
The effectiveness of radionuclide scintigraphy in confirming testicular torsion at delayed presentation
Highlight box
Key findings
• Pain and swelling were common presenting complaint.
• No statistically significant relationship between clinical presentation and torsion.
• Prevalence of torsion was high—51% relative to other abnormal scrotal findings.
• 20% of patients presented with salvageable testis despite late presentation.
• All patients with positive scans underwent surgery and testicular torsion (TT) confirmed, indicating 100% sensitivity of testicular scintigraphy (TS) in confirming TT.
What is known and what is new?
• After the golden 6 hours, likelihood of testicular salvage is low. 20% were salvaged despite late presentation.
• Decrease tracer accumulation as scan time increases was appreciated in the salvaged group and increase tracer accumulation in the orchidectomy group was observed.
What is the implication, and what should change now?
• TS may be used to determine which testes are salvageable regardless of the time of presentation and as a gate keeper for surgery in patients who present late.
• More validation studies should be done.
Introduction
Testicular torsion (TT) is a twisting of the spermatic cord and its contents, which results in the reduction of the blood flow to the testicles (1). Anatomically TT is classified as extra-vaginal, torsion occurs at the level of the external inguinal ring usually only observed in neonates; and intra-vaginal, a more common variety seen in adolescents and young adults where there is an inability of the testis and epididymis to fixate onto the scrotum, this is referred to as a bell clapper deformity (2).
Studies have reported various prevalence rates of this condition. In male patients who presented with scrotal pain and/or swelling, the suspicion of TT ranges from 10.1% to 84.6% (1,3-5).
The global incidence of torsion in males below the age of 25 years is 1 in 4,000 annually (6-8). Early evaluation and management are essential for testicular salvage (4,8,9). Although doppler ultrasound (U/S) is the most common imaging study used, taken alone, it has been shown to yield a lower sensitivity compared to scintigraphy in missed TT (10).
Patient history, physical examination and urinalysis can usually indicate the diagnosis (11,12), but diagnosis of TT is only definitely confirmed at surgery. It has been recommended that imaging studies do not need to be performed if these clinical assessments are suggestive of torsion, and rather such a patient should undergo immediate surgical exploration if in doubt (13,14). Surgical intervention is the only effective treatment for intravaginal TT, with the best results noted if performed before the testes become necrotic optimal generally within 6 hours of the onset of symptoms (15). Fixing the contralateral testes is also mandatory as there is up to a 25% chance of the unaffected testes also undergoing TT in the future (4,7,13,15).
Several case reports have shown that most patients with TT present with sudden and often severe scrotal or testicular pain and swelling (16,17). Some patients present with acute abdominal pain and if the condition remains undiagnosed, the twisted testicle can cause major complications, mainly infarction and possible infertility (18). Having a clear knowledge of the clinical presentation, history, risk factors, and treatment is important to reduce delays in the diagnosis and management.
A diagnostic test that is simple, cheap, non-invasive, easily accessible with a superior sensitivity and specificity is favoured in clinical practice, and doppler U/S is considered the “gold standard”, with a sensitivity of 85–93%. Comparatively testicular scintigraphy (TS) has a superior sensitivity of 95% U/S (14,17).
TS is a non-invasive imaging study which evaluates testicular perfusion, differentiating a non-perfused testicle of acute torsion from the hyperemic tissues seen in epididymo-orchitis and other scrotal conditions which present with similar clinical symptoms. It is thus documented to have additional benefits of not only having a value-added diagnostic role in non-surgical testicular pathologies (7,8); but also its ability to classify the findings in terms of early, mid or late phase torsion (see Table 1), gives an added benefit to the role it plays in prompt diagnosis and surgical intervention. Successful intervention is highly dependent on the time of onset and presentation to the emergency department or urology department with a complaint of scrotal pain.
Table 1
| Types of torsion | Associated findings |
|---|---|
| Normal testis | · Homogenous tracer accumulation in both scrotum that is isointense with the background activity (thighs) |
| Early phase (acute torsion) | · Blood flow may appear normal or decreased to absent on the involved side |
| · A “nubbin” sign may be seen as a bump of activity extending medially from the iliac artery, denoting reactive increase in blood flow in the spermatic cord with abrupt termination | |
| · Static images show decreased tracer accumulation within the involved testicle without evidence of the surrounding halo of increased activity noted on later phases | |
| Mid phase | · After 6 hours of acute onset, with halo sign |
| · This halo gradually disappears on subsequent images | |
| Late phase (missed torsion) | · Irreversible testicular infarction has occurred |
| · Persistent halo sign |
Adapted from Lutzker LG, Zuckier LS. Testicular scanning and other applications of radionuclide imaging of the genital tract. Semin Nucl Med 1990;20:159-88. (19). 99mTc, technetium-99m.
Thus, we aimed to determine the effectiveness of testicular radionuclide scintigraphy in correctly diagnosing missed TT and its significance and role as an imaging modality in the management of these patients. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-116/rc).
Methods
A cohort of all patients, pediatric and adult, who underwent TS in Department of Nuclear Medicine at Dr George Mukhari Academic Hospital (DGMAH), during the period of January 2016 to December 2021 were included in our study. These consisted of patients who presented to the accident and emergency as well as the Urology outpatient departments with a history of acute scrotal pain.
The DGMAH picture archiving and communication system (PACS) and radiology information system (RIS) were used to access archived images and reports of all testicular scans done in the period 2016–2021 that were interpreted, approved and provided to the urology team for review.
Patient data was collected from patient files and hospital records. Clinical records, U/S and management notes on both surgical and non-surgical interventions, were reviewed.
In our department the protocol for TS involves the injection of technetium-99m (99mTc)-pertechnetate activity, that is calculated according to patient’s weight. There is no patient preparation required prior to the study, apart from adequate hydration. This activity is injected in a peripheral vein with the patient lying supine on the gamma camera bed. Dynamic images, representing the perfusion to the scrotal structures, are acquired immediately post injection followed by static images acquired 5 minutes later and at 5-minute intervals for 20 minutes. The images were acquired on the GE Healthcare SPECT/CT system (Chicago, USA).
The patients with suspected TT and positive TS scans were referred for surgical intervention. Intraoperatively the urologists determined the state of the testis by demonstrating reperfusion after detorsion in theatre. The assessment of viability of the testis is based on colour changes, from “dusky to pink”, after detorsion and wrapping of the testis in warm soaked surgical swab. They classify torsion as either complete (missed), intermittent torsion or torsion-detorsion syndrome (20).
The patients with incomplete information including no surgical notes, hospital file not found, images for the testicular scan not found on PACS, under their medical records were excluded from the study.
Data analysis
Data analysis was performed using STATA version 16. Continuous and categorical data were presented using the median and interquartile range and frequency/percentages, respectively. The association between age, clinical presentation, history and 99mTc results was performed using Fisher Exact test. A P value of less than 0.05 was considered statistically significant.
Ethical considerations
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Sefako Makgatho Health Sciences University Research Ethics Committee (Ref: SMUREC/M/78/2021:PG) and individual consent for this retrospective analysis was waived.
Results
During the study period, a total number of 68 patients (n=68) referred to the Department of Nuclear Medicine for evaluation of TT that met the inclusion criteria were evaluated. Their median age was 18.5 years with an interquartile range of 15–31 years. Slightly more than half (51%) were under 20 years of age (Table 2). Patients referred to Nuclear Medicine after presenting to casualty and/or urology, were imaged after the recommended 6 hours following the onset of symptoms with the presentation time ranging from 1 to 30 days, with a mean of 5 days.
Table 2
| Patient characteristics | N [%] |
|---|---|
| Age (years) | |
| <15 | 15 [22] |
| 15–19 | 20 [29] |
| 20–29 | 13 [19] |
| 30–39 | 9 [13] |
| 40+ | 11 [16] |
| Clinical presentation | |
| Pain | 67 [99] |
| Swelling | 46 [68] |
| History | |
| Trauma | 4 [6] |
| Non-trauma | 64 [94] |
The most common clinical presentation was acute testicular (scrotal) pain observed in almost all patients (99%) and a few, 4 (6%) cases had a history of trauma. The majority (97%) of the patients were African and 3% were Whites. There were no Coloureds or Indians in our sample.
Only 16% (n=11) of the patients had information of U/S. Of these, 36% (n=4) were positive for TT, 55% (n=6) were negative for TT and one of the patients had inconclusive findings. The patient whose U/S results were inconclusive was reported as negative for TT on TS imaging. The findings of one patient that had a positive U/S yet a negative TS were reported as being suggestive of epididimo-orchitis on TS.
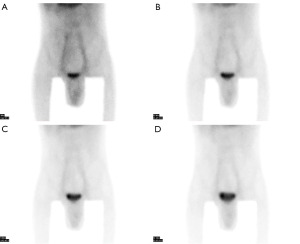
As shown in Figure 1, the findings of 99mTc-pertechnetate imaging indicate that 51% (n=35) of the patients had TT (Figure 2), all classified as missed torsion, and 49% (n=33) were negative or had alternative findings. All patients reported as positive for TT on the 99mTc-pertechnetate imaging (n=35) underwent a surgical operation, of which all were confirmed to have TT at surgery. Of this group, 7 (20%) had manual detorsion performed intraoperatively (intermittent torsion), 20 (57%) had missed torsion (complete torsion) and 8 (23%) had necrotic testes.

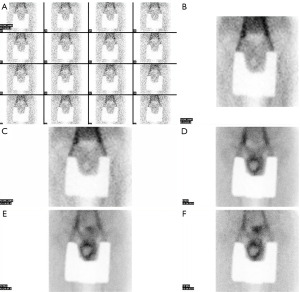
As shown in Table 3, of the patients who were negative for TT on 99mTc-pertechnetate imaging (n=33), 30% (n=10) of the patients had normal scans (Figure 3) while 70% (n=23) had abnormal results of which various scrotal abnormalities were encountered: 57% (n=13) were epididymitis (Figure 4), 13% (n=3) were orchitis and epididymitis in combination with orchitis accounting for 30% (n=7) of the cases.
Table 3
| Findings | N [%] |
|---|---|
| 99mTc results | |
| Positive for torsion | 35 [51] |
| Negative for torsion | 33 [49] |
| Other types of scrotal abnormalities (n=23) | |
| Epididymitis | 13 [57] |
| Orchitis | 3 [13] |
| Epididymo-orchitis | 7 [30] |
| Surgical findings (testicle involved) | |
| Left | 12 [34] |
| Right | 23 [66] |

Two thirds, 23 (66%), had TT on the right testis and 12 (34%) on the left testis. These results of the site involved were in agreement with our scan findings.
A significantly higher proportion of patients aged <15 years and those in the age group 15–19 years were confirmed to have TT compared to the other age groups (Table 4). There was no statistically significant relationship between clinical presentation, history and 99mTc results (P>0.05).
Table 4
| Patient characteristics | n | 99mTc results, n [%] | P value | |
|---|---|---|---|---|
| Positive for torsion (n=35) | Negative for torsion (n=33) | |||
| Age (years) | 0.008 | |||
| <15 | 15 | 10 [67] | 5 [33] | |
| 15–19 | 20 | 15 [75] | 5 [25] | |
| 20–24 | 8 | 4 [50] | 4 [50] | |
| 25–29 | 5 | 1 [20] | 4 [80] | |
| 30+ | 20 | 5 [25] | 15 [75] | |
| Clinical presentation | ||||
| Pain | 67 | 35 [52] | 32 [48] | 0.712 |
| Swelling | 46 | 27 [59] | 19 [41] | 0.152 |
| History | ||||
| Non-trauma | 64 | 34 [53] | 30 [47] | 0.606 |
99mTc, technetium-99m.
Discussion
TT is as a result of the twisting of the spermatic cord with the subsequent loss of blood supply to the affected testicle (1,20). The diagnosis and treatment of TT depend primarily on the findings on history and physical examination (10,11). The gravity of ischemia is variable and dependent on the time period of torsion including the extent of rotation of the cord (10,11,21).
It is recommended that if there is high suspicion of torsion on physical examination and history, prompt surgical exploration be performed and to not postpone it for imaging studies (12,13), so as to avoid testicular necrosis and subsequent orchidectomy (17). This management route is commonly adopted when the patient presents within the first 6 hours of onset of scrotal pain and or swelling (7,12,13).
In our setting we found there’s a significant delay in patient presentation to the emergency department. The majority of patients presented more than 6 hours to days after the onset of scrotal pain. The mean presentation time in our study, from time of onset of symptoms to presentation to the hospital, was 5 days. This was three times more than that found by Mukendi et al. (21), where the mean time of presentation following onset of symptoms was 36 hours. Hence in all our patients, TS was performed at “delayed” presentation of more than 6 hours after the onset of the various symptoms reported.
There are certain documented predisposing factors to TT, commonly bell clapper deformity, a horizontal lying testis, and trauma (22,23). Trauma induced TT is rare, reported at 1% of cases, which is consistent with our findings. Nearly all the patients, 99%, presented with a history of pain, 68% had associated swelling, and only 6% had a history of associated trauma. Of the trauma group, only 1 patient had a positive TS scan and went for surgery where an associated hematoma was found.
The mechanism of post traumatic torsion is believed to be due to sudden contraction of the cremaster muscle that surrounds the spermatic cord, and this results in TT, or hematoma formation or even rupture of affected testis (23). The clinical presentation of trauma alone, with doppler U/S examination does not negate the need for urgent surgical exploration in the management 1of trauma-included TT (24). In cases of scrotal trauma, there is mild to moderate increase in activity on TS and the presence of a hematoma a halo sign may be appreciated and this becomes indistinguishable to TT (19).
Similarly, studies have reported that patients with suspected TT often present with scrotal pain, swelling, and erythema (8,9,15,16). On physical examination there are differentiating features between TT and epididymitis, although they are said to be non-specific; importantly findings on doppler U/S are thickening of the spermatic cord with absent flow for positive TT result, a positive Phrens sign and angel sign in the latter (25-27). Then there is the “high riding” testicle that is observed in affected side but not in torsion of the testicular appendix (28).
Likewise, with other conditions such as testicular cancer, there is an irregular border of the testis also found with the pain and swelling (27).
Symptoms of pain and swelling reported by patients at clinical presentation were not sufficient to diagnose TT confidently in Lutzker and Zuckier’s study (19). In our study we could similarly not elicit a significant relationship between clinical presentation and TT. Our results showed that for those reported positive results for TT, 52% presented with pain and 59% with swelling, while in the group without TT, but other scrotal abnormalities or normal scans as indicated, a similar number demonstrated the same clinical presentation, notably, 48% presenting with pain and 47% who with swelling. We therefore could not demonstrate a statistically significant relationship between clinical presentation and TT (P>0.05) similar to Lutzker and Zuckier (19).
In our findings, TS indicated that 51% of the patients had positive findings for TT and 49% had negative findings. Scintigraphically, these findings were in keeping with features of missed torsion (see Table 1) and were reported as such. Considering the late presentation in our cohort, the dominant finding of missed torsion was expected, as those who present early are likely sent for U/S due to convenience and ease of logistics or go directly to theatre for exploration to increase the possibility of testicular salvage.
DaJusta et al. (7), in their review, established that the sensitivity of doppler U/S vs. high resolution U/S was 76% and 96% respectively. U/S being known in literature as the ‘gold-standard’ for diagnosis of acute TT (6,7), we evaluated the agreement between doppler US and TS in our setting. Patients that had both U/S and TS done were 16% (n=11) of the total study population, the reason for the low numbers of U/S cases on the PACS may be due to the referral system. U/S is a bedside examination, that may be done in casualty or in the ward, therefore there may be patients who didn’t get referred to radiology for their U/S thus no available reports.
The U/S reported positive TT in 36% of the patients and 55% were found to be negative. One patient had inconclusive findings and found on TS to be negative for TT. These results therefore showed a 90% concordance between U/S and TS.
All patients with positive results for missed TT on TS and US were referred for surgical exploration.
Looking at the surgical findings of suspected TT; Mukendi et al. (21) demonstrated in their study; that up to 63% of their study population had an orchidectomy due to missed (complete torsion) TT. Missed torsion was found in 80% of the positive cases in our study and resulted in orchidectomy, the difference in findings between these two studies could be due to the longer delay in presentation time in our setting. In our study testicular salvage in the positive TS patients with intermittent torsion was 20% and intraoperative manual detorsion was performed. Of those with missed torsion (complete torsion) 22% were found with testicular necrosis. Of great interest was the difference in findings on TS in the intermittent torsion vs. complete torsion group. We found that, decrease in tracer accumulation as scan time increases was appreciated in the testicular salvage group vs. increase in tracer accumulation in the orchidectomy group.
As cited in literature, epididymitis and orchitis or epididymo-orchitis often present as gradual onset of scrotal pain and swelling, these conditions affect males of any age and are found to be the most common cause of scrotal pain in the emergency department (15,16,25,26). In the scans reported to be negative for TT, epididymitis was the most prevalent abnormality, accounting for 57% of the cases, followed by 30% with epididymo-orchitis.
This study has several limitations. Majority of our patients presented after the golden 6 hours cut off for possible testicular salvaging (7,12,13), and our typical findings on TS were that of missed TT with no comparison group of early presenters. We desired to assess the correlation between TS and the surgical outcomes, but discovered that there was no histological data available, as the surgeons made a definitive diagnosis using their intra operative criteria for TT (acute or missed) and testicular necrosis. There was a bias in that only the patients who had positive TS results went to theatre.
In addition to that, because we are an imaging department we rely on referral from the treating surgeons and their knowledge and confidence in our study’s sensitivity and specificity in giving the correct diagnosis, and this may have affected the overall patient numbers that are frequently referred. Due to the low numbers of patients who had both TS and U/S, evaluating a comparison between TS, U/S and surgery could not be achieved.
Conclusions
In this study, the prevalence of TT noted on TS is relatively high (51%) compared to the other abnormal findings in the scrotum. Surgical exploration confirmed a diagnosis of missed (complete) TT in 80% of patients with positive TS, while in the rest they were able to salvage the torqued testes. This confirms that even in patients who present late, the need for surgical exploration is still warranted as there is still a possibility of salvage of the torqued testes in a few exceptional cases. The right testicle was affected more than the left. Our results also showed that there is a high concordance between TS and U/S in the evaluation of patients with suspected TT but further studies to validate these findings between TS and U/S are warranted In our study population all the patients with positive scans for TT underwent surgery and indeed the findings were TT, showing the high sensitivity of TS, and that TS is effective and reliable in confirming TT in our setting and may serve as an effective gate-keeper for surgery by excluding TT in other non-surgical testicular pathologies.
Acknowledgments
The author (NEN) would like to acknowledge her supervisors for their guidance, the Department of Nuclear Medicine and Urology for access to the data and to her husband and family for their support during this journey.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-116/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-116/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-116/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-116/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by institutional ethics board of Sefako Makgatho Health Sciences University Research Ethics Committee (Ref: SMUREC/M/78/2021:PG) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Guo X, Li S, Chen HT, et al. Clinical characterization of incomplete testicular torsion in children. Zhonghua Nan Ke Xue 2019;25:1005-10. [PubMed]
- Beni-Israel T, Goldman M, Bar Chaim S, et al. Clinical predictors for testicular torsion as seen in the pediatric ED. Am J Emerg Med 2010;28:786-9. [Crossref] [PubMed]
- Erdoğan A, Günay EC, Gündoğdu G, et al. Testicular torsion in the left inguinal canal in a patient with inguinal hernia: a difficult case to diagnose. Mol Imaging Radionucl Ther 2011;20:108-10. [Crossref] [PubMed]
- Srinivasan A, Cinman N, Feber KM, et al. History and physical examination findings predictive of testicular torsion: an attempt to promote clinical diagnosis by house staff. J Pediatr Urol 2011;7:470-4. [Crossref] [PubMed]
- Molokwu CN, Somani BK, Goodman CM. Outcomes of scrotal exploration for acute scrotal pain suspicious of testicular torsion: a consecutive case series of 173 patients. BJU Int 2011;107:990-3. [Crossref] [PubMed]
- Wang JH. Testicular torsion. Urological Science 2012;23:85-6. [Crossref]
- DaJusta DG, Granberg CF, Villanueva C, et al. Contemporary review of testicular torsion: new concepts, emerging technologies and potential therapeutics. J Pediatr Urol 2013;9:723-30. [Crossref] [PubMed]
- Yin S, Trainor JL. Diagnosis and management of testicular torsion, torsion of the appendix testis, and epididymitis. Clinical Pediatric Emergency Medicine 2009;10:38-44. [Crossref]
- Zhao LC, Lautz TB, Meeks JJ, et al. Pediatric testicular torsion epidemiology using a national database: incidence, risk of orchiectomy and possible measures toward improving the quality of care. J Urol 2011;186:2009-13. [Crossref] [PubMed]
- Lee SM, Huh JS, Baek M, et al. A nationwide epidemiological study of testicular torsion in Korea. J Korean Med Sci 2014;29:1684-7. [Crossref] [PubMed]
- Huang WY, Chen YF, Chang HC, et al. The incidence rate and characteristics in patients with testicular torsion: a nationwide, population-based study. Acta Paediatr 2013;102:e363-7. [Crossref] [PubMed]
- Feng S, Yang H, Lou Y, et al. Clinical Characteristics of Testicular Torsion and Identification of Predictors of Testicular Salvage in Children: A Retrospective Study in a Single Institution. Urol Int 2020;104:878-83. [Crossref] [PubMed]
- Tu L, Zhao YW, He J. Diagnosis and treatment of 109 cases of testicular torsion in children and adolescents. Zhonghua Nan Ke Xue 2019;25:46-49. [PubMed]
- Boettcher M, Bergholz R, Krebs TF, et al. Clinical predictors of testicular torsion in children. Urology 2012;79:670-4. [Crossref] [PubMed]
- Somekh E, Gorenstein A, Serour F. Acute epididymitis in boys: evidence of a post-infectious etiology. J Urol 2004;171:391-4; discussion 394. [Crossref] [PubMed]
- Graumann LA, Dietz HG, Stehr M. Urinalysis in children with epididymitis. Eur J Pediatr Surg 2010;20:247-9. [Crossref] [PubMed]
- Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and management. Am Fam Physician 2013;88:835-40. [PubMed]
- Keays M, Rosenberg H. Testicular torsion. CMAJ 2019;191:E792. [Crossref] [PubMed]
- Lutzker LG, Zuckier LS. Testicular scanning and other applications of radionuclide imaging of the genital tract. Semin Nucl Med 1990;20:159-88. [Crossref] [PubMed]
- Kawamura M, Kuribayashi S, Yamamichi G, et al. A Case of Prenatal Testicular Torsion. Hinyokika Kiyo 2016;62:389-91. [PubMed]
- Mukendi AM, Kruger D, Haffejee M. Characteristics and management of testicu-lar torsion in patients admitted to the Urology Department at Chris Hani Baragwanath Academic Hospital. African Journal of Urology 2020;26:26. [Crossref]
- Pakmanesh H, Alinejad M. A case of bilateral perinatal testicular torsion that presented with unilateral torsion; necessity of contralateral testis exploration. Turk J Urol 2018;44:511-4. [Crossref] [PubMed]
- Adlan T, Freeman SJ. Can ultrasound help to manage patients with scrotal trauma? Ultrasound 2014;22:205-12. [Crossref] [PubMed]
- Ogbetere FE. Traumatic testicular torsion: A call to look beyond the obvious. Urol Ann 2021;13:431-3. [Crossref] [PubMed]
- McConaghy JR, Panchal B. Epididymitis: An Overview. Am Fam Physician 2016;94:723-6. [PubMed]
- Bonner M, Sheele JM, Cantillo-Campos S, et al. A Descriptive Analysis of Men Diagnosed With Epididymitis, Orchitis, or Both in the Emergency Department. Cureus 2021;13:e15800. [Crossref] [PubMed]
- Roth B, Giannakis I, Ricklin ME, et al. An Accurate Diagnostic Pathway Helps to Correctly Distinguish Between the Possible Causes of Acute Scrotum. Oman Med J 2018;33:55-60. [Crossref] [PubMed]
- Hamzavi SS, Derakhshan D, Askari A, et al. Torsion of the Appendix Testis as a Presenting Feature of Multisystemic Inflammatory Syndrome in Children: A Case Report. Pediatr Infect Dis J 2021;40:e526-7. [Crossref] [PubMed]


