubic angle and fully reveal the penis. This study also has some limitations. Because some patients were included in the study for a short time, we only have complete data of 6 months follow-up. The long-term outcomes of surgery were lack. The follow-up procedure is still in progress. We will continue to observe the effect of surgery in the later stage. Second, the sample size was small in our study. We expect to expand the sample size in the following study.
Conclusions
In conclusion, the surgical treatment of pediatric concealed penis by scrotal skin transfer instead of the outer foreskin plate method is a satisfactory solution to the problems of limited skin on the outer foreskin plate, significant differences in color between the inner and outer plates, foreskin edema, unsatisfactory penile exposure, and penile retraction.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-22-852/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-22-852/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-22-852/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-852/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of the Anhui Provincial Children’s Hospital (No. mr-34-21-010291) and informed consent was taken from all the patients’ guardians.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Li Y, Zhu XY, Feng DC, et al. A new measurement method for the diagnostic of different types of concealed penis in children. Iran J Pediatr 2020;30:1032-6. [Crossref]
- Xu A, Li X, Zhang Z, et al. Comparison of pedicled skin flap of foreskin for phalloplasty and Sugita surgical method in treatment of complete concealed penis. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2020;34:1423-8. [PubMed]
- Wang Z, Zhou G, Yang Z, et al. Application of Pediatric Penile Perception Scale in follow-up evaluation after occult penis. J Clin Urol 2022;37:436-9.
- Tang Star. Focus on the psychological factors in the treatment of hidden penis in children. Journal of Clinical Pediatric Surgery 2018;17:891-3.
- Liu F, Lin T, He D, et al. New Technique for the Treatment of Buried Penis in Children. Urology 2016;88:166-9. [Crossref] [PubMed]
- Li XL, Gong YB, Lin T. Diagnosis and surgical treatment of buried penis in children. Chinese Journal of Pediatric Surgery 1996;17:215-7.
- Hao W. Investigation and analysis of the occurrence of postoperative complications in 96 children with occult penis. Contemporary Medicine Theory Cluster 2020;18:71-2.
- Qi C, Zhang T, Chu D, et al. Application of the "button method" for dorsal flap flap transfer in children with severe occult penis. The Chinese Journal of Pediatric Surgery 2021;42:345-9.
- Gao Z. Progress in the diagnosis and treatment of the occult penis. The Chinese Journal of Male Science 2021;35:73-5, 80.
- Yin W, Wang G, Wu K. Analysis of the advantages of reducing postoperative foreskin edema. Chinese Journal of Male Science 2019;25:901-4.
- Shiraki IW, Shirai RS. Congenital micropenile skin sleeve. J Urol 1975;114:469-72. [Crossref] [PubMed]
- The Male Science Branch of the Chinese Medical Association. The Chinese expert consensus on the diagnosis and treatment of occult penis in children. The Chinese Journal of Male Science 2021;27:941-7.
- Yao X, Liu X. Etiology and treatment advances in children with an occult penis. Clinical Medical Research and Practice 2020;5:190-2.
- Yang Y, Xu Z. Controversy and research progress of occult penis surgery and follow-up. Journal of Clinical Pediatric Surgery 2018;17:881-5.
- Zampieri N, Camoglio F. Pediatric-adolescent andrology: Single centre experience. Arch Ital Urol Androl 2020;92: [Crossref] [PubMed]
- Huang SS, Zhang QM, Wan XD. Curative effect of scrotal flap on adult concealed penis. The 16th Andrology Academic Conference of the China Association of Chinese Medicine 2016:1042-3.
- Hu Y, Xu B, Cai B, et al. Efficacy of modified Borsellino in occult penis. Chinese Journal of Pediatric Surgery 2021;42:435-8.
- Zhang YF, Cheng C, Liu Y, et al. Application of Plastic Surgery in Andrology Penile Surgery. Chinese Medical Journal 2020;100:1681-3. [PubMed]


