
This article has an erratum available at: http://dx.doi.org/10.21037/tau-2023-02 the article has been update on 2023-08-17 at here.
Effects of recipient education disparity on living donor kidney transplant outcomes across different ethnic groups: a retrospective study in the United States
Highlight box
Key findings
• Our study found that the educational background of living kidney transplant recipients can influence transplant outcomes. In addition, the unequal distribution of educational background across races may be a key factor influencing the prognosis of living kidney transplantation across races.
What is known and what is new?
• Different transplant outcomes among kidney transplant recipients with different educational backgrounds.
• Differences in transplant outcomes among living kidney transplant recipients with different educational backgrounds, and these differences are unevenly distributed across races.
What is the implication, and what should change now?
• Our study can help clinicians identify differences in the prognosis of living kidney transplant recipients from different educational backgrounds to identify disadvantaged groups and help this group of patients improve transplant outcomes through intensive medication adherence and behavioral guidance.
Introduction
Since the first successful living donor kidney transplant (LDKT), approximately 50,000 LDKTs have been performed annually in the US (1). Despite the significant improvements in LDKT over the past 50 years, the kidney transplant outcomes remain unsatisfactory. There are some reasons why a kidney transplant may fail, such as human leukocyte antigen (HLA) differences, immune reaction and graft failure. Among those, graft failure is the most common cause of transplant failure (2,3). Moreover, social factors such as socioeconomic status (SES) also have adverse effects on patient prognosis. Studies have shown that SES factors, such as education level, income level, employment status, citizenship status, and insurance coverage, are inherently interconnected with patient prognosis. Additional medical resources and social support can be obtained with a good SES. Studies have also indicated that kidney transplant recipients with higher SES might have graft survival and patient survival rates compared to those with lower SES (4,5). However, the effect of education level, as an essential factor in the evaluation of SES, on the prognosis of LDKT recipients remains unclear.
Previous studies have suggested that a higher educational background might improve the patient’s health literacy, leading to better medication adherence and, thereby, better transplant outcomes (6,7). However, the prognosis of Black patients tends to worsen after kidney transplantation (8,9), which might be due to multiple reasons, social factors including SES (9,10), transplant center effects, biological factors including non-compliance (11), HLA differences (12,13), and a more vigorous immune response (14). Similar to other SES factors, educational levels may also be unevenly distributed among different races.
Therefore, we hypothesize that education level might be critical in the prognostic differences among different ethnic groups. To test this hypothesis, the current study aimed to employ data from the United Network for Organ Sharing (UNOS) to investigate the correlation between confounding factors and the prognosis of LDKT recipients. A retrospective study was conducted to compare and validate the predictive differences in LDKT recipients with different education levels, and to assess the correlations between education level and the prognostic risk of LDKT recipients across different ethnic groups. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-288/rc).
Methods
Data source
The Organ Procurement and Transplantation Network (OPTN) data and study file released in March 2021 were used in this study. The data included patients who underwent LDKT between 2005 and 2020 (n=291,972), with follow-ups through December 31, 2021. Data collection was the sole responsibility of the authors; it does not necessarily reflect the views or policies of the US. Department of Health and Human Services, nor does it refer to trade names and commercial products or imply endorsements by the US government. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Study population
Using the transplant-related database collected by UNOS, we conducted a retrospective study of kidney transplant recipients, analyzing the records of all adults (≥18 years of age) who received a kidney transplant between January 1, 2005, and December 31, 2020. The exclusion criteria were as follows: (I) deceased donor kidney transplants; (II) recipients <18 years of age; (III) recipients of unknown and no education level; (IV) recipients of unknown race and races other than White, Black, Hispanic, or Asian; and (V) non-first kidney transplants, double kidney transplants, and multi-organ transplants.
Our primary goal was to determine the prognostic value of education level among LDKT recipients. LDKT recipients were divided into two education level groups: the lower-education group and the higher-education group. The lower-education group included grade school [0–8], high school [9–12], and General Educational Development (GED). The higher-education group consisted of those who attended college/technical school, associate/bachelor’s degree, or a post-college degree.
Measures and definition of outcomes
Primary outcomes of this study included graft survival (death-uncensored), patient survival, and death-censored graft survival (DCGS). Death censored graft failure (DCGF) was defined as time form transplantation until the date of returned to dialysis or re-transplantation (whichever occurred first). Patients who reached the study duration endpoint without experiencing death-censored graft failure or death were treated as censored observations. Patient survival was defined as the time from transplantation to the recipient’s death.
Statistical analyses
Person chi-square and student t-tests were used in testing associations for categorical and continuous recipient baseline characteristics with highest education level achieved, respectively. Comparative analyses of graft and patient survival were performed using Kaplan-Meier curves and log-rank test. Differences in the baseline characteristics across education levels were eliminated using propensity score matching. The baseline characteristics, which were potential confounders, were adjusted using Cox proportional hazards models to assess graft failure and patient mortality, which included the following covariates: recipient characteristics [education, age, race, body mass index (BMI), type of health insurance, cause of end-stage renal disease (ESRD), duration of dialysis, country of citizenship, employment income, calculated panel reactive antibody (CPRA), donor-recipient relationship, number of HLA mismatches], and donor characteristics (age, sex, and BMI). All covariates included in the Cox regression hazard model were tested for compliance with the proportional hazard assumption. We used Cox regression hazard model to test the prognostic risk differences among different races and levels of education, the adjusted variables include recipient’s age, sex, education, BMI, ABO compatible, primary insurance, cause of ESRD, dialysis time, citizenship, working for income, donor-recipient relationship, HLA-mismatch, CPRA, donor’s age, sex, BMI. All data were analyzed using R statistical software version 3.6.2 (RStudio is an open source form with more than one developer, belonging to Posit Software, PBC, and is an integrated development of the R language). All statistical tests were two-sided, and a P value <0.05 was considered to be statistically significant.
Results
Cohort statistics
After inclusion and exclusion, 76,150 adult LDKTs were performed between January 1, 2005, and December 31, 2020. Among them, the number of LDKTs performed on White people was the highest (n=50,476) and those performed on Asians were the lowest (n=3,943). The percentages of LDKTs who were White, Black and Asian were higher in the higher-education group than in the lower-education group; however, the lower-education group contained a higher percentage of Hispanic recipients compared to the higher-education group. Conversely, the lower-education group comprised 24.1% (950/3,943), 34.0% (17,172/50,476), 37.5% (3,937/10,490), and 59.2% (6,656/11,241) of Asians, Whites, Blacks, and Hispanics, respectively (P<0.001) (Figure 1). Among Asians, patients with a bachelor’s degree had the highest number of LDKTs. Meanwhile, among the other three ethnic groups, patients with high school-level education had the highest number of LDKTs. Among Hispanics, patients with postgraduate education levels had the least number of LDKTs, whereas patients with Grade school levels had the least number of LDKTs among the other three ethnic groups (Figure 2).


Baseline characteristics
Compared to the lower-education group, the higher-education group had an older average age (49.61±13.96 vs. 48.60±14.74 years), a higher proportion of middle-aged and older adults (74.5% vs. 72.3%), lower BMI (26.72±4.10 vs. 27.21±4.27), more White recipients (70.2% vs. 59.8%), more likely to have private health insurance (63.4% vs. 47.7%), more likely to have history of diabetes (72.3% vs. 67.6%), more likely to be a US citizen (96.7% vs. 91.8%), more likely to have an HLA mismatches ≥3 (75.1% vs. 71.9%), the proportion of acute rejection was lower (6.9% vs. 8.5%), the proportion of CPRA <30 was higher (23.8% vs. 21.0%), a shorter duration (in years) of dialysis before transplantation [1.16 (0.57, 2.23) vs. 1.42 (0.74, 2.65)], more likely to have a working income source (53.1% vs. 34.9%), less likely to be related to the donor (45.9% vs. 55.3%), received a kidney from an older living donor (43.69±12.09 vs. 41.20±11.81), lower donor BMI (27.76±5.41 vs. 28.03±5.48), median follow-up time was shorter [4.87 (2.00, 8.07) vs. 5.47 (2.54, 8.97)], total follow-up time was longer (257,209.03 vs. 170,578.1), the proportion of graft failure event was lower (18.5% vs. 25.1%), the proportion of DCGF event was lower (9.7% vs. 13.1%), the proportion of patient death event was lower (12.0% vs. 16.7%) (P<0.01 for all). The leading causes of ESRD in the higher-education and lower-education groups were glomerular disease (24.8%) and diabetes (26.7%), respectively (Table 1).
Table 1
| Variable | Higher-education group (N=47,435) | Lower-education group (N=28,715) | P value |
|---|---|---|---|
| Recipient age, mean (± SD) | 49.61 (±13.96) | 48.60 (±14.74) | <0.01 |
| Recipient age (years), n (%) | <0.01 | ||
| <40 | 12,116 (25.5) | 7,959 (27.7) | |
| 40–60 | 23,483 (49.5) | 13,878 (48.3) | |
| >60 | 11,836 (25.0) | 6,878 (24.0) | |
| Recipient sex, male, n (%) | 29,612 (62.4) | 18,133 (63.1) | 0.047 |
| Donor-recipient ABO match, yes, n (%) | 46,729 (98.5) | 28,334 (98.7) | 0.074 |
| Recipient BMI mean (± SD) | 27.76 (±5.41) | 28.03 (±5.48) | <0.01 |
| HLA mismatch ≥3, n (%) | 35,614 (75.1) | 20,647 (71.9) | <0.01 |
| CPRA | <0.01 | ||
| <30% | 38,895 (23.8) | 22,812 (21.0) | |
| ≥30% | 4,693 (75.1) | 2,812 (71.9) | |
| Unknown | 3,847 (1.1) | 3,091 (1.1) | |
| Recipient dialysis, (years, median, IQR) | 1.16 (0.57, 2.23) | 1.42 (0.74, 2.65) | <0.01 |
| Recipient ethnicity, n (%) | <0.01 | ||
| White | 33,304 (70.2) | 17,172 (59.8) | |
| Black | 6,553 (13.8) | 3,937 (13.7) | |
| Hispanic | 4,585 (9.7) | 6,656 (23.2) | |
| Asian | 2,993 (6.3) | 950 (3.3) | |
| Recipient primary payment, n (%) | <0.01 | ||
| Private insurance | 30,056 (63.4) | 13,702 (47.7) | |
| Non-private insurance | 17,379 (36.6) | 15,013 (52.3) | |
| History of diabetes, n (%) | 34,307 (72.3) | 19,411 (67.6) | <0.01 |
| Cause of ESRD, n (%) | <0.01 | ||
| DM | 10,615 (22.4) | 7,674 (26.7) | |
| Hypertension | 7,415 (15.6) | 6,159 (21.4) | |
| Glomerular disease | 11,754 (24.8) | 6,181 (21.5) | |
| Polycystic kidneys | 7,104 (15.0) | 2,817 (9.8) | |
| Other | 10,547 (22.2) | 5,884 (20.5) | |
| Acute rejection, n (%) | 3,289 (6.9) | 2,450 (8.5) | <0.01 |
| Recipient citizenship, n (%) | <0.01 | ||
| US citizens | 45,846 (96.7) | 26,366 (91.8) | |
| Resident alien | 471 (1.0) | 807 (2.8) | |
| Non-resident alien | 1,118 (2.4) | 1,542 (5.4) | |
| Working for income? Yes, n (%) | 25,188 (53.1) | 10,022 (34.9) | <0.01 |
| Donor-recipient relationship, n (%) | <0.01 | ||
| Related | 21,765 (45.9) | 15,885 (55.3) | |
| Unrelated | 25,670 (54.1) | 12,830 (44.7) | |
| Donor age, mean (± SD) | 43.69 (±12.09) | 41.20 (±11.81) | <0.01 |
| Donor sex, male, n (%) | 18,121 (38.2) | 10,607 (36.9) | <0.01 |
| Donor BMI, mean (± SD) | 26.72 (±4.10) | 27.21 (±4.27) | <0.01 |
| Median follow-up time (years, median, IQR) | 4.87 (2.00, 8.07) | 5.47 (2.54, 8.97) | <0.01 |
| Total follow-up time (years) | 257,209.03 | 170,578.14 | <0.01 |
| Graft failure, n (%) | 8,761 (18.5) | 7,216 (25.1) | <0.01 |
| DCGF, n (%) | 4,585 (9.7) | 3,750 (13.1) | <0.01 |
| Patient death, n (%) | 5,698 (12.0) | 4,804 (16.7) | <0.01 |
SD, standard deviation; BMI, body mass index; HLA, human leucocyte antigen; CPRA, calculated panel reactive antibody; IQR, interquartile range; ESRD, end-stage renal disease; DM, diabetes mellitus; ABO, donor-recipient ABO compatible; DCGF, death censored graft failure.
Graft survival, DCGS and patient survival
Overall, graft survival, DCGS and patient survival was higher in the higher-education group than in the lower-education group (P<0.001 for all) (Figure 3). Graft survival was higher in the higher-education group than in the lower-education group (P<0.01 for all) in other three ethnic groups, except among Hispanics (P=0.382) (Figure S1). DCGS was higher in the higher-education group than in the lower-education group (P<0.05 for all) across all three ethnic groups, except among Hispanics (P=0.265) (Figure S2). Patient survival was higher in the higher-education group than in the lower-education group (P<0.01 for all) across all three ethnic groups, except among Hispanics (P=0.408) (Figure S3). After propensity score matching, we still observed similar results that the total graft, DCGS and patient survival of the higher-education group was higher than those in the lower-education group (P<0.01 for all) (Figure 4). Graft survival, DCGS, and patient survival of the three ethnic groups (White, Black, Asian) in the higher-education group were higher than in the lower-education group (P<0.05 for all), expect for Hispanic (P=0.163, P=0.717, 0.164 respectively) (Figures S4-S6). After considering the interrelationship between education and race, we analyzed the prognostic results between different races. Asian graft survival, DCGS, and patient survival were significantly higher than the other three races in the high-education group (P<0.05 for all) (Figure S7). Asian graft survival and patient survival were significantly higher than the other two races (White and Black) in the lower-education group (P<0.01 for all), but it was no significant of graft survival, DCGS and patient survival between Asian and Hispanic (P=0.657, P=1, P=1, respectively) (Figure S8).


Five-, ten-, and fifteen-year survival analysis between the two education groups
Overall, the 5-, 10-, 15-year of graft, DCGS and patient survival rates were observed in the higher-education group better than in the lower-education group (P<0.01 for all) (Tables 2-4).
Table 2
| Race | Five-year (%) | Ten-year (%) | Fifteen-year (%) |
|---|---|---|---|
| Total | |||
| Higher-education group | 87.3 (87.0–87.7) | 68.2 (67.6–68.9) | 44.7 (43.2–46.4) |
| Lower-education group | 84.5 (84.0–85.0) | 62.6 (61.8–63.5) | 37.6 (35.9–39.4) |
| P value | <0.01 | <0.01 | <0.01 |
| White | |||
| Higher-education group | 87.7 (87.2–88.1) | 68.7 (67.9–69.5) | 45.4 (43.6–47.4) |
| Lower-education group | 84.0 (83.4–84.7) | 61.7 (59.9–63.6) | 35.7 (33.6–37.9) |
| P value | <0.01 | <0.01 | 0.19 |
| Black | |||
| Higher-education group | 83.1 (82.0–84.2) | 61.7 (59.9–63.6) | 35.7 (31.6–40.2) |
| Lower-education group | 78.1 (76.6–79.6) | 55.6 (53.5–59.9) | 31.7 (27.8–36.1) |
| P value | 0.38 | <0.01 | <0.01 |
| Hispanic | |||
| Higher-education group | 92.6 (91.4–93.8) | 77.8 (75.2–80.5) | 58.0 (50.8–66.2) |
| Lower-education group | 91.6 (89.5–93.7) | 70.2 (65.5–75.2) | 52.9 (45.6–61.4) |
| P value | <0.01 | 0.38 | <0.01 |
| Asian | |||
| Higher-education group | 87.9 (86.7–89.1) | 69.3 (67.0–71.8) | 48.4 (43.7–53.5) |
| Lower-education group | 88.9 (88.0–89.8) | 69.6 (67.8–71.4) | 47.7 (43.9–51.8) |
| P value | 0.49 | 0.017 | <0.01 |
The data in parentheses represent 95% confidence interval.
Table 3
| Race | Five-year (%) | Ten-year (%) | Fifteen-year (%) |
|---|---|---|---|
| Total | |||
| Higher-education group | 92.8 (92.5–93.1) | 82.4 (81.8–82.9) | 67.2 (65.6–68.8) |
| Lower-education group | 91.1 (90.7–91.4) | 78.6 (77.8–79.3) | 62.6 (60.6–64.6) |
| P value | <0.01 | <0.01 | <0.01 |
| White | |||
| Higher-education group | 93.7 (93.4–94.1) | 84.6 (84.0–85.2) | 70.8 (69.0–72.7) |
| Lower-education group | 91.9 (91.4–92.4) | 80.3 (79.4–81.2) | 64.8 (62.2–67.4) |
| P value | <0.01 | <0.01 | 0.5 |
| Black | |||
| Higher-education group | 87.5 (86.5–88.4) | 72.1 (70.4–73.8) | 51.2 (46.7–56.1) |
| Lower-education group | 84.1 (82.8–85.5) | 68.9 (66.9–71.0) | 50.6 (45.8–55.9) |
| P value | 0.38 | <0.01 | <0.01 |
| Hispanic | |||
| Higher-education group | 92.0 (91.0–93.0) | 78.4 (76.2–80.7) | 62.6 (57.7–68.0) |
| Lower-education group | 92.6 (91.8–93.3) | 79.8 (78.2–81.5) | 63.9 (59.9–68.1) |
| P value | 0.4 | 0.016 | <0.01 |
| Asian | |||
| Higher-education group | 95.6 (94.6–96.5) | 86.0 (83.7–88.3) | 70.6 (63.6–78.4) |
| Lower-education group | 95.0 (93.4–96.7) | 79.6 (75.3–84.1) | 68.7 (62.2–76.0) |
| P value | <0.01 | 0.027 | 0.013 |
The data in parentheses represent 95% confidence interval.
Table 4
| Race | Five-year (%) | Ten-year (%) | Fifteen-year (%) |
|---|---|---|---|
| Total | |||
| Higher-education group | 92.4 (92.1–92.7) | 77.7 (77.1–78.3) | 58.4 (56.8–60.2) |
| Lower-education group | 90.8 (90.4–91.2) | 73.5 (72.7–74.3) | 51.4 (49.6–53.2) |
| P value | <0.01 | <0.01 | <0.01 |
| White | |||
| Higher-education group | 91.8 (91.4–92.1) | 76.2 (75.5–77.0) | 56.7 (54.8–58.7) |
| Lower-education group | 89.5 (89.0–90.0) | 70.7 (69.7–71.7) | 47.3 (45.1–49.6) |
| P value | <0.01 | <0.01 | 0.66 |
| Black | |||
| Higher-education group | 92.8 (92.0–93.5) | 78.6 (77.0–80.2) | 56.7 (52.1–61.6) |
| Lower-education group | 90.4 (89.3–91.4) | 72.2 (70.1–74.4) | 50.5 (45.9–55.5) |
| P value | 0.29 | <0.01 | <0.01 |
| Hispanic | |||
| Higher-education group | 96.3 (95.4–97.1) | 86.8 (84.5–89.1) | 76.9 (70.9–83.3) |
| Lower-education group | 95.4 (93.8–97.0) | 81.9 (77.9–86.1) | 65.7 (57.7–74.8) |
| P value | <0.01 | 0.42 | <0.01 |
| Asian | |||
| Higher-education group | 94.1 (93.2–95.0) | 83.5 (81.6–85.5) | 68.9 (63.7–74.5) |
| Lower-education group | 94.2 (93.5–94.9) | 82.1 (80.6–83.7) | 65.3 (61.3–69.6) |
| P value | 0.55 | 0.032 | <0.01 |
The data in parentheses represent 95% confidence interval.
Among White, the 5- and 10-year of graft survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Black the 10- and 15-year of graft survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Hispanic the 5- and 15-year of graft survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Asian the 10- and 15-year of graft survival rate in the higher-education group better than in the lower-education group (P<0.05 for both) (Table 2).
Among White, the 5- and 10-year of DCGS rate in the higher-education group higher than in the lower-education group (P<0.01 for both). Among Black the 10- and 15-year of DCGS rate in the higher-education group higher than in the lower-education group (P<0.01 for both). Among Hispanic the 10- and 15-year of DCGS rate in the higher-education group higher than in the lower-education group (P<0.05 for both). Among Asian the 5-, 10- and 15-year of DCGS rate in the higher-education group higher than in the lower-education group (P<0.05 for all) (Table 3).
Among White, the 5- and 10-year of patient survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Black the 10- and 15-year of patient survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Hispanic the 5- and 15-year of patient survival rate in the higher-education group better than in the lower-education group (P<0.01 for both). Among Asian the 10- and 15-year of patient survival rate in the higher-education group better than in the lower-education group (P<0.05 for both) (Table 4).
Cox proportional hazards model
Compared to the higher-education group, the lower-education group had an 11% higher risk of graft failure [adjusted hazard ratio (aHR), 1.11; 95% confidence interval (CI): 1.06 to 1.16], a 15% higher risk of DCGF (aHR, 1.15; 95% CI: 1.08 to 1.22) and a 7% higher risk of mortality (aHR, 1.07; 95% CI: 1.02 to 1.14). Compared with the White group, the other ethnic groups showed the following risks of graft failure, DCGF and mortality rates: the Black recipients revealed an insignificant difference in graft failure risk ratio (aHR, 1.05; 95% CI: 0.99 to 1.11), a 46% higher risk of DCGF (aHR, 1.46; 95% CI: 1.35 to 1.57) a 22% lower risk of mortality (aHR, 0.78; 95% CI: 0.72 to 0.84); the Hispanic recipients had a 25% lower risk of graft failure (aHR, 0.75; 95% CI: 0.70 to 0.80), a 10% lower risk of DCGF (aHR, 0.90; 95% CI: 0.82 to 0.98) and a 35% lower risk of patient mortality (aHR, 0.65; 95% CI: 0.59 to 0.71); and the Asian recipients had a 36% lower risk of graft failure (aHR, 0.64; 95% CI: 0.57 to 0.72), a 23% lower risk of graft failure (aHR, 0.77; 95% CI: 0.66 to 0.90) and a 44% lower risk of patient mortality (aHR, 0.56; 95% CI: 0.48 to 0.65) (Figures 5-7).
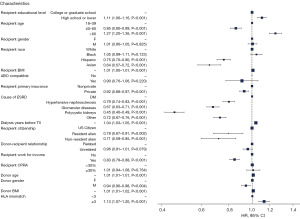


Subgroup analysis
The risks of graft failure and patient mortality in each ethnic group were compared between the lower- and higher-education groups. Among the White ethnic group, there was a 31% unadjusted increased risk of graft failure (HR, 1.31; 95% CI: 1.25 to 1.37), a 32% unadjusted increased risk of mortality (HR, 1.32; 95% CI: 1.25 to 1.39), and a 7% adjusted decreased risk of mortality (aHR, 0.93; 95% CI: 0.87 to 0.99) in the lower-education group compared to the higher-education group. Among the Black ethnic group, the unadjusted risks of graft failure and mortality increased by 27% (HR, 1.27; 95% CI: 1.16 to 1.38) and 35% (HR, 1.35; 95% CI: 1.20 to 1.51), and the adjusted risks of graft failure increased by 18% (aHR, 1.18; 95% CI: 1.07 to 1.30) in the lower-education group as compared to the higher-education group. Among the Asian ethnic group, there was a 26% unadjusted increased risk of graft failure (HR, 1.26; 95% CI: 1.02 to 1.56) and a 43% unadjusted increased risk of mortality (HR, 1.43; 95% CI: 1.08 to 1.90) in the lower-education group compared to the higher-education group. Among the Hispanic ethnic groups, the risk ratios for graft failure and mortality rates before and after adjustment were not statistically significant in the lower-education group compared to the higher-education group (Table 5).
Table 5
| Outcome | White | Black | Hispanic | Asian |
|---|---|---|---|---|
| Graft failure, HR (95% CI) | ||||
| Higher-education | Reference | |||
| Lower-education | 1.31 (1.25 to 1.37) | 1.27 (1.16 to 1.38) | 0.95 (0.86 to 1.06) | 1.26 (1.02 to 1.56) |
| Patient mortality, HR (95% CI) | ||||
| Higher-education | Reference | |||
| Lower-education | 1.32 (1.25 to 1.39) | 1.35 (1.20 to 1.51) | 1.04 (0.90 to 1.20) | 1.43 (1.08 to 1.90) |
| After adjusted covariates, aHR (95% CI) | ||||
| Graft failure | ||||
| Higher-education | Reference | |||
| Lower-education | 1.01 (0.96 to 1.07) | 1.18 (1.07 to 1.30) | 0.92 (0.81 to 1.04) | 1.23 (0.94 to 1.61) |
| Patient mortality | ||||
| Higher-education | Reference | |||
| Lower-education | 0.93 (0.87 to 0.99) | 0. 89 (0.77 to 1.02) | 0.98 (0.83 to 1.17) | 0.79 (0.55 to 1.14) |
The model was adjusted for the following covariates: recipient’s education, age, sex, BMI, ABO compatible, primary insurance, cause of ESRD, dialysis time, citizenship, working for income, donor-recipient relationship, HLA-mismatch, CPRA, as well as the donor’s age, sex, BMI. HR, hazard ratio; aHR, adjusted hazard ratio; CI, confidence internal; BMI, body mass index; ABO, donor-recipient ABO compatible; ESRD, end-stage renal disease; HLA, human leucocyte antigen; CPRA, calculated panel reactive antibody.
Discussion
In this study, the data of 76,150 LDKT recipients obtained from the UNOS database between 2005 and 2020 were analyzed. The results demonstrated that the high-education group had better graft and patient survival rates than the low-education group across different ethnic groups. The risk of graft failure increased with lower education in the Black ethnic group. The risk of patient mortality decreased with lower education in the White ethnic group. However, there was no significant difference in the risk of graft failure and patient mortality between the two education level groups in the Hispanic and Asian ethnic groups. Furthermore, this study also confirmed the adverse effects of low educational levels on the prognosis of LDKT recipients.
This research also indicated that educational level was closely related to the prognosis of recipients, which might be inseparable from the post-transplant nursing care of patients. We observed a similar phenomenon in other diseases, where highly educated patients with gastric cancer and those who underwent knee surgery had better outcomes than those with low levels of education (15,16). A better educational background can help patients understand basic health information related to their disease, resulting in better adherence to immunosuppressive drugs after kidney transplantation. In the study by Ghods et al. It was suggested that one possible mechanism by which lower levels of education may lead to poorer transplant outcomes may be lower adherence to immunosuppressive regimens (17). In addition, educational background may also influence patients’ proper use of therapeutic drugs, with studies finding that compliance with oral anticoagulants was 21% higher in the most educated patients with atrial fibrillation than in the least educated (18). Consistent with the current results, a previous study suggested that higher education levels might lead to higher incomes (19), which might translate into better healthcare services and regular long-term use of immunosuppressants. In addition, the social support received by recipients with high educational levels was relatively high. For example, they might seek healthcare service support through online advertising or social media, while recipients with low education levels might have poor social support and poor access to healthcare. In several studies, we observed a similar trend, with significantly better transplant outcomes for higher-education recipients than for lower-education recipients in the overall population receiving kidney transplants (6,19,20).
Previous studies have confirmed that social factors, such as low education levels, poverty, and unemployment, could affect medical outcomes, thereby adversely affecting human health (19,21). However, unlike most social factors, the effects of a low education level on the prognosis of LDKT recipients might change to a certain extent. One study indicated that improving nephrologists’ awareness of patients’ transplantation and education before and after transplantation could improve the impact of low education levels to a certain extent (22). In addition, the current study showed that diabetes is an independent risk factor for poor prognosis in LDKT recipients. A previous study confirmed that individuals with low educational levels were more likely to develop diabetes due to poor health behaviors, work, and life stress (23). Moreover, a 2017 annual kidney transplantation report showed that diabetes could affect the prognosis of recipients. Among the main pathogenic factors, ESRD caused by diabetes has the worst prognosis (24). Diabetes is a significant factor affecting the risk of death among LDKT recipients in the US; among them, type 1 diabetes has the highest mortality rate (25).
The annual family income of the lower-education group also has a significant impact on the management and treatment of diabetes. In general, education level is positively correlated with the patient’s annual family income. However, with the increase in medical costs, diabetic patients are required to control disease progression through lifelong medication, which also imposes a considerable economic burden on patients with low educational levels. In 2007, the average annual medical expenditure of diabetic patients in the US was $11,744, which was 2.3 times higher than that of non-diabetic patients (26). This might also be another important reason for the poor prognosis of patients with low educational levels.
Regular long-term use of immunosuppressants after transplantation is critical for graft survival. However, the income sources and insurance coverage of recipients with lower-education group are unlikely to support the regular use of immunosuppressants. In this study, recipients with low education levels were less likely to have private insurance and a stable source of work income than those with high education levels, which might also contribute to the poor outcomes of recipients with low education levels. Public health insurance has a precise time limit for post-transplant immunosuppressants and requires patients to bear part of the drugs’ costs (27), leading to a pessimistic attitude towards high medical costs among low-educated recipients and ultimately resulting in a poor prognosis. Compared to public health insurance, private insurance companies bear a high proportion of medical expenses, thereby significantly reducing the patient’s expenses, which reduces the patient’s financial pressure after surgery, resulting in better compliance with immunosuppressants, and helping patients achieve better transplant outcomes. A previous study reported similar outcomes among patients who underwent liver transplants; the study revealed that patients with other types of medical insurance had lower survival rates than those with private medical insurance (28).
Existing studies suggest that Black recipients often have poor prognoses after transplantation (8,29-31). However, in our study, it was found that Black recipients had a worse prognosis risk for DCGF compared to White recipients, with no significant difference in graft failure and patient mortality. This may be related to the improvement of transplantation strategies in recent years and the emphasis on postoperative care. Extant literature demonstrates that the gradual improvement of education level could narrow down the difference in prognosis between Black and White recipients (6). This also suggests that relevant measures could be taken to alleviate the difference in education level, thereby reducing the difference in transplant outcomes among different ethnicities. In addition, the current study also showed no significant differences in transplant outcomes among Hispanics before and after matching the baseline characteristics between the different education groups.
The current study also compared the prognostic risk among different education groups across the four ethnic groups. The results showed no significant differences in the prognostic risk of graft failure and mortality rate among Hispanic recipients between the two education groups with or without adjustment for relevant covariates. But in the other three races, we can find differences in prognostic risk before or after adjusted. After adjusting for confounders, White recipients with higher education levels had a higher risk of mortality, while Black recipients with lower education levels had a higher risk of graft failure, reflecting the impact of education on the predictive risk of recipients. The effects of education levels were illustrated in the White and Black ethnic groups. After adjusting for confounding factors, the risk of mortality among White recipients in different education levels was reversed, which may be due to the fact that the baseline characteristics in the lower-education group is not conducive to the long-term survival of white recipients in the lower-education group. After adjusting for confounding factors, the risk of graft failure in Black patients remains higher in the low-education group. However, including insufficient variables for adjustment and a lack of fully adjusting the effects of other variables on patient prognosis might have caused this change. Therefore, the effects of high education level on the risk of graft failure in White recipients might not have been truly reflected.
This research has certain limitations that should be noted. First, this study analyzed and compared the results of LDKT for a cohort between 2000 and 2020 for different educational level groups. However, during this period, there were significant innovations in healthcare services after LDKT, such as immunotherapy and postoperative care, as well as changes in donor and recipient selection. These potential confounding factors should be analyzed and explained. Second, this was a retrospective study that lacked control over all potential confounding factors. Although the variables collected in the UNOS database were sufficiently rich, they did not fully cover all of the baseline characteristics of patients; therefore, some crucial variables might have been missed. Finally, data quality is often a critical issue when analyzing large databases such as UNOS because of missing or incorrect information in the data. Such issues are difficult to address in retrospective studies but are vital for large databases, which is one of the disadvantages of retrospective analysis.
Conclusions
In conclusion, a higher educational level could positively affect the prognosis of LDKT recipients and dramatically improve their outcomes. However, the degree to which educational level affects prognosis is inconsistent across races. Our findings may benefit nephrologists by helping patients achieve long-term recovery after transplantation.
Acknowledgments
We gratefully acknowledge the research support from the OPTN/UNOS and the data analysis guided by Dr. Nahel Elias at the Center for Transplantation Sciences and Division of Transplant Surgery, Department of Surgery, Massachusetts General Hospital, Boston, Massachusetts, USA.
Funding: This work was supported by grants from Beijing NOVA program (No. 20220484230).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-288/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-288/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-288/coif). QY serves as an unpaid editorial board member (Emerging Editor) of Health Care Science from 2022 to 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lentine KL, Lam NN, Segev DL. Risks of Living Kidney Donation: Current State of Knowledge on Outcomes Important to Donors. Clin J Am Soc Nephrol 2019;14:597-608. [Crossref] [PubMed]
- Gill JS, Rose C, Pereira BJ, et al. The importance of transitions between dialysis and transplantation in the care of end-stage renal disease patients. Kidney Int 2007;71:442-7. [Crossref] [PubMed]
- Cosio FG, Hickson LJ, Griffin MD, et al. Patient survival and cardiovascular risk after kidney transplantation: the challenge of diabetes. Am J Transplant 2008;8:593-9. [Crossref] [PubMed]
- Naylor KL, Knoll GA, Shariff SZ, et al. Socioeconomic Status and Kidney Transplant Outcomes in a Universal Healthcare System: A Population-based Cohort Study. Transplantation 2019;103:1024-35. [Crossref] [PubMed]
- Francis A, Didsbury M, Lim WH, et al. The impact of socioeconomic status and geographic remoteness on access to pre-emptive kidney transplantation and transplant outcomes among children. Pediatr Nephrol 2016;31:1011-9. [Crossref] [PubMed]
- Goldfarb-Rumyantzev AS, Sandhu GS, Barenbaum A, et al. Education is associated with reduction in racial disparities in kidney transplant outcome. Clin Transplant 2012;26:891-9. [Crossref] [PubMed]
- Hod T, Goldfarb-Rumyantzev AS. The role of disparities and socioeconomic factors in access to kidney transplantation and its outcome. Ren Fail 2014;36:1193-9. [Crossref] [PubMed]
- Gordon EJ, Ladner DP, Caicedo JC, et al. Disparities in kidney transplant outcomes: a review. Semin Nephrol 2010;30:81-9. [Crossref] [PubMed]
- Malek SK, Keys BJ, Kumar S, et al. Racial and ethnic disparities in kidney transplantation. Transpl Int 2011;24:419-24. [Crossref] [PubMed]
- Ciancio G, Burke GW, Suzart K, et al. The use of daclizumab, tacrolimus and mycophenolate mofetil in african-american and Hispanic first renal transplant recipients. Am J Transplant 2003;3:1010-6. [Crossref] [PubMed]
- Butkus DE, Meydrech EF, Raju SS. Racial differences in the survival of cadaveric renal allografts. Overriding effects of HLA matching and socioeconomic factors. N Engl J Med 1992;327:840-5. [Crossref] [PubMed]
- Eckhoff DE, Young CJ, Gaston RS, et al. Racial disparities in renal allograft survival: a public health issue? J Am Coll Surg 2007;204:894-902; discussion 902-3. [Crossref] [PubMed]
- Roberts JP, Wolfe RA, Bragg-Gresham JL, et al. Effect of changing the priority for HLA matching on the rates and outcomes of kidney transplantation in minority groups. N Engl J Med 2004;350:545-51. [Crossref] [PubMed]
- Hutchings A, Purcell WM, Benfield MR. Increased costimulatory responses in African-American kidney allograft recipients. Transplantation 2001;71:692-5. [Crossref] [PubMed]
- Goodman SM, Mandl LA, Mehta B, et al. Does Education Level Mitigate the Effect of Poverty on Total Knee Arthroplasty Outcomes? Arthritis Care Res (Hoboken) 2018;70:884-91. [Crossref] [PubMed]
- Xu J, Du S, Dong X. Associations of Education Level With Survival Outcomes and Treatment Receipt in Patients With Gastric Adenocarcinoma. Front Public Health 2022;10:868416. [Crossref] [PubMed]
- Ghods AJ, Nasrollahzadeh D. Noncompliance with immunnosuppressive medications after renal transplantation. Exp Clin Transplant 2003;1:39-47. [PubMed]
- Teppo K, Jaakkola J, Biancari F, et al. Association of income and educational levels with adherence to direct oral anticoagulant therapy in patients with incident atrial fibrillation: A Finnish nationwide cohort study. Pharmacol Res Perspect 2022;10:e00961. [Crossref] [PubMed]
- Goldfarb-Rumyantzev AS, Koford JK, Baird BC, et al. Role of socioeconomic status in kidney transplant outcome. Clin J Am Soc Nephrol 2006;1:313-22. [Crossref] [PubMed]
- Schold JD, Buccini LD, Kattan MW, et al. The association of community health indicators with outcomes for kidney transplant recipients in the United States. Arch Surg 2012;147:520-6. [Crossref] [PubMed]
- Diaz VA Jr. Cultural factors in preventive care: Latinos. Prim Care 2002;29:503-17. viii. [Crossref] [PubMed]
- Goldfarb-Rumyantzev AS, Sandhu GS, Baird B, et al. Effect of education on racial disparities in access to kidney transplantation. Clin Transplant 2012;26:74-81. [Crossref] [PubMed]
- Allen K, McFarland M. How Are Income and Education Related to the Prevention and Management of Diabetes? J Aging Health 2020;32:1063-74. [Crossref] [PubMed]
- Hart A, Smith JM, Skeans MA, et al. OPTN/SRTR 2017 Annual Data Report: Kidney. Am J Transplant 2019;19:19-123. [Crossref] [PubMed]
- Harding JL, Pavkov M, Wang Z, et al. Long-term mortality among kidney transplant recipients with and without diabetes: a nationwide cohort study in the USA. BMJ Open Diabetes Res Care 2021;9:e001962. [Crossref] [PubMed]
- Economic costs of diabetes in the U.S. In 2007. Diabetes Care 2008;31:596-615. [Crossref] [PubMed]
- Woodward RS, Schnitzler MA, Lowell JA, et al. Effect of extended coverage of immunosuppressive medications by medicare on the survival of cadaveric renal transplants. Am J Transplant 2001;1:69-73. [Crossref] [PubMed]
- Yoo HY, Thuluvath PJ. Outcome of liver transplantation in adult recipients: influence of neighborhood income, education, and insurance. Liver Transpl 2004;10:235-43. [Crossref] [PubMed]
- Taber DJ, Egede LE, Baliga PK. Outcome disparities between African Americans and Caucasians in contemporary kidney transplant recipients. Am J Surg 2017;213:666-72. [Crossref] [PubMed]
- Lentine KL, Smith JM, Hart A, et al. OPTN/SRTR 2020 Annual Data Report: Kidney. Am J Transplant 2022;22:21-136. [Crossref] [PubMed]
- Taber DJ, Gebregziabher M, Hunt KJ, et al. Twenty years of evolving trends in racial disparities for adult kidney transplant recipients. Kidney Int 2016;90:878-87. [Crossref] [PubMed]
(English Language Editor: A. Kassem)


