
The therapeutic effect of pelvic floor muscle training on stress urinary incontinence following prostatectomy: a systematic review and meta-analysis
Highlight box
Key findings
• This study systematically evaluated the therapeutic effect of pelvic floor muscle training (PFMT) on stress Urinary incontinence after prostatectomy.
What is known and what is new?
• PFMT is one of the treatment methods for male Urinary incontinence after radical prostatectomy.
• However, there are still some disputes about whether PFMT can improve Urinary incontinence, so more high-level systematic evaluation is still needed to provide Evidence-based medicine evidence for the application and standardization of PFMT.
What are the implications, and what should change now?
• PFMT can significantly improve stress Urinary incontinence after prostatectomy. In the future, more high-quality research needs to be included for further exploration.
IntroductionOther Section
Prostate cancer is one of the most common cancers among males worldwide, with its incidence positively correlated with age. In males aged 65 and above, the incidence rate of prostate cancer is close to 60% (1). Radical prostatectomy (RP), is the gold standard for localized prostate cancer treatment and is associated with a 5-year survival rate greater than 95% (2,3). Despite excellent disease-specific survival, RP often causes debilitating consequences to continence and erectile function. Urinary incontinence is common after RP, occurring in 2% to 87% of patients (4,5). While continence improves in most men over time, this recovery time is variable with some patients requiring up to 12 months (6,7). In addition, a large proportion of men fail to achieve complete continence at any point and suffer from long-term leakage and impact on quality of life.
Pelvic floor muscle training (PFMT) is a well-described treatment for urinary incontinence after RP (8,9). Accordingly, it is recommended by the European Association of Urology (EAU) and the American Urology Association (AUA) as a first-line treatment for Urinary incontinence after prostatectomy (8,9).
Despite significant reported studies demonstrating that PFMT can improve post-operative urinary incontinence, there remains controversy as to its efficacy given conflicting results reported in other studies (10-13). For example, a 2004 study did not recommend it as a first-line rehabilitation after prostatectomy, as incontinence symptoms did not significantly improve over time (14). Systematic review is limited and also complicated by the wide variety of PFMT regimens that are reported across the literature. Thus, further systematic evaluations are needed to provide evidence-based medical evidence for the application and standardization of PFMT. We present this article in accordance with the PRISMA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-337/rc).
MethodsOther Section
Literature retrieval
Two trained researchers conducted a literature search following the established inclusion and exclusion criteria. The databases searched included PubMed, Web of Science, EMBASE, CNKI, VIP, Wanfang, and the China Biology and Medicine Literature Database (CBM). The search focused on literature regarding PFMT in patients after prostatectomy. The English search terms included pelvic floor muscle, prostatectomy, urinary incontinence, RP, physiotherapy, and prostatic tumor. The search was conducted from database establishment to January 30th, 2023, and included both Chinese and English language literature. The protocol of this systematic review has been registered in the International prospective register of systematic reviews (PROSPERO, No. CRD42023442960).
Inclusion and exclusion criteria of literature
Inclusion criteria
- Study type: randomized controlled trials, no limitation on blinding;
- Study population: prostate cancer patients aged ≥18 years old undergoing prostatectomy;
- Intervention: PFMT in the experimental group. The control group patients received routine exercise as a placebo;
- Outcome measures: patient-reported incontinence (1-hour urine pad test or 24-hour urine pad test was used to determine whether there was Urinary incontinence, that is, the incidence of self-control urination) and International Consultation on Incontinence Questionnaire-Simple Form (ICIQ-SF) score at 1-, 3-, 6-, and 12-month post-surgery, which was evaluated from both follow-up data and patients based on validated questionnaires.
Exclusion criteria
- Studies that are not randomized controlled trials;
- Conference papers, reports, reviews, meta-analyses, and other types of literature;
- Studies that included within the review examine PFMT in combination with other interventions and might not be considered eligible;
- Studies where the full text is unavailable or where important data are missing.
Literature screening and data extraction
Two researchers independently performed literature screening and data extraction based on the inclusion and exclusion criteria and then cross-checked their data. In case of any disagreements, a third researcher made the final decision. The extracted data included general information (author, publication year, sample size, patient age, follow-up time, etc.) and outcome indicators.
Risk of bias assessment
The quality assessment of the literature was conducted using the Cochrane collaboration’s tool for assessing the risk of bias in randomized trials (RoB1) (15), as recommended by the Cochrane Handbook, which included seven items: random allocation, group blindness, participant and researcher blindness, result measurement blindness, data completeness, selective reporting, and other biases. The items were evaluated as “unclear”, “no”, or “yes”.
Statistical analysis
A meta-analysis was performed using R 4.2.2. For binary data, the combined effect size was analyzed using odds ratio (OR) and 95% confidence interval (CI). For continuous variables, the combined effect size was analyzed using the mean difference (MD) and 95% CI. If P≥0.1 and I2≤50%, there was homogeneity among the included literature, and fixed-effect model analysis was performed. If P<0.1 and I2>50%, heterogeneity existed among the included studies. A random-effects model was employed for the analysis, and if necessary, the data were grouped into subgroups. A funnel plot was used to assess publication bias of the included literature. Differences were considered statistically significant at P<0.05.
ResultsOther Section
Literature search results
After the literature search, a total of 1,586 articles were obtained. After removing duplicate articles, a total of 1,464 articles were obtained. After reading the titles and abstracts, 1,266 articles that clearly did not meet the requirements were excluded, leaving 198 articles. Among these, the full text of 188 articles was accessible. A total of 113 articles were removed after secondary screening. After excluding 3 articles with duplicate content, 8 articles with significant missing data, and 53 articles that combined other interventions, a total of 11 articles were finally included. All of them were randomized controlled studies. as shown in Figure 1. The general information of the articles is shown in Table 1.
Table 1
| Author | Year of publication | Country | Study type | Age, years | Sample size | Operation | Follow-up period, months | Outcome indicators | |||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Experimental Group | Control Group | Experimental Group | Control Group | ||||||||
| Van Kampen (16) | 2000 | Germany | RCT | 64.38 | 66.58 | 50 | 52 | Prostatectomy | 12 | 1, 2, 3, 4 | |
| Filocamo (12) | 2005 | Italy | RCT | 65±4.79 | 68±5.33 | 150 | 150 | Prostatectomy | 12 | 1, 2, 3, 4 | |
| Manassero (9) | 2007 | Italy | RCT | 66.8±6.3 | 67.9±5.5 | 54 | 40 | Prostatectomy | 12 | 1, 2, 3, 4 | |
| Glazener (17) | 2011 | UK | RCT | – | – | 205 | 206 | Prostatectomy | 12 | 1, 2, 3, 4 | |
| Aydın Sayılan (10) | 2018 | Turkey | RCT | 63.00±8.61 | 59.93±6.98 | 30 | 30 | Prostatectomy | 6 | 1, 2, 3, 5 | |
| de Lira (11) | 2019 | Brazil | RCT | 67.3±5.63 | 63.53±7.62 | 16 | 15 | Prostatectomy | 3 | 3, 5 | |
| Milios (18) | 2019 | Australia | RCT | 62.2±6.8 | 63.5±6.8 | 50 | 47 | Prostatectomy | 4 | 1, 2 | |
| Oh (19) | 2020 | South Korea | RCT | 67.5±6.9 | 65.9±6.8 | 40 | 42 | Robot-assisted prostatectomy | 3 | 1, 2 | |
| Gezginci (13) | 2023 | Turkey | RCT | 67.6± 6.7 | 69.2± 5.4 | 30 | 30 | Prostatectomy | 3 | 5 | |
| Jian (20) | 2020 | China | RCT | 62.21±4.2 | 62.48±4.5 | 40 | 40 | Prostatectomy | 3 | 1, 2, 5 | |
| Zhong (21) | 2022 | China | RCT | 54–83 | 51–82 | 41 | 41 | Prostatectomy | 3 | 1, 2, 5 | |
Outcome indicators: 1 indicates patient-reported incontinence 1-month post-surgery; 2 indicates patient-reported incontinence 3-month post-surgery; 3 indicates patient-reported incontinence 6-month post-surgery; 4 indicates patient-reported incontinence 12-month post-surgery; 5 indicates ICIQ-SF (International Consultation on Incontinence Questionnaire-Simple Form), a simple form of the questionnaire for international consultation on incontinence. RCT, random clinical trial.
Risk of bias assessment of included literature
The risk of bias assessment results of 11 studies showed that 3 studies had a moderate risk of bias, and 8 studies had a low risk of bias (see Figures 2,3).
Meta results
Patient-reported incontinence
One month after the operation
The results of nine studies reporting the patient-reported incontinence one month after surgery were analyzed. Homogeneity existed among the studies (P=0.54, I2=0%), and the fixed effect model was employed. The meta-analysis showed that compared to the control group, patients undergoing PFMT had a significantly improved patient-reported incontinence one month after surgery (OR: 2.71, 95% CI: 1.86–3.94, P<0.01). This was visualized in Figure 4. A funnel plot was used to assess publication bias, and it was observed that all studies were within the funnel and showed symmetry, as shown in Figure 5. Egger’s test also supports that the risk of publication bias of included studies is low (P>0.05).

Three months after the operation
Nine studies reported the patient-reported incontinence three months after the surgery. There was heterogeneity among the studies (P<0.01, I2=68%), and a random-effects model was used. The meta-analysis results showed that compared with the control group, patients who underwent PFMT had an improved patient-reported incontinence three months after the surgery (OR: 3.42, 95% CI: 1.96–5.98, P<0.01). See Figure 6. Publication bias was shown using a funnel plot, and although there were three studies outside the funnel, they still showed symmetry, as shown in Figure 7. Egger’s test also supports that the risk of publication bias of included studies is low (P>0.05).

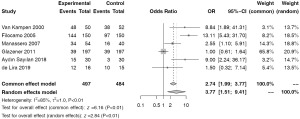
Six months after the operation
Six studies reported the patient-reported incontinence 6 months after surgery. There was heterogeneity among the studies (P<0.01, I2=85%), and a random-effects model was used. The meta-results showed that compared to the control group, patients who underwent PFMT had a 2.77-fold increase in urinary patient-reported incontinence 6 months after surgery (OR: 3.77, 95% CI: 1.51–9.41, P<0.01), as shown in Figure 8. Publication bias was displayed through a funnel plot, and two studies were outside the funnel and had poor symmetry, as shown in Figure 9. Egger’s test also supports that the risk of publication bias of included studies is low (P>0.05).
Twelve months after the operation
Four studies reported on the patient-reported incontinence 12 months after surgery. The studies were homogeneous (P=0.12, I2=49%) using a fixed effect model. The meta-analysis results showed that compared to the control group, patients who underwent PFMT had an increased patient-reported incontinence 12 months after surgery (OR: 1.21, 95% CI: 1.11–1.31, P<0.01), as shown in Figure 10. The funnel plot shows a low risk of publication bias, as all included studies were within the funnel and had good symmetry, as shown in Figure 11. Egger’s test also supports that the risk of publication bias of included studies is low (P>0.05).

ICIQ-SF score
The results of 4 studies reporting postoperative ICIQ-SF scores showed heterogeneity (P<0.01, I2=96%), and a random effects model was used. The meta-analysis results showed that compared to the control group, patients undergoing PFMT had a reduction in their postoperative ICIQ-SF scores (MD: −2.74, 95% CI: −4.96 to −0.52, P=0.02), as shown in Figure 12. Subgroup analysis by postoperative evaluation time found that the ICIQ-SF scores decreased after 1 month (MD: −0.61, 95% CI: −0.81 to −0.40) and after 3 months (MD: −3.43, 95% CI: −6.85 to −0.02), as shown in Figure 12.

Sensitivity analysis
The sensitivity analysis using the one-by-one elimination method showed that the elimination of literature one by one has little effect on the results, so it is robust.
DiscussionOther Section
Continuous urinary incontinence after prostatectomy is a common postoperative complication, with multiple studies suggesting that invasive treatment for urinary incontinence should be delayed for at least one year (17,22). As such, in certain cases, PFMT will be chosen as an alternative option. Some authors still argue that postprostatectomy urinary incontinence is due to an intrinsic deficiency of the pelvic floor muscles caused by excessive activity of the detrusor muscle and pelvic floor muscle damage (23). Excessive activity of the detrusor muscle is a pathological-physiological cause of urinary incontinence that can be corrected by PFMT. Wang et al. found that pelvic floor muscle contractions effectively inhibit detrusor muscle hypertrophy, increasing mechanical pressure on the urethra and preventing urinary incontinence (24). However, this does not seem to be widely supported, and the effectiveness of PFMT in treating post-RP urinary incontinence remains a controversial issue. Thus, the present meta-analysis aims to assess the effect of pelvic floor muscles on the patient-reported incontinence after RP.
The results of this study suggest that PFMT programs impact the recovery of patient-reported incontinence in men after RP. The meta-analysis showed that compared to the control group, the patient-reported incontinence after PFMT programs improved (1-month post-surgery OR: 2.7, 3-month post-surgery OR: 3.42, 6-month post-surgery OR: 3.77, 1-year post-surgery OR: 1.21). Our findings differ from those of Chang et al., who concluded that PFMT had low ORs at 1-, 3-, and 6-month post-surgery, with only a significant difference at 3 months (25). The study by Rangganata et al. found that PFMT significantly reduced the incidence of urinary incontinence at 1-, 3-, and 6-month post-surgery, while there was no difference in the incidence of urinary incontinence at 12 months post-surgery (23), which may be related to the relatively few studies included in their study (only 4 articles). Although there is heterogeneity in the results of patient-reported incontinence at 3- and 6-month post-surgery in our results, these results still need to be treated with caution. Additionally, the ICIQ-UI SF questionnaire scores also showed that the scores of patients in the PFMT group significantly decreased, indicating that the patient’s urinary incontinence improved, but there was also a high degree of heterogeneity between studies.
There are some limitations in this study. First, some of the included literature did not mention the blind part, may lead to the low quality of the included literature. Secondly, the heterogeneity of some results may have an impact on the results.
ConclusionsOther Section
PFMT significantly improved stress urinary incontinence after prostatectomy, which can be improved by 2.77 times at most; however, due to the limited number of studies included and the heterogeneity of some of the results, further validation of the effectiveness of PFMT is still needed. Therefore, more high-quality studies need to be included for further exploration in the future.
AcknowledgmentsOther Section
We thank Dr. David E. Rapp (UVA Medical Center, Charlottesville, USA) and Francesco Del Giudice (“Sapienza” Rome University, Policlinico Umberto I Hospital, Rome, Italy) for the critical comments and valuable advice on this study.
Funding: The project was supported by Ningbo Yinzhou District Science and Technology Bureau (No. 2022AS032).
FootnoteOther Section
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-337/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-337/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-337/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Strojek K, Weber-Rajek M, Strączyńska A, et al. Randomized-Controlled Trial Examining the Effect of Pelvic Floor Muscle Training in the Treatment of Stress Urinary Incontinence in Men after a Laparoscopic Radical Prostatectomy Pilot Study. J Clin Med 2021;10:2946. [Crossref] [PubMed]
- Baumann FT, Reimer N, Gockeln T, et al. Supervised pelvic floor muscle exercise is more effective than unsupervised pelvic floor muscle exercise at improving urinary incontinence in prostate cancer patients following radical prostatectomy - a systematic review and meta-analysis. Disabil Rehabil 2022;44:5374-85. [Crossref] [PubMed]
- Li C, Zhang M, Wang J, et al. The 45-month therapy outcomes of permanent seed implantation and radical prostatectomy for prostate cancer patients. Invest New Drugs 2022;40:660-7. Erratum in: Invest New Drug 2022 Jul 5. [Crossref] [PubMed]
- Chung E, Wang J. The AdVance Sling and Male Sexual Function: A Prospective Analysis on the Impact of Pelvic Mesh on Erectile and Orgasmic Domains in Sexually Active Men With Postprostatectomy Stress Urinary Incontinence. Sex Med 2022;10:100529. [Crossref] [PubMed]
- Huang Y, Chen H. Analysis of the Influence of Nursing Safety Management on Nursing Quality in Hemodialysis Room. Comput Intell Neurosci 2022;2022:6327425. [Crossref] [PubMed]
- Ali M, Hutchison DD, Ortiz NM, et al. A narrative review of pelvic floor muscle training in the management of incontinence following prostate treatment. Transl Androl Urol 2022;11:1200-9. [Crossref] [PubMed]
- Kasai T, Banno T, Nakamura K, et al. Duration and Influencing Factors of Postoperative Urinary Incontinence after Robot-Assisted Radical Prostatectomy in a Japanese Community Hospital: A Single-Center Retrospective Cohort Study. Int J Environ Res Public Health 2023;20:4085. [Crossref] [PubMed]
- Canning A, Raison N, Aydin A, et al. A systematic review of treatment options for post-prostatectomy incontinence. World J Urol 2022;40:2617-26. [Crossref] [PubMed]
- Manassero F, Traversi C, Ales V, et al. Contribution of early intensive prolonged pelvic floor exercises on urinary continence recovery after bladder neck-sparing radical prostatectomy: results of a prospective controlled randomized trial. Neurourol Urodyn 2007;26:985-9. [Crossref] [PubMed]
- Aydın Sayılan A, Özbaş A. The Effect of Pelvic Floor Muscle Training On Incontinence Problems After Radical Prostatectomy. Am J Mens Health 2018;12:1007-15. [Crossref] [PubMed]
- de Lira GHS, Fornari A, Cardoso LF, et al. Effects of perioperative pelvic floor muscle training on early recovery of urinary continence and erectile function in men undergoing radical prostatectomy: a randomized clinical trial. Int Braz J Urol 2019;45:1196-203. [Crossref] [PubMed]
- Filocamo MT, Li Marzi V, Del Popolo G, et al. Effectiveness of early pelvic floor rehabilitation treatment for post-prostatectomy incontinence. Eur Urol 2005;48:734-8. [Crossref] [PubMed]
- Gezginci E, Goktas S, Ata A. Effect of perioperative pelvic floor muscle training program on incontinence and quality of life after radical prostatectomy: A randomized controlled trial. Clin Rehabil 2023;37:534-44. [Crossref] [PubMed]
- Hunter KF, Moore KN, Cody DJ, et al. Conservative management for postprostatectomy urinary incontinence. Cochrane Database Syst Rev 2004;CD001843. [PubMed]
- Higgins JP, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928. [Crossref] [PubMed]
- Van Kampen M, De Weerdt W, Van Poppel H, et al. Effect of pelvic-floor re-education on duration and degree of incontinence after radical prostatectomy: a randomised controlled trial. Lancet 2000;355:98-102. [Crossref] [PubMed]
- Glazener C, Boachie C, Buckley B, et al. Conservative treatment for urinary incontinence in Men After Prostate Surgery (MAPS): two parallel randomised controlled trials. Health Technol Assess 2011;15:1-290. iii-iv. [Crossref] [PubMed]
- Milios JE, Ackland TR, Green DJ. Pelvic floor muscle training in radical prostatectomy: a randomized controlled trial of the impacts on pelvic floor muscle function and urinary incontinence. BMC Urol 2019;19:116. [Crossref] [PubMed]
- Oh JJ, Kim JK, Lee H, et al. Effect of personalized extracorporeal biofeedback device for pelvic floor muscle training on urinary incontinence after robot-assisted radical prostatectomy: A randomized controlled trial. Neurourol Urodyn 2020;39:674-81. [Crossref] [PubMed]
- Jian X, Xin Y. Effect of intensive pelvic floor muscle training on temporary urinary incontinence in elderly patients undergoing transurethral resection of the prostate. Chinese General Practice Nursing 2020;18:2876-8.
- Zhong M, Li Q, Liu R. Effect of intensive pelvic floor muscle training on urinary incontinence in patients with benign prostatic hyperplasia undergoing electroresection. Journal of Guangdong Medical College 2022;40:433-5.
- Gentile F, La Civita E, Ventura BD, et al. A Neural Network Model Combining [-2]proPSA, freePSA, Total PSA, Cathepsin D, and Thrombospondin-1 Showed Increased Accuracy in the Identification of Clinically Significant Prostate Cancer. Cancers (Basel) 2023;15:1355. [Crossref] [PubMed]
- Rangganata E, Rahardjo HE. The Effect of Preoperative Pelvic Floor Muscle Training on Incontinence Problems after Radical Prostatectomy: A Meta-Analysis. Urol J 2021;18:380-8. [PubMed]
- Wang Y, Chen W, Li W. To Compare the Effects of two Pelvic Floor Muscle Treatments on Quality of Life and Sexual Function in Female Patients With Urinary Incontinence. Sex Med 2022;10:100561. [Crossref] [PubMed]
- Chang JI, Lam V, Patel MI. Preoperative Pelvic Floor Muscle Exercise and Postprostatectomy Incontinence: A Systematic Review and Meta-analysis. Eur Urol 2016;69:460-7. [Crossref] [PubMed]









