
Bilateral epididymal tuberculosis causing abscess formation and male infertility: a case report and literature review
Highlight box
Key findings
• Bilateral epididymal tuberculosis may cause severe complications, particulary infertility, in young males.
What is known and what is new?
• Epididymal TB is a rare disease that is difficult to diagnose due to similarities with other epididymo-testicular diseases and low sensitivity and specificity of diagnostic tools except for histopathological examination.
• Infertility is rare but important among subsequent complications caused by epididymal TB, particularly in young males. We emphasize that physicians should consider the possibility of epididymal TB in patients with persistent testicular symptoms to prevent subsequent complications, particularly infertility in young males.
What is the implication, and what should change now?
• When a definitive diagnosis of epididymal TB is established, or clinically suspected, immediate treatment initiation, including pharmacological and, if needed, surgical treatment, should be performed.
Introduction
Tuberculosis (TB) is a systemic disease caused by the acid-fast bacillus Mycobacterium tuberculosis. Mycobacterium tuberculosis invades the human body through inhaling the bacillus, which makes the lungs the most common site to develop active TB. When the primary infection is not cured or develops into a latent form, the bacillus can spread to other organs or tissues in the body through blood or lymphatic circulation, which results in extra-pulmonary manifestations. Extra-pulmonary TB occurs with an incidence of approximately 20–25% of all TB cases (1,2).
The genitourinary tract is known to be the second most frequently involved site in extra-pulmonary TB after the lymph nodes, which is the most commonly involved site. A previous study has reported that kidneys are the most common site involved in genitourinary TB; however, other organs in the genitourinary tract can also be involved with the disease (2). Epididymal TB is an uncommon form of TB; however, it is known to develop frequently in the male reproductive system (3). Epididymal TB may occur without the involvement of other organs. A previous study has reported that most TB cases developed in the scrotum did not have active pulmonary TB infection (4). Similarly, another study has reported that the involvement of other organs with TB was present in 12.3% of patients diagnosed with TB epididymo-orchitis (5).
Additionally, it is difficult to differentiate epididymal TB from other epididymo-testicular diseases, such as nonspecific bacterial epididymitis, orchitis, or epididymis neoplasia, due to the similarity of clinical symptoms among these diseases. Moreover, initial TB infection may develop into a latent form for up to 30 years before clinical manifestations develop in extra-pulmonary organs (6,7). These factors can make the diagnosis of epididymal TB difficult or often late, leading to inadequate treatment or missing the time for management.
Identifying acid-fast bacilli (AFB) or chronic granulomatous inflammation with amorphous caseous necrosis in the epididymal tissues can make the definitive diagnosis of epididymal TB (8,9). Although other methods are broadly used in diagnosing genitourinary TB, their limitations include the long period needed for the result and low sensitivity (10,11). Polymerase chain reaction (PCR) has become another useful option for genitourinary TB diagnosis; however, the accuracy is not totally reliable (11,12).
Epididymal TB care is initiated with pharmacological treatment involving a combination of anti-TB drugs for 6 to 9 months (9,10,13). However, surgical treatment should be considered in severe disease status (2,14).
Improper or late management of epididymal TB may worsen the disease, causing several complications, including cutaneous fistulas, abscess formation, extensive testis involvement, sexual dysfunction, or infertility, particularly in young males (4,5). We report a rare case of a young patient lately diagnosed with bilateral epididymal TB causing male infertility. We recommend considering the possibility of epididymal TB in patients presenting with testicular symptoms for a timely diagnosis and treatment. We present this case in accordance with the CARE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-22-728/rc).
Case presentation
A 37-year-old patient presented with left testicular pain and swelling, which was present for approximately 8 months. He had previously been treated with antibiotics in several medical facilities for suspected bacterial epididymitis; however, the symptoms worsened over time. Moreover, he reported having intermittent fever for several weeks. The patient did not report trauma history to the scrotum or any urethral discharge and had been with a single sexual partner. He did not have any comorbidities, including pulmonary TB. Additionally, he was married but did not have children and was worried about infertility.
Physical examination revealed a firm and tender mass, which was palpable in the area of the left epididymis near the left testicle, measuring 3.5 cm × 2.2 cm in diameter. However, he had no symptoms in the right testicle and epididymis with unremarkable signs on physical examination. Laboratory results were within normal ranges. On urinalysis, pyuria was observed, but urine culture showed no microorganisms. Additionally, AFB staining and PCR for TB bacillus of the urine were negative. We performed semen analysis to evaluate infertility, which revealed no sperm in the semen, implying the diagnosis of azoospermia.
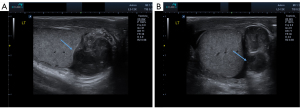
Scrotal ultrasonography demonstrated severe dilation of the left epididymis with heterogeneous echogenicity and an irregularly-shaped fluid-filled space in the area near the left epididymis, suggestive of severe epididymitis with abscess formation without abnormal appearance of the testicle (Figure 1). Meanwhile, the right testis and epididymis showed a normal appearance at the time (Figure 1). We examined testicular tumor markers such as alpha-fetoprotein, human chorionic gonadotropin, and lactate dehydrogenase in the blood, and the results were within normal limits.
Due to persistent testicular pain, intermittent fever, and severe epididymitis with abscess formation, the patient underwent surgery for scrotal exploration. The findings on the exploration revealed severely swollen and firm epididymis with abscess materials. Additionally, the vas deferens connected to the epididymis were severely hard and dilated, implying severe inflammatory reactions. Considering the worsening symptoms and the findings on surgical exploration, epididymectomy with partial resection of vas deferens was performed. At the same time, testicular biopsy was performed on both testicles to determine the cause of infertility.
The histopathological examination revealed chronic granulomatous inflammation with caseous necrosis rimmed with epithelioid macrophages, Langhans-type giant cells, and lymphocytes in the epididymis tissue after staining with hematoxylin-eosin (Figure 2). PCR test of resected epididymis tissue was positive for Mycobacterium tuberculosis, which confirmed the diagnosis of epididymal TB. Testicular biopsy performed during surgical management revealed that both testes had normal spermatogenesis. Initial urine AFB culture isolated TB bacillus several weeks after the surgical treatment.

According to histopathological results, the patient was treated with pyrazinamide for 3 months and isoniazid and rifampin for 6 months. After surgical intervention, the symptoms were relieved without any other discomfort. However, approximately 1 month after the surgery, he presented with pain in the right testicular area, although the pain was not as severe as the prior left testicular pain. Scrotal ultrasonography showed swollen and heterogeneous epididymis with an abscess appearance in the right epididymal area (Figure 3). Additionally, we performed a computed tomography (CT) scan to investigate other organ involvement, which showed a suspicious finding of TB lymphadenopathy in several lymph nodes. In addition, thickening of both vas deferens was observed, implying TB involvement and abscess formation in the right epididymal area (Figure 3). Considering the previous TB diagnosis of left epididymis, the patient was diagnosed with bilateral TB epididymis.

After several weeks of continued pharmacological treatment, the right testicular pain was relieved. After completion of the pharmacological treatment, the patient had no complaints, such as pain or swelling in both testicular areas. However, the finding of azoospermia was persistent on a subsequent semen analysis 1 month later. We described the timeline of clinical history in case presentation (Figure 4).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Genitourinary TB is a rare condition comprising about 4% of extra-pulmonary TB cases (15). Epididymal TB has a low incidence rate among extra-pulmonary manifestations, making the disease diagnosis challenging (3,10). Because the latent form of TB can evolve into active extra-pulmonary TB, including genitourinary TB when the immune system is suppressed due to old age, systemic diseases, and immunocompromised states such as human immunodeficiency virus infection and immunosuppressive agents after organ transplantation, a history of TB infection is an important factor in these situations (2,5,6). When a patient with testicular symptoms has a history of TB infection, physicians should consider the possibility of epididymal TB. However, epididymal TB may develop without any history of other organ involvement with TB infection (4,5). In our case, the patient did not report prior TB history.
Clinical symptoms of epididymal TB may not be definitive for diagnosing the disease without any other organ involvement. The common presenting symptoms include testicular pain, swelling, and a palpable nodule, which are similar to other diseases related to testis and epididymis, causing misdiagnosis. However, when the diagnosis is late or proper treatment is not applied, the disease may worsen, causing severe complications, including cutaneous fistulas, abscess formation, or extensive testis involvement. Additionally, sexual dysfunction or infertility can occur, particularly in young men (1,5,6). In our case, the clinical symptoms of the patient were testicular pain, swelling, and intermittent fever.
Subsequently, we found abscess formation on radiologic examination and infertility on semen analysis due to worsening disease status. He had been treated with antibiotics for several months with the suspicion of bacterial infection at medical facilities after the onset of the symptoms. The definitive diagnosis was epididymal TB; therefore, it is thought that the delayed diagnosis and improper treatment worsened the epididymal TB resulting in complications such as abscess formation and infertility. Therefore, patients with persistent or recurrent epididymitis should be followed up closely for the possibility of epididymal TB.
Interestingly, the patient in our case initially presented with left testicular pain and swelling, and right testicular symptoms occurred after several months, implying that epididymal TB might involve the other side of the organ over time. Although most cases of epididymal TB in the literature have been unilateral, bilateral involvement has also been reported (1). Therefore, these patients should be observed for presenting with symptoms and signs in the other testicle, particularly when prior history related to TB exists. Epididymal TB does not affect testicular function if it does not involve the testis extensively. In our case, testicular biopsy confirmed that the tissues of both testes were normal.
Several previous studies have reported that infertility might occur as a rare complication of genitourinary TB. Epididymis TB involvement can lead to male infertility through the obstruction and distortion of epididymis and vas deferens caused by granulomas and fibrosis, particularly when both epididymal areas are involved, as found in our patient (16,17). Tzvetkov et al. reported that 69 male patients with genital TB had infertility as a complication (18). Additionally, Fraietta et al. reported azoospermia caused by TB of seminal vesicles (19), and Gow et al. have described that genitourinary TB could develop calcification of the prostate, seminal vesicles and vas deferens (20). Venyo et al. described the possibility of the involvement of the penile shaft and the glans penis by TB, which could make sexual intercourse difficult due to structural deformity and lead to infertility subsequently (21). The same study also reported that semen deposition during intercourse might be suppressed by urethral strictures or urethrocutaneous fistulae, causing infertility (21). Patients with infertility due to genitourinary TB may be managed with in vitro fertilization. A study has reported that those patients had success rates comparable to men with azoospermia of other causes (22).
The definitive diagnosis of epididymal TB is made after identifying AFB from the epididymis tissue through Ziehl-Neelsen staining, cultures, or histopathological examination with microscopy (8,9). Although urine AFB culture is broadly used in diagnosing genitourinary TB, the method needs up to 8 weeks to acquire maximal sensitivity. On the other hand, urine AFB staining has low sensitivity, especially in genitourinary TB (10,11). Additionally, PCR has become another useful option for genitourinary TB diagnosis, with high sensitivity and specificity rates (11,12). However, in our case, urine PCR results were negative. It is thought that the concentration of AFB in urine is low, which makes the diagnosis based on staining, cultures, and PCR difficult in genitourinary TB. In our case, epididymal TB diagnosis was made by the histopathological examination of the resected epididymis tissue. The identification of AFB or chronic granulomatous inflammation with amorphous caseous necrosis on microscopy in the tissues acquired from the epididymis can make the definitive diagnosis of epididymal TB.
The treatment of choice for genitourinary TB is pharmacological treatment, which involves a combination of anti-TB drugs for 6 to 9 months, as in pulmonary TB or other extra-pulmonary TB forms (9,10,13). The standard regimen of anti-TB drugs was used in the treatment of TB in our case. Isoniazid, rifampin, and pyrazinamide, with or without ethambutol, are usually used initially for 6 to 12 weeks. After the initiation of pharmacological treatment, isoniazid and rifampin are used for an additional 3 to 6 months (10,13). The pharmacological treatment for genitourinary TB, including epididymal TB, should be initiated immediately after definitive diagnosis is made by histological or microbiological examination. Otherwise, when genitourinary TB is suspected clinically or radiologically, it is recommended that pharmacological treatment be started to prevent consequent complications, including abscess formation and male infertility, as in our case (1,5).
Surgery is the treatment option when pharmacological treatment fails because TB bacillus, embedded for many years or caused extensive epididymal or testicular involvement, may be resistant to pharmacological treatment (2,14). Surgery should also be performed when advanced disease has resulted in severe complications, including cutaneous fistulas, abscess formation, or extensive testicular involvement, presenting with persistent symptoms such as pain, swelling, and fever, as in our case (14). Surgical approach should also be considered when the diagnosis is not clearly made and one cannot rule out the possibility of epididymis or testicular neoplasia by radiologic findings (23). Moreover, surgical treatment might be considered more strongly when the patient has a history of pulmonary TB or immunosuppression. However, it might develop alone without any history of other organ involvement with TB, like our case; therefore, we should not exclude the possibility of the development of epididymal TB in patients without a history of TB infection (10). As surgical management for epididymal TB, epididymectomy is the procedure most commonly performed with or without respective orchiectomy, depending on the extent of the disease.
Conclusions
Epididymal TB is a rare disease that is difficult to diagnose due to similarities with other epididymo-testicular diseases and low sensitivity and specificity of diagnostic tools except for histopathological examination. However, physicians should consider the possibility of epididymal TB in patients with persistent testicular symptoms. When definitive diagnosis of epididymal TB is established or clinically suspected, immediate initiation of pharmacological treatment should be performed to prevent subsequent complications, including abscess formation, extensive disease, or male infertility. A surgical approach should be considered when pharmacological treatment fails, or severe complications develop.
In particular, epididymal TB should be suspected in young patients with persistent or recurrent epididymitis history and monitored subsequently for symptoms and signs in the other testicle to prevent male infertility.
Acknowledgments
The authors thank the entire staff of the Department of Urology, Sanggye Paik Hospital, Inje University College of Medicine.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-22-728/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-22-728/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committees and with the Declaration of Helsinki (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Madeb R, Marshall J, Nativ O, et al. Epididymal tuberculosis: case report and review of the literature. Urology 2005;65:798. [Crossref] [PubMed]
- Muneer A, Macrae B, Krishnamoorthy S, et al. Urogenital tuberculosis - epidemiology, pathogenesis and clinical features. Nat Rev Urol 2019;16:573-98. [Crossref] [PubMed]
- Kulchavenya E, Kholtobin D, Shevchenko S. Challenges in urogenital tuberculosis. World J Urol 2020;38:89-94. [Crossref] [PubMed]
- Lee IK, Yang WC, Liu JW. Scrotal tuberculosis in adult patients: a 10-year clinical experience. Am J Trop Med Hyg 2007;77:714-8. [Crossref] [PubMed]
- Huang Y, Chen B, Cao D, et al. Surgical management of tuberculous epididymo-orchitis: a retrospective study of 81 cases with long-term follow-up. BMC Infect Dis 2021;21:1068. [Crossref] [PubMed]
- Borges WM, Bechara GR, de Miranda MML, et al. Epididymis tuberculosis: Case report and brief review of the literature. Urol Case Rep 2019;26:100969. [Crossref] [PubMed]
- Chandran S, Rahman A, Norris JM, et al. Diagnostic pitfalls of urogenital tuberculosis. Trop Med Int Health 2021;26:753-9. [Crossref] [PubMed]
- K Mehta P. Kamra E. Recent trends in diagnosis of urogenital tuberculosis. Future Microbiol 2020;15:159-62. [Crossref] [PubMed]
- Buchholz NP, Salahuddin S, Haque R. Genitourinary tuberculosis: a profile of 55 in-patients. J Pak Med Assoc 2000;50:265-9. [PubMed]
- Jacob JT, Nguyen TM, Ray SM. Male genital tuberculosis. Lancet Infect Dis 2008;8:335-42. [Crossref] [PubMed]
- Moussa OM, Eraky I, El-Far MA, et al. Rapid diagnosis of genitourinary tuberculosis by polymerase chain reaction and non-radioactive DNA hybridization. J Urol 2000;164:584-8. [Crossref] [PubMed]
- Figueiredo AA, Lucon AM, Arvellos AN, et al. A better understanding of urogenital tuberculosis pathophysiology based on radiological findings. Eur J Radiol 2010;76:246-57. [Crossref] [PubMed]
- Wejse C. Medical treatment for urogenital tuberculosis (UGTB). GMS Infect Dis 2018;6:Doc04. [PubMed]
- Cek M, Lenk S, Naber KG, et al. EAU guidelines for the management of genitourinary tuberculosis. Eur Urol 2005;48:353-62. [Crossref] [PubMed]
- Singh JP, Priyadarshi V, Kundu AK, et al. Genito-urinary tuberculosis revisited--13 years' experience of a single centre. Indian J Tuberc 2013;60:15-22. [PubMed]
- Gueye SM, Ba M, Sylla C, et al. Epididymal manifestations of urogenital tuberculosis. Prog Urol 1998;8:240-3. [PubMed]
- Ravikanth R, Kamalasekar K, Patel N. Extensive Primary Male Genital Tuberculosis. J Hum Reprod Sci 2019;12:258-61. [Crossref] [PubMed]
- Tzvetkov D, Tzvetkova P. Tuberculosis of male genital system--myth or reality in 21st century. Arch Androl 2006;52:375-81. [Crossref] [PubMed]
- Fraietta R, Mori MM, De Oliveira JM, et al. Tuberculosis of seminal vesicles as a cause of aspermia. J Urol 2003;169:1472. [Crossref] [PubMed]
- Gow JG, Barbosa S. Genitourinary tuberculosis. A study of 1117 cases over a period of 34 years. Br J Urol 1984;56:449-55. [PubMed]
- Venyo AK. Tuberculosis of the Penis: A Review of the Literature. Scientifica (Cairo) 2015;2015:601624. [Crossref] [PubMed]
- Paick J, Kim SH, Kim SW. Ejaculatory duct obstruction in infertile men. BJU Int 2000;85:720-4. [Crossref] [PubMed]
- Kholtobin DP, Kulchavenya EV. Surgical treatment of patients with urogenital tuberculosis. Urologiia 2021;155-61. [Crossref] [PubMed]



