
The safety and effectiveness of laparoscopic anterior sacral ligament suspension combined with dome suspension in the treatment of bladder prolapse after hysterectomy: a retrospective cohort study
Highlight box
Key findings
• Laparoscopic anterior sacral ligament suspension combined with dome suspension (L-ASLS + DS) effectively treats bladder prolapse after hysterectomy, reduces the incidence of postoperative complications, improves the cure rate and safety, and is worthy of comprehensive clinical application.
What is known and what is new?
• L-ASLS + DS and transperineal whole pelvic floor reconstruction (T-WPFR) can both be used totreat bladder prolapse after hysterectomy.
• L-ASLS + DS outperformed T-WPFR in terms of the perioperative indicators, and the incidence of postoperative complications in the L-ASLS + DS group was significantly lower than that in the T-WPFR group.
What is the implication, and what should change now?
• To better treat patients with bladder prolapse after hysterectomy, L-ASLS + DS should be chosen, as it has better efficacy and safety than T-WPER.
Introduction
Bladder prolapse is a kind of pelvic organ prolapse (POP), defined by the herniation of the bladder into the vagina (1). Bladder prolapse is a common complication after hysterectomy. It can cause urinary incontinence (UI), voiding dysfunction, fecal incontinence, incomplete defecation, and sexual dysfunction, and thus can have a significant effect on patients’ quality of life (2,3). However, only a few treatment methods are available for bladder prolapse, most of which have unsatisfactory long-term efficacy and safety (4). Currently, reconstruction surgery is the most effective way to treat hysterectomy-induced bladder prolapse (5). The surgery can be performed using transperineal, laparoscopic, or open approaches (6). Doctors often choose transperineal pelvic floor reconstruction to treat hysterectomy-induced bladder prolapse, but it has a number of inevitable complications, such as massive bleeding, dysuria, and overactive bladder, and a relatively high recurrence rate (7-9).
The Urology Department of Shanxi Provincial People’s Hospital first introduced a laparoscopic approach that used anterior sacral ligament suspension combined with dome suspension to treat patients with bladder prolapse after hysterectomy in 2011. Compared to traditional whole pelvic floor reconstruction, this laparoscopic method reduces the complications and increases overall safety. Thus, we sought to evaluate the efficacy and safety of the 2 different surgical methods from the perioperative outcomes using 1-year follow-up data to determine if laparoscopic anterior sacral ligament suspension combined with dome suspension (L-ASLS + DS) was a better surgical procedure for treating hysterectomy-induced bladder prolapse. We present the following article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-50/rc).
Methods
Study design and setting
This was a retrospective cohort study. Patients who had undergone a hysterectomy at the Department of Urology of Shanxi Provincial People’s Hospital from January 2011 to January 2022 were included in this study. Based on the inclusion and exclusion criteria, 146 patients were selected for this study. All patients had bladder prolapse more than 3 degrees after hysterectomy, and all received surgical treatment. We used either L-ASLS + DS or transperineal whole pelvic floor reconstruction (T-WPFR) method. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Shanxi Provincial People’s Hospital (2021 Provincial Medical Science Ethics Review No. 376) and informed consent was taken from all the patients.
Patient selection
The 146 patients included in this study were treated for bladder prolapse after hysterectomy at the Urology Department of Shanxi Provincial People’s Hospital from January 2011 to January 2022. Patients were divided into study group and control group by voluntary means or economic reasons.
To be eligible for inclusion in this study, patients had to meet the following inclusion criteria: (I) be aged between 20–85 years; (II) have a POP quantitative score of grade 3 or above; (III) have undergone a hysterectomy before at least 6 months; and (IV) have undergone a urodynamic examination that showed bladder detrusor pressure of ≥50 cmH2O. Patients were excluded from the study if they met any of the following exclusion criteria: (I) had not undergone a hysterectomy; (II) had received at least 1 pelvic floor operation other than hysterectomy within the last 6 months; (III) was suffering from a gynecological or urinary malignancy; (IV) had received radiotherapy or chemotherapy to treat pelvic floor disease; (V) had a urogenital tract infection; (VI) had received tolterodine or local estrogen treatment within the last week, or had received a non-drug treatment, such as vaginal POP or electrical stimulation; (VII) had restricted activity (e.g., could not walk, run, or climb stairs); (VIII) had other diseases that may adversely affect the function of the lower urethra, including uncontrollable diabetes, multiple sclerosis, Parkinson’s disease, spinal cord injury, cauda equina injury, or multiple system atrophy; (IX) was a pregnant or lactating women; and/or (X) was suffering from a severe autoimmune disease.
Operation procedure
In the control group, the routine T-WPFR was performed strictly according to the guidelines for the clinical reconstruction of the entire pelvic floor, so as to treat bladder prolapse caused by hysterectomy. Conversely, the L-ASLS + DS was employed in the study group to treat hysterectomy-induced bladder prolapse.
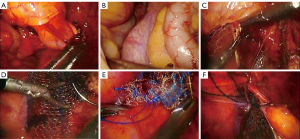
For the L-ASLS + DS procedure, after successful anesthesia, the patient was placed in the bladder amputation position. Routinely, the urinary catheter was retained, standard disinfection was performed, sheets were spread out, and the vagina was sterilized. Alice forceps (2 pairs) were used to lift the highest point of the dome in the upper and lower directions, the dome gap was filled with water (250 mL saline + 1 mL adrenaline), the membrane of the dome was cut crosswise, and the membrane of the walls on both sides of the dome was lifted. Next, the bladder was pushed up to separate the bladder gap, and the retroflexed peritoneum of the bladder was cut. Afterwards, the posterior dome was opened by clamping and pulling the dome. The rectum retroperitoneal fold was then opened by pushing down the rectum. A mesh patch, which had been cut into 2 5-by-3 cm pieces, was then sewed into the upper and lower spaces, and the joint of the higher patch was folded into the abdominal cavity. At this point, the skin was cut 10 cm above the umbilicus, where the laparoscopy was inserted, and 5- and 10-mm puncture holes for the Trocar were made in the left lower abdomen. The patch at the lower point of the abdominal cavity was identified under a microscope, and a posterior clamp was used to make a mark. Next, the anterior sacral ligament on the right side was located. The peritoneum was opened along the path from the anterior sacral ligament to the lowest point of the anterior basin. The upper end of the patch was fixed on the right anterior sacral ligament with a 4-0 micro suture line, flattened, and trimmed. Finally, the peritoneum was closed with 4-0 micro lines, a tube was left, and each hole was sutured (Figure 1).
Recorded data
All the selected patients were followed up at 3, 6, and 12 months. The incidence of postoperative complications (including the recurrence of bladder prolapse, bladder overactivity, urination difficulty, the mesh rejection, and mesh erosion) were compared between the 2 groups.
Statistical analysis
SPSS 25.0 software was used for the statistical analysis. The descriptive data are shown as mean ± standard deviation, number (percentage) or median (interquartile spacing). and chi-square test was used for comparison of measurement data using independent sample T test technology data components, and the Students’t test was used for comparisons. The measured data are expressed as the number of cases (n) and the percentage of total patients (%). P<0.05 indicated statistically signiffcant differences.
Results
Patient information
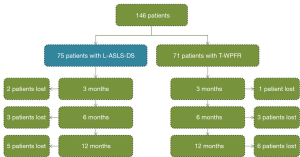
In total, 146 patients were selected for inclusion in this study from January 2011 to January 2018. Among the patients, 75 were designated to the study group that received the L-ASLS + DS treatment, and 71 were designated to the control group that received T-WPFR treatment. The patients in the study group had an average age of 63.17±9.38 years (range, 45–82 years), and the patients in the control group had an average age of 62.01±9.45 years (range, 46–80 years). There was no significant difference between the 2 groups in terms of age (P>0.05) (see Table 1). In the control group, 2, 3, and 5 patients were lost to the follow-up at the 3-, 6-, and 12-month timepoints, respectively. In the study group, 1, 3, and 6 patients were lost to the follow-up at the 3-, 6-, and 12-month timepoints, respectively (see Figure 2).
Table 1
| Variables | Study group (N=75) | Control group (N=71) | t/χ2/Z | P |
|---|---|---|---|---|
| Age (years) | 63.17±9.38 | 62.01±9.45 | 0.744 | 0.458 |
| Height (cm) | 161.76±4.84 | 162.49±4.76 | −0.922 | 0.358 |
| Body weight (kg) | 68.24±8.54 | 69.07±8.18 | −0.599 | 0.550 |
| Smoking status | ||||
| No smoking | 68 | 68 | Fisher | 0.497 |
| ≤5 pieces/day | 5 | 3 | ||
| One bag a day | 2 | 0 | ||
| Coffee consumption | ||||
| ≤1 cup/day | 72 | 67 | 0.006 | 0.941 |
| >1 cup/day | 3 | 4 | ||
| Alcohol consumption | Fisher | 1.000 | ||
| No alcohol | 73 | 70 | ||
| Drinking occasionally | 1 | 0 | ||
| Alcohol | 1 | 1 | ||
| Age at first menarche (years) | 12.01±1.58 | 11.77±1.61 | 0.902 | 0.368 |
| Disease course (length) (years) | 4.00 (1.00, 5.00) | 5.00 (1.00, 6.00) | −0.776 | 0.438 |
| Age of pregnancy (years) | 22.94±2.95 | 23.45±3.56 | −0.909 | 0.365 |
| No. of deliveries (parity, parities) | 1.00 (1.00, 1.00) | 1.00 (1.00, 2.00) | −1.418 | 0.156 |
| No. of vaginal deliveries | 1.00 (1.00, 1.00) | 1.00 (1.00, 2.00) | −1.106 | 0.269 |
| No. of caesarean sections | 0.00 (0.00, 0.00) | 0.00 (0.00, 0.00) | −0.338 | 0.736 |
| Blood cell count and classification | ||||
| WBC (×109/L) | 7.05±1.89 | 7.31±1.72 | −0.849 | 0.397 |
| Hb (g/L) | 111.33±18.54 | 108.39±16.40 | 1.012 | 0.313 |
| PLT (×109/L) | 231.00 (195.00, 256.00) | 211.00 (185.00, 245.00) | −0.888 | 0.375 |
| Blood biochemistry | ||||
| ALT (U/L) | 32.88±5.29 | 30.63±3.55 | 0.939 | 0.349 |
| ALB (g/L) | 40.60±3.58 | 40.59±3.26 | 0.029 | 0.977 |
| BUN (mg/dL) | 5.16±1.27 | 5.26±1.08 | −0.512 | 0.609 |
| Cr (μmol/L) | 63.73±15.45 | 60.73±12.08 | 1.301 | 0.195 |
| Coagulation function | ||||
| APTT (s) | 28.90 (27.30, 31.90) | 29.60 (27.60, 32.30) | −0.903 | 0.367 |
| INR | 0.95 (0.89, 1.02) | 0.98 (0.91, 1.04) | −1.214 | 0.225 |
| TT (s) | 13.80 (12.90, 15.30) | 13.30 (12.40, 14.60) | −1.890 | 0.059 |
| Urine | ||||
| WBC (×109/L) | 7.00 (4.00, 52.00) | 6.00 (3.00, 16.00) | −1.669 | 0.095 |
| RBC (×109/L) | 6.00 (3.00, 8.00) | 6.00 (3.00, 23.00) | −0.636 | 0.525 |
| Urine protein | ||||
| 1-weakly positive | 1 | 3 | 0.317 | 0.574 |
| 2-negative | 74 | 68 | ||
| Bladder detrusor pressure (cmH2O) | 41.00 (30.50, 52.00) | 41.00 (26.50, 51.50) | −0.911 | 0.362 |
| Average urine flow rate (mL/s) | 13.40 (11.45, 16.70) | 15.60 (12.70, 18.50) | −1.886 | 0.059 |
| Maximum urinary flow rate (mL/s) | 16.50 (14.75, 19.70) | 17.50 (15.65, 21.65) | −1.304 | 0.192 |
| Maximum bladder volume (mL) | 300.00 (215.00, 345.00) | 300.00 (180.00, 300.00) | −1.303 | 0.193 |
| Residual urine volume (mL) | 0.00 (0.00, 15.00) | 0.00 (0.00, 0.00) | −1.475 | 0.140 |
| MUPP (cmH2O) | 37.83 (25.70, 43.72) | 35.76 (20.82, 41.45) | −1.718 | 0.086 |
| PdetQmax (cmH2O) | 37.20 (34.25, 44.00) | 36.60 (32.45, 42.00) | −1.500 | 0.134 |
Data are shown as mean ± standard deviation, number (percentage) or median (interquartile spacing). WBC, white blood cell; Hb, hemoglobin; PLT, platelet count; ALT, alanine aminotransferase; ALB, albumin; BUN, blood urea nitrogen; Cr, creatinine; APTT, activated partial thromboplastin time; INR, international normalized ratio; TT, thrombin time; RBC, red blood cell; PdetQmax, detrusor pressure at maximum flow velocity; MUPP, micturition urethral pressure measurement.
Perioperative results: L-ASLS + DS outperformed T-WPFR
The perioperative related indicators, including the operation time, intraoperative bleeding, and time to first urination, were compared between the 2 groups. The operation time of the study group was longer than that of the control group, and the intraoperative bleeding volume of the study group was less than that of the control group, and the differences were both statistically significant (P<0.05). Moreover, the time to first urination was earlier in the study group than the control group, and the difference was statistically significant (P<0.05) (Table 2). Thus, L-ASLS + DS had a better safety profile than T-WPFR in relation to the perioperative parameters.
Table 2
| Group | Control group (n=71) | Study group (n=75) | P |
|---|---|---|---|
| Operation time (min) | 63.66±14.39 | 121.55±15.26 | <0.001 |
| Bleeding volume (mL) | 218.45±42.28 | 64.73±30.57 | <0.001 |
| First micturition time after operation (h) | 50.07±8.02 | 15.49±8.05 | <0.001 |
Data are presented as mean ± standard deviation.
Long-term follow-up results: L-ASLS + DS outperformed T-WPFR
The postoperative complications were evaluated during the 1-year follow-up period. In the control group, there were 14 cases of recurrence, 5 cases of dysuria, 15 cases of detrusor instability, 14 cases of overactive bladder, 3 cases of infection, 16 cases of UI, 3 cases of mesh rejection, 1 case of mesh erosion, and no cases of embolism/thrombosis at the end of the 1-year follow-up period. In the study group, there were no cases of recurrence, no cases of dysuria, 2 cases of detrusor instability, 2 cases of overactive bladder, 1 case of infection, 2 cases of UI, no cases of mesh rejection, no cases of mesh erosion, and 1 case of embolism/thrombosis at the end of the 1-year follow-up period. Thus, comparing the 2 groups, the incidence of long-term postoperative complications (i.e., recurrence, dysuria, detrusor instability, overactive bladder, and UI) was significantly lower in the study group than the control group (P<0.05). However, there was no statistically significant differences in the rates of infection, mesh rejection, mesh erosion, or embolism/thrombosis between the 2 groups (Table 3).
Table 3
| Group | Control group (N=66) | Study group (N=69) | P |
|---|---|---|---|
| Recurrence, n (%) | 14 (21.2) | 0 (0.0) | <0.001 |
| Dysuria, n (%) | 5 (7.6) | 0 (0.0) | 0.020 |
| Detrusor instability, n (%) | 15 (22.7) | 2 (2.9) | <0.001 |
| Overactive bladder, n (%) | 14 (21.2) | 2 (2.9) | <0.001 |
| Infection, n (%) | 3 (4.5) | 1 (1.4) | 0,289 |
| Urinary incontinence, n (%) | 16 (24.2) | 2 (2.9) | <0.001 |
| Mesh rejection, n (%) | 3 (4.5) | 0 (0.0) | 0.073 |
| Mesh erosion, n (%) | 1 (1.5) | 0 (0.0) | 0.305 |
| Embolism/thrombosis, n (%) | 0 (0.0) | 1 (1.4) | 0.326 |
In relation the 3- and 6-month timepoints, the rates of dysuria, detrusor instability, overactive bladder, and UI differed significantly between the 2 groups from 6 months after the operation (P<0.05), and the rates of recurrence between the 2 groups differed significantly from 3 months after the surgery (P<0.05; Table 4).
Table 4
| Category | 3 months | 6 months | 12 months | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study group (N=75) | Control group (N=71) | Z | P | Study group (N=75) | Control group (N=71) | Z | P | Study group (N=75) | Control group (N=71) | Z | P | |||
| Recurrence of bladder prolapse | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 3 | 0 | 3 | ||||||||
| No | 74 | 69 | 72 | 65 | 69 | 63 | ||||||||
| Dysuria | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 3 | 0 | 4 | ||||||||
| No | 74 | 69 | 72 | 65 | 69 | 62 | ||||||||
| Detrusor instability | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 7 | 2 | 14 | ||||||||
| No | 74 | 69 | 72 | 61 | 67 | 52 | ||||||||
| Overactivity | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 7 | 2 | 14 | ||||||||
| No | 74 | 69 | 72 | 61 | 67 | 52 | ||||||||
| Infection | 0.000 | 1.000 | −0.408 | 0.683 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 2 | 1 | 1 | 1 | 3 | ||||||||
| No | 74 | 67 | 71 | 67 | 68 | 63 | ||||||||
| Stress UI after surgical procedure | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 3 | 0 | 3 | ||||||||
| No | 74 | 69 | 72 | 65 | 69 | 63 | ||||||||
| Urge UI after surgical procedure | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 7 | 2 | 14 | ||||||||
| No | 74 | 69 | 72 | 61 | 67 | 52 | ||||||||
| Mixed UI after surgical procedure | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 0 | 0 | 1 | 0 | 1 | ||||||||
| No | 74 | 69 | 72 | 67 | 69 | 65 | ||||||||
| Mesh rejection | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 1 | 0 | 1 | 0 | 2 | ||||||||
| No | 74 | 68 | 72 | 67 | 69 | 64 | ||||||||
| Mesh erosion | 0.000 | 1.000 | 0.000 | 1.000 | 0.000 | 1.000 | ||||||||
| Yes | 0 | 1 | 0 | 2 | 0 | 1 | ||||||||
| No | 74 | 68 | 72 | 66 | 69 | 65 | ||||||||
| Embolism or thrombosis | −0.775 | 0.439 | 0.000 | 1.000 | ||||||||||
| Yes | 1 | 0 | 0 | 0 | 1 | |||||||||
| No | 73 | 69 | 72 | 68 | 68 | |||||||||
In the safety analysis, there were 14 missing cases in total, and some cases had been lost at the beginning of the study. Therefore, in the effectiveness analysis, the data of the missing persons were treated with missing values. Rank combination test was used to compare the classification data. UI, urinary incontinence.
From the PFDI-20 [including: Pelvic Organ Prolapse Distress Inventory 6 (POPDI-6), Colorectal-Anal Distress Inventory 8 (CRAD-8) and Urinary Distress Inventory 6 (UDI-6)], we can see that the three scales are improving gradually with the passage of time, and the UDI-6 scale shows statistical significance between the two groups within 3 months after operation (P<0.05); however, POPDI-6 showed statistical significance between the two groups at 6 months after operation (P<0.05) (Table 5).
Table 5
| Time | Category | Study group (N=75) | Control group (N=71) | t/Z | P |
|---|---|---|---|---|---|
| Pre-operation | UDI-6 | 13.32±9.18 | 12.66±2.39 | 0.586 | 0.559 |
| POPDI-6 | 15.29±3.43 | 15.38±3.27 | −0.156 | 0.876 | |
| CRADI-8 | 17.96±2.83 | 18.08±2.90 | −0.263 | 0.793 | |
| 3 months | UDI-6 | 8.50±2.58 | 10.81±2.54 | −5.399 | <0.001 |
| POPDI-6 | 11.34±2.15 | 11.30±1.93 | 0.098 | 0.922 | |
| CRADI-8 | 13.66±2.19 | 13.42±2.47 | 0.620 | 0.536 | |
| 6 months | UDI-6 | 4.82±2.56 | 10.76±4.18 | −10.221 | <0.001 |
| POPDI-6 | 5.33±3.18 | 10.24±2.52 | −10.085 | <0.001 | |
| CRADI-8 | 8.28±3.77 | 8.57±2.15 | −0.566 | 0.573 | |
| 12 months | UDI-6 | 2.00 (1.00, 4.00) | 12.00 (8.75, 16.25) | −9.088 | <0.001 |
| POPDI-6 | 2.00 (1.00, 3.50) | 6.00 (5.00, 7.00) | −8.232 | <0.001 | |
| CRADI-8 | 3.00 (2.00, 4.00) | 8.00 (5.00, 10.00) | −6.866 | <0.001 |
In the effectiveness analysis, there were 11 missing cases, accounting for about 7% of the study population. Therefore, in the effectiveness analysis, the data of the missing persons were processed with missing values. The mean ± standard deviation was used for the normal distribution data, the independent sample t-test was used for the comparison, the P50 (P25, P75) was used for the non-normal distribution data, and the rank combination test was used for the inter-group comparison. POPDI-6, Pelvic Organ Prolapse Distress Inventory 6; CRAD-8, Colorectal-Anal Distress Inventory 8; UDI-6, Urinary Distress Inventory 6.
Discussion
Bladder prolapse is a common complication after hysterectomy, and has troubled many urologists and gynecologists in recent years. Currently, there are few clinical treatments for this disease, and the treatment effects are poor. Many doctors use transperineal pelvic floor reconstruction to treat bladder prolapse after hysterectomy, but the effect is poor, and the complications are many. In 2011, the Urology Department of Shanxi Provincial People’s Hospital began to perform laparoscopic anterior sacral ligament suspension combined with fornix suspension to treat patients with bladder prolapse after hysterectomy. The surgical effect was good and compared to traditional pelvic floor reconstruction, the complications were greatly reduced and the safety was increased. This study compared the characteristics, efficacy, and safety of the 2 different surgical methods to determine the more appropriate surgical method for treating bladder prolapse after hysterectomy.
Whole pelvic floor reconstruction surgery through the perineum is a traditional standard operation method for treating POP, among other surgical treatments. Whole pelvic floor reconstruction suspends the prolapsed pelvic organ at the anatomical level (10). However, for patients with bladder prolapse after hysterectomy, the reconstruction of the pelvic floor through the perineum has a number of apparent disadvantages. First, compared to the uterine wall, the bladder wall is thinner and has greater flexibility, and bladder rupture during the operation is highly likely (11). Second, patients who receive traditional perineal whole pelvic floor reconstruction are prone to have postoperative overactive bladder, as the operative area is closer to the bladder wall (12). Third, urinary retention often occurs when the mesh is placed near the bladder. Fourth, bladder suspension is prone to ureteral injuries, such as distortion and obstruction, caused by indwelling mesh (13). Forth, the traditional pelvic floor reconstruction changes the vaginal axis to a certain extent, resulting in many complications.
The suspension dome is the crucial point of the L-ASLS + DS surgery, the traditional repair surgery only suspends the bladder through the perineal route, and the suspension force and force point are limited. The use of laparoscopic technology is to suspend the prolapsed bladder from the highest point, so the suspension force and force point are stronger than the traditional repair surgery. The traditional T-WPFR operation involves changing the vaginal axis, which results in complications, such as postoperative bleeding, sexual intercourse pain, pelvic pain and overactivity of the bladder (14). However, in L-ASLS + DS, the dome is suspended and sutured under the direct vision of a laparoscope, which significantly reduces the damage to the surrounding soft tissues, such as the rectum, blood vessels, and nerves, during the fixation of the anterior ligament of the sacrum (15), and is more conducive to the restoration of anatomical reduction of various organs in the pelvic cavity, and the operation has little impact on the detrusor of the bladder, thus reducing mesh erosion and the occurrence of overactivity of the bladder. During the suturing process, it is recommended that the following procedures be adopted: (I) suspend about 2/3 of the thickness of the anterior sacral ligament, with a needle distance of about 1 cm, suture 2 to 3 needles, and determine whether it is firm by traction; (II) use a right anterior sacral ligament suture. This effectively avoids the interference of the descending colon and rectum so that the surgeon can operate better and will not affect the recovery of the typical structure of the dome; (III) use the “Y” mesh to fix the right sacro anterior ligament at the top of the mesh confluence combined with the suspension. This maintains the tension-free state of the suspension path due to the elasticity in the retroperitoneum, maintains the bladder range of motion to the greatest extent, and allows the bladder and vault to be anatomically reduced with the help of the sacro anterior ligament; and (IV) during the operation, ensure that the suture is close to the right sacrum, and away from the right ureter, and the sacro anterior ligament is suspended. By folding the ureter at an angle, the hydronephrosis on the right side can be effectively reduced. In addition, anterior sacral ligament suspension can maintain the appropriate degree of relaxation, and effectively prevent an increase in the vaginal wall tension and sexual intercourse pain after pelvic floor reconstruction (16). We suspended and sutured the fornix under the direct vision of laparoscope to greatly reduce the damage to bladder, rectum, blood vessels, nerves and other surrounding soft tissues during the fixation of anterior sacral ligament, so as to ensure the stability and accuracy of suspension and reduce the occurrence of complications.
This study had some limitations. First, of the 146 patients enrolled in the study, 20 patients withdrew. Second, the abscission rate was high. Third, it was a retrospective study. Due to the limitation of the study time, further time is needed to observe the long-term effects of the 2 surgical methods. In the future, we intend to focus on the long-term changes in the indicators by improving the observation timepoints or extending the observation time. We also intend to include more comprehensive evaluation indicators and provide more detailed reports.
Conclusions
The treatment of bladder prolapse after hysterectomy is complicated; thus, the selection of an appropriate, effective, and safe surgical method is essential. The 2 methods (i.e., L-ASLS + DS and T-WPFR) used in this study both followed the guidelines and principles for pelvic floor reconstruction and employed the ligaments and fascia as supporting structures to reconstruct the pelvic floor (17). However, L-ASLS + DS is a minimally invasive approach and has a higher efficacy and safety than the T-WPFR, and is thus worthy of more comprehensive clinical application in the future.
Acknowledgments
Funding: The study was funded by the Pair-Up Assistance Cooperation Project of the Health Committee of the Sixth Division of Xinjiang Production and Construction Corps, Screening and Prevention of Female Pelvic Floor Dysfunction Diseases (No. 202104041101035).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-50/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-50/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-50/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-50/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was performed in accordance with the principles of the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of the Shanxi Provincial People’s Hospital (2021Provincial Medical Science Ethics Review No. 376), and informed consent was taken from all the patients
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn 2010;29:4-20. [Crossref] [PubMed]
- Haylen BT, Maher CF, Barber MD, et al. An International Urogynecological Association (IUGA) / International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J 2016;27:165-94. [Crossref] [PubMed]
- Xie J, Li S, Yao T, et al. A 2D equivalent mechanical model of the whole pelvic floor and impairment simulation. Int J Numer Method Biomed Eng 2022; Epub ahead of print. [Crossref] [PubMed]
- Matsuo K, Fullerton ME, Moeini A. Treatment patterns and survival outcomes in patients with cervical cancer complicated by complete uterine prolapse: a systematic review of literature. Int Urogynecol J 2016;27:29-38. [Crossref] [PubMed]
- de Tayrac R, Antosh DD, Baessler K, et al. Summary: 2021 International Consultation on Incontinence Evidence-Based Surgical Pathway for Pelvic Organ Prolapse. J Clin Med 2022;11:6106. [Crossref] [PubMed]
- Meister MR, Sutcliffe S, Ghetti C, et al. A pilot trial of movement-based pelvic floor physical therapy to address pelvic floor myofascial pain and lower urinary tract symptoms. Int Urogynecol J 2022; Epub ahead of print. [Crossref] [PubMed]
- Braun NM, Andraos W, Bettin S. Safety and efficacy of spider anchoring device for apical repair in laparoscopic sacrocolpopexy: Retrospective cohort study. Eur J Obstet Gynecol Reprod Biol 2019;235:88-92. [Crossref] [PubMed]
- Linder BJ, Occhino JA, Habermann EB, et al. A National Contemporary Analysis of Perioperative Outcomes of Open versus Minimally Invasive Sacrocolpopexy. J Urol 2018;200:862-7. [Crossref] [PubMed]
- de Boer TA, Salvatore S, Cardozo L, et al. Pelvic organ prolapse and overactive bladder. Neurourol Urodyn 2010;29:30-9. [Crossref] [PubMed]
- Meriwether KV, Antosh DD, Olivera CK, et al. Uterine preservation vs hysterectomy in pelvic organ prolapse surgery: a systematic review with meta-analysis and clinical practice guidelines. Am J Obstet Gynecol 2018;219:129-146.e2. [Crossref] [PubMed]
- Villot A, Pizzoferrato AC, Longie A, et al. Technical considerations and mid-term follow-up after vaginal hysterocolpectomy with colpocleisis for pelvic organ prolapse. Eur J Obstet Gynecol Reprod Biol 2020;247:73-9. [Crossref] [PubMed]
- Practice Bulletin No. 176: Pelvic Organ Prolapse. Obstet Gynecol 2017;129:e56-72. [Crossref] [PubMed]
- Yurteri-Kaplan LA, Meyn L, Moalli PA, et al. Outcomes of Pessary Use at 1 Year in Women Treated for Pelvic Organ Prolapse in a Large Multicenter Registry: Developed by the Pelvic Floor Disorders Registry. Urogynecology (Phila) 2022;28:800-10. [PubMed]
- Jacquetin B, Hinoul P, Gauld J, et al. Total transvaginal mesh (TVM) technique for treatment of pelvic organ prolapse: a 5-year prospective follow-up study. Int Urogynecol J 2013;24:1679-86. [Crossref] [PubMed]
- Dai Z, Li C, Wang X, et al. A new laparoscopic technique of inguinal ligament suspension for vaginal vault prolapse. Int J Surg 2017;43:131-6. [Crossref] [PubMed]
- Rogers RM, Pasic R. Pelvic Retroperitoneal Dissection: A Hands-on Primer. J Minim Invasive Gynecol 2017;24:546-551. Erratum in: J Minim Invasive Gynecol 2017;24:879. [Crossref] [PubMed]
- Paramasivam S, Proietto A, Puvaneswary M. Pelvic anatomy and MRI. Best Pract Res Clin Obstet Gynaecol 2006;20:3-22. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


