
Inflatable penile prosthesis placement in Peyronie’s disease: a review of surgical considerations, approaches, and maneuvers
Introduction
Peyronie’s disease (PD) is a wound-healing disorder in which a fibrous plaque develops within the tunica albuginea resulting in abnormal curvature or deformity of the penis. It most commonly presents as uniplanar or multiplanar curvature, with some PD patients having indentations, tapering, hourglass deformities, penile pain, hinge defects, or buckling during sexual activity. Variability exists regarding the reported prevalence of PD in the United States, with estimates ranging between 0.5–13.1% depending on the study population (1). Concomitant erectile dysfunction (ED) is also common in patients with PD, with a prevalence of up to 58% (1,2). Treatment for PD is typically reserved for patients in the chronic stage of the disease and includes traction, intralesional therapies, and surgery. In settings where medical treatment has failed and or in patients who desire a more rapid and definitive treatment, surgery for PD should be considered. Surgical options include penile plication, plaque incision/excision with grafting, and penile prosthesis with or without adjunct straightening maneuvers. In men with concomitant ED refractory to medical therapy and PD, the gold standard treatment is an inflatable penile prosthesis (IPP) which may correct the curvature in isolation or require additional adjunct procedures. Herein, we will review the indications, patient selection criteria, approaches to IPP surgery as well as adjunct procedures for curvature correction, postoperative care and satisfaction in patients with PD and refractory ED.
Indications
IPP is indicated in patients with PD and concomitant ED when patients have failed medical therapy or in men with severe, complex deformities with risk factors for ED.
The initial evaluation of a patient with PD involves a complete history and physical examination (PE). History should include the duration of PD, rated past/current penile pain, stable vs. chronic phase, direction and degree of curvature or deformity, palpable plaque, history of congenital penile curvature patient and partner bother, along with associated conditions, like Dupuytren’s contracture (1,2). Assessment of erectile function is paramount, as well as any prior therapies tried, duration of sexual dysfunction, penile sensation, ejaculatory ability, erection sufficiency, and any co-morbid conditions that may affect ED, difficulty/pain with penetrative intercourse, and concerns regarding penile length and girth (1,2). PE should note the location of any palpable plaques, girth, indentations or other deformities, and penile length. A diagnosis of PD can be made from the history and physical exam, but American Urological Association (AUA) guidelines also recommend further assessment of curvature using intracavernosal injections (ICI) with or without penile duplex Doppler ultrasound (PDDUS) (1). ICIs allow for accurate assessment of the penile deformity, plaque(s), pain, determination of the point of maximum curvature, erectile function, measurement of penile length, and girth of the erect penis (1). PDDUS is an adjunctive test to ICI that provides additional information regarding the vascular integrity of the penis, erectile function, and plaque characteristics such as density and calcification, which can be helpful for surgical planning (1,2).
There is variability in the definitions of acute vs. chronic phase of PD, with the chronic stage defined as when there is absent or subsiding pain and or the deformity has been stable without change for 3 months (3). Typically, IPP is performed in the chronic phase of PD. However, intervention may be considered in the acute phase as evidence suggests early treatment with an IPP may preserve penile length secondary to plaque formation, corporal atrophy, and fibrosis (4,5).
Patient selection
The patient selection process is imperative in ensuring satisfactory outcomes in IPP implantation. Following the assessment of the patient, a shared decision-making process should be had, which details the risks and benefits of IPP. The patient should be informed of alternative therapies for ED and PD, including medications, traction, intralesional therapies, and other available surgical procedures. The patient should meet the previously discussed criteria for IPP implantation as well (1,6).
Setting patient expectations prior to placement of an IPP will ensure the patient understands the possible risks, benefits, and outcomes of the procedure, leading to higher satisfaction. Significant risks to discuss include the possibility of penile shortening, persistent or recurrent curvature, infection, device malfunction, and the need for additional procedures. It should be made clear that the goal of surgery is not to perfectly straighten the penis but to allow for a functionally straight erection satisfactory for penetration (6,7). Patients should be informed that a penile implant should not significantly impact penile size, ejaculation, orgasmic function, libido, or penile sensation (1). As with any procedure, fully informed consent should be obtained prior to surgery. Trost et al. identified a subset of seven traits to regard with caution in patients pursuing IPP surgery, largely due to the increased risk of post-op dissatisfaction (7,8). He defined these high-risk traits in the mnemonic, “CURSED Patient” which stands for: compulsive/obsessive, unrealistic, revision, surgeon shopping, entitled, denial, and psychiatric (8). Patients who are adequately informed and accept realistic outcomes are ideal candidates for IPP and exhibit high satisfaction post-procedure.
Not all patients meet the criteria for an IPP, and a malleable penile prosthetic (MPP) may be a viable alternative. Indications for the preferential use of MPP include diminished hand strength/dexterity, body habitus/anatomy, cost, and avoidance of potential mechanical failure (9,10). In addition, there are numerous methods to prognosticate patient outcomes prior to surgical intervention, specifically looking at frailty. While there remains a lack of utilization of patient frailty in sexual medicine, at a minimum, the application of patient grip strength prior to prosthetic procedures could significantly improve patient outcomes and help predict which patients may be at increased risk of prolonged recovery with pain or have more challenges with device manipulation/instruction postoperatively, and whom may be better candidates for MPP (11). Habous et al. found no significant difference in satisfaction rates between patients receiving an MPP or IPP for the treatment of PD (9). While IPP is the modern choice for the treatment of PD with refractory ED, MPP can still be of use in particular patients (9). Proper patient selection is imperative for successful outcomes.
Adjunctive procedures during IPP placement for PD
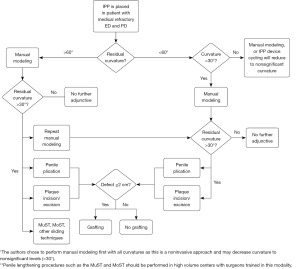
An understanding of the extent and degree of penile deformity in the patient prior to IPP surgery can help with surgical planning and anticipation of potential adjunctive procedures needed to achieve straightening (2). There are several adjunctive maneuvers that may be performed to accomplish straightening during IPP placement, including penile modeling, plication with or without grafting, and plaque excision/incision with grafting (1,6). Manual modeling alone can be attempted in most men with a residual curvature <30-degrees following IPP implant, however it may be successful in patients with curvatures <60-degrees (12). Plication techniques are employed if significant residual curvature is still present following modeling or if it exceeds 30 degrees after IPP insertion (6,12). Plaque excision/incision with grafting procedures may be used in cases of severe PD with curvatures >60 degrees, ventral curvature, and/or large plaques, or in men with concerns over penile length loss (6,12,13). Figure 1 demonstrates a flowchart for intra-operative decision-making, including author recommendations. Modeling is the least invasive approach with minimal side effects or complications and should be tried before more invasive measures even in patients with up to 60 degrees of curvature. In patients where the loss of length is a concern, traction therapy or a vacuum erection device (VED) may be used as adjunctive therapy preoperatively (1,7). Levine and Rybak demonstrated that daily penile traction device use for 2–4 hours up to 4 months prior to IPP surgery resulted in 70% of ED patients having postoperative stretched penile length gain up to 1.5 cm when compared to their preoperative measurements (14). Data shows use of VED for 10–15 min daily one month prior to IPP placement increased stretched penile length in patients by an average of 0.80 cm (15). Multiple approaches may be employed for adjunct straightening procedures with IPP; each with its own advantages, and limitations highlighted below (Figure 1).
Modeling
The goal of an IPP is to restore erectile function of the patient, but it may also correct curvature. (16) Dilation of the corpora during IPP placement frequently breaks through the fibrotic plaque and struts to allow for curvature correction. Mulhall et al. reported that 61% of men with a mean curvature of 35 degrees (range, 25–95 degrees) treated with an IPP had their curvature reduced to less than 10 degrees with IPP placement alone (16). Chung et al. also showed in their study population with a mean curvature of 49 degrees (15–90 degrees) that 91% of the men had their curvature reduced by IPP alone to less than 10 degrees (17). The ability to remedy both issues with one procedure has made IPP the gold standard for treatment of PD with concurrent ED (16-18). Despite this, sometimes additional maneuvers are warranted to create a functionally straight erection.
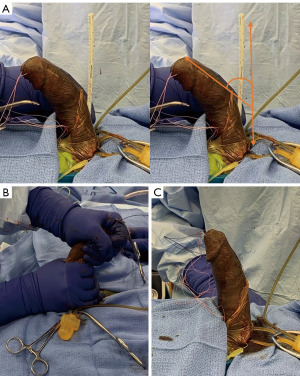
Manual modeling was first introduced by Delk and Wilson in 1994 (19). To perform this, the IPP is inflated to maximal rigidity. Then to prevent back pressure on the pump, a pair of rubber shodded hemostats are used to clamp the IPP tubing from the cylinders to the pump (3,13). Once the rubber shods are placed, the penis is bent contralateral to the curvature and held for 90 seconds, with the bottom hand stabilizing the base of the penis and the corporotomies, and the top hand grasping the distal shaft and glans firmly to protect the corpora from cylinder extrusion and the urethra from rupture as shown in the illustration in Figures 2,3 (3). This process may be repeated as needed for straightening (3,13).

A case series found that 30% of patients with PD who had an IPP inserted would need additional straightening procedures to correct residual curvature (>10–20 degrees) (13). They found the success rate of manual modeling to be 84% in men with an IPP and 54% in men with a malleable device, with no urethral damage reported (13).
In the initial modeling study by Wilson and Delk, the success rate was 86% in a cohort of 118 patients, and the most common complication was urethral perforation in 3% of patients. Figure 3 demonstrates a functionally straight erection following modeling in a man with 50-degree curvature (19). In a recent study by Lucas et al., they sought to optimize the modeling procedure. Their results showed a mean preoperative curvature of 47.8 degrees and a mean postoperative curvature of 10.6 degrees, a significant decrease in all 40 patients requiring additional straightening following IPP insertion (20). They also suggested that by applying significant glandular pressure, urethral perforation can be avoided, as no complications were observed in their procedure, potentially correcting a weakness in the original method presented by Wilson and Delk (19,20) (Figure 3). Wilson et al. later performed a long-term follow-up of their initial cohort, finding no significant difference in the penile prosthetic survival rate between modeling and non-modeling groups, concluding no significant damage was done by the modeling process (21). Current AUA guidelines published in 2015 moderately recommend adjunctive intraoperative procedures such as modeling, plication or incision/grafting, giving them a C evidence grading (1).
One novel option for patients with residual curvature following IPP is home modeling (22). A study performed in 2020 by Moncada et al. sought to evaluate the effectiveness of a home modeling protocol in patients with a residual curvature of <45 degrees following intra-operative modeling (22). In this study of 92 men (average age 62.8 years), there was a significant reduction in curvature following home modeling, and at 3 months, 85.5% of patients had curvature <10 degrees, and at 6 months, 94.7% saw the same result (22). This study included 18 men with diabetes, 26 with hypertension, and 12 with cardiovascular disease. Despite these potential comorbidities, the success rate was still significant (22). This pilot study shows strong evidence that home modeling can be an effective adjunctive measure for patients with residual curvature, while avoiding further surgical intervention (22). Following the insertion of an IPP with or without modeling, residual curvature may still be present. Curvature of less than 30 degrees is not an indication for further procedures as the curvature is likely to resolve with device cycling on its own over the following year (23,24).
Penile plication
Penile plication for the treatment of PD without ED has a long history, with the first described plication technique by Nesbit in 1965 (25). The overall goal of penile plication, regardless of technique, is to place permanent sutures on the convex side of the penis to shorten it, thereby correcting the curvature resulting in penile straightening (16). Modern plication technique began with the 16-dot technique introduced by Gholami and Lue (26). In this method, either a circumcision or longitudinal incision can be used (26). Following incision, 16 dots are marked bilaterally which serve as the marker for suture placement (26). Each group of four dots corresponds to one suture, and they are placed individually until satisfactory curvature reduction is achieved (26,27).
The Kiel Knot technique, as described by Cordon et al., is a modified 16-dot procedure which utilizes two dots for each suture, reducing the distance between dots to limit suture prominence and sexual discomfort (27). Both of these techniques may require degloving of the shaft, which can cause surgical trauma (26,27). Chung et al. described a novel method of plication in which only a small upper scrotal longitudinal incision is needed to insert the corrective sutures (28). Once the incision is made, a series of parallel, inverting sutures are placed and tied immediately. This is continued until satisfactory curvature reduction is achieved (28). They later applied this method to patients undergoing IPP implantation, and found it to be successful (29). A significant benefit of this method is that it allows for the insertion of the IPP following plication, without multiple incisions, reducing potential surgical trauma (29). The upper scrotal longitudinal incision used for plication is retracted proximally to the standard penoscrotal (PS) junction used for PS IPP placement, allowing implantation without an additional incision (29).
A common patient concern with plication is the penile shortening that accompanies it (29). Chung et al. reported a subjective decrease in penis length for 73% of patients that underwent plication procedure, despite all 15 patients reporting improved curvature (29). This study highlights both the high success rate of this surgery and the potential issues it brings about for patients (29). Syed et al. found that of 42 men, 38.1% reported a subjective loss in penile length with no effect on sexual intercourse, and 11.9% had disabling penile length loss (30). Taylor and Levine found that of 61 patients, 69% reported subjective shortening, whereas objective shortening was found only in 18% of the patients (31). The method of measurement was unclear in these studies, which serves as a limitation to the findings (28,30,31). This significant rate of shortening, whether subjective or objective, is concerning for patients, and should be discussed prior to treatment. Current AUA guidelines state that tunical plication surgery may be used in patients with adequate rigidity for intercourse (1). This is a moderate recommendation with a C evidence strength grade (1).
Penile plication as an adjunctive treatment to penile prosthetic insertion was first introduced by Rahman et al. in 2004 (32). Coming nearly 40 years after plication had begun being used for PD (24). In this study, 5 patients who had undergone previous failed treatments for PD with concurrent ED were treated with IPP and additional intraoperative plication (32). Up to 36 months following the procedure, no complications were reported, and the curvature was corrected (32). In alignment with Rahman et al., current surgical algorithms for PD state that plication should be used following attempts at manual modeling intraoperatively after IPP placement for residual curvature >30 degrees (13,19,32). As Ziegelmann et al., describes this method, the sutures are placed prior to the insertion of the IPP (33). If the curvature is persistent following IPP insertion and modeling attempts, then the sutures are secured as to straighten the penis, if the curvature is corrected via IPP alone or modeling, the sutures are removed (33). Tausch et al. performed a retrospective study in which 23 patients were treated with plication and IPP insertion, they found that curvature was reduced from an average of 38 degrees to <10 degrees postoperatively, demonstrating the effectiveness of plication and IPP in reducing curvature (34). Due to the small sample size, however, it is difficult to extrapolate this data. The AUA stated in their 2015 guidelines on PD that the literature on procedures with IPP and plication is limited by its sample size and diversity of techniques used, which makes it difficult to assess (1).
A novel curve reduction method introduced by Perito and Wilson is described as the Peyronie’s plaque “Scratch” technique, which utilizes a hook-bladed knife to manually disrupt the fibrous plaque causing the curvature within the corpus cavernosum (35). The goal of this technique is to limit additional procedures following IPP insertion and improve the efficacy of modeling (35). Prior treatment with collagenase clostridium histolyticum (CCH) or Xiaflex for patients with PD is not a contraindication to penile plication or plaque excision and grafting (PEG) though most experts recommend waiting 3 to 6 months post Xiaflex prior to surgery (36).
Plaque incision/excision with grafting
Plaque Incision/Excision with grafting can be used as an adjunct alongside IPP placement to help minimize residual curvature and maximize penile lengthening post placement. There are multiple surgical techniques that can be used to perform this procedure and it is typically used in patients with greater residual curvature or deformity, and those concerned about penile length loss. Incisions are typically made in the plaque at the point of maximum curvature on the concave side though other surgeons may make multiple relaxing incisions, circumferential incisions of the tunica, or lengthening or sliding techniques. Grafting can be omitted if the tunical defect is less than 2 cm (4). Grafting techniques can be further grouped into circumferential tunical incisions with grafting, simple plaque incision or excisions with grafting and the penile lengthening or sliding techniques with grafting (Figures 4,5).
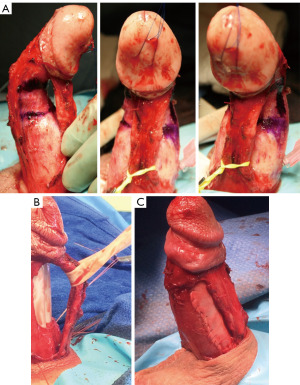

Sansalone et al. describes a technique of plaque incision with circumferential grafting at the time of IPP insertion in a group of 23 patients with mean curvature >70 degrees. Surgery is performed through a combined subcoronal (SC) and PS approach resulting in maximum exposure of the penile shaft. Buck’s fascia and urethra are dissected off the corpora followed by induction of an artificial erection (37). Penile circumference is measured to determine total girth of graft (37). Two lines tangential to the penile axis are drawn on the proximal and distal straight segments of the shaft and their intersection is indicated at the point of maximal curvature (37). At the level of maximal curvature, a circumferential incision of the tunica albuginea is performed, with the dimension of the defect measured with the penis in traction (37). The patch graft is then inserted within the defect and attached with a continuous 4-0 polydioxanone suture (37). Once the graft has been put in place they proceed with penile prothesis insertion (37).
In their study, a total of 23 patients (mean age 53 years) with stable PD, refractory ED, and severe penile shortening underwent the procedure. Patients gained an average length of 2.8 cm (37). No intraoperative complications were noted. Postoperatively, 3 patients developed minor wound dehiscence, 4 had diminished glans sensitivity, and 3 had residual curvature of <15 degrees. Eighteen patients reported feeling overall satisfied with the cosmetic and functional results of surgery (37). Compared to IPP placement alone, Sansalone et al. concluded that concomitant circumferential grafting with IPP placement helps prevent further shortening and improves lengthening, translating to patient satisfaction rates of 90%.
Choi and Lee described a circumferential grafting approach utilizing bovine pericardium graft material through an H-shaped incision made at the point of maximum deformity of the tunica albuginea (38). This allows for correction of the defect and circumferential implantation of the graft without circumferential incision of the tunica albuginea. In the study, they followed a cohort of 21 patients with severe PD (median curvature 70 degrees), without ED for 1 year post-procedure. Primary outcomes included PDDUS measurements peak systolic velocity (PSV), end-diastolic velocity (EDV), and resistive index (RI) in both the left and right corpus cavernosum, and degree of residual curvature. Findings revealed no significant differences between PSV, EDV, and RI pre vs. 1 year post-procedure and a significant sustained reduction in curvature (median curvature 70 degrees at time of surgery vs. median curvature 5 degrees 1 year post procedure, P<0.001). This cohort did not have ED at the time of grafting and did not undergo simultaneous IPP, no subjects developed ED in the post-procedural period (38).
Plaque excision with grafting can be used to excise the fibrotic plaque causing curvature or deformity in PD patients with significant PD and those desiring preservation penile length. This approach has proven to be viable in patients with significant PD and those desiring preservation of penile length (31,39). A novel approach to plaque excision/incision and grafting was introduced by Hatzichristodoulou et al., in 2013 which utilized a collagen fleece, such as Tachosil, for extratunical grafting material to reduce operative time by avoiding the need for exact measurement and suturing (39). In this technique, the penis is degloved via a circumcising incision to reveal the tunical defect, and excision of the plaque is performed on the concave side of the curvature to remove the entirety of the plaque. The collagen fleece is tailored to cover the tunical defect, soaked with physiological saline, applied, and compressed for 3 minutes (39). In their initial feasibility study of 70 patients, no major complications were observed, with pain being the most frequent complaint (34.9%). This study was limited by its short follow-up time of 5.2 days (39). A later study by Fernández-Pascual et al., with a longer follow-up time assessed the efficacy of this grafting technique in 27 patients receiving an IPP and found the method to be safe and effective, with an average length gain of 2.7 cm and no major complications reported (40). Plaque incision or excision with placement of extratunical TachoSil graft is safe and results yield a functionally straight erection with length preservation, and lower operative times than traditional grafts (Figure 5).
Penile lengthening techniques
In the “Sliding Technique” first described by Rolle et al., a ventro-dorsal incision of the tunica albuginea is made, and a double dorsal-ventral patch grafting with porcine small intestinal submucosa is placed over the defects once the cylinders are in place. To start a 4-cm longitudinal incision is made on the sides of the two corpora cavernosa, one at the 3 o’clock position of the left side and the other at the 9 o’clock position on the right. Two dorsal semicircular incisions are then made in the dorsal and lateral positions to connect the upper and lower ends of the lateral incisions (41). Incision and dissection of the tunica albuginea from the cavernous tissue and from the septum is performed in tandem with gentle traction applied to the glans to lengthen the distal and proximal ends. Once the neurovascular bundle reaches maximum length, two 3/0 polyglycolic sutures are applied to the lateral portions of the albuginea and the cylinders of the prosthesis are inserted in the corpora cavernosa (41). Finally, two rectangular grafts of 3.5 cm × 4 cm porcine small intestinal submucosa are added to cover the loss of substance (41).
This procedure was completed on three patients who presented with documented PD and chief complaints including: penile shortening, ED, and inability to satisfy their sexual partners. Curvature was minimal. The patients experienced postoperative penile lengthening of 4, 2.5, and 3 cm respectively (41). The patients were able to resume sexual intercourse, reported high levels of satisfaction, and had no significant loss of sensitivity nor any signs of vascular distress of the glans at the 3-, 6-, and 12-month follow-ups. No complications were reported (41).
Overall, the “sliding technique” helps to combine the effectiveness of the classical circular incision’s length gain with an improved safety profile, as the stabilization of the penis with the two transverse incisions with sutures allows for the prosthesis to be inserted without risk of longitudinal traction on the neurovascular bundle and the urethra (41). Unfortunately, this study is significantly underpowered and larger cohorts are needed to better evaluate outcomes along with the possible risks of glans ischemia and penile prosthesis erosion (41). Egydio et al. introduced a modified sliding technique (MoST) that improved upon the original sliding technique described by Rolle et al. This modified version uses no graft and instead makes use of the Buck’s fascia by repositioning it to cover the dorsal and ventral tunical defects (41,42). This modified procedure was performed on 143 patients all of whom had ED; with concomitant PD identified in 77/143 (42). The majority of the cohort (133/143) received malleable penile prostheses (MPP) vs. 10/143 received IPP. The average penile length gain was 3.1 cm at the 6-month follow-up.
Patient satisfaction was improved as measured by the International Index of Erectile Function (IIEF) questionnaire, where the average points increased from 24 points prior to surgery to 60 points at the 6-month follow-up with 79.7% of the patients completing the questionnaire (42). With the benefit of not needing to spend time to suture the graft to the tunica albuginea, Egydio et al. reported operative times averaging around 90 min for MPP and 120 min for IPP while still maintaining good outcomes. This is in contrast to Rolle et al. who reported average operative times of 170 min (41,42). A noted potential complication of the MoST technique is hematoma formation causing bulging or herniation of the prosthesis cylinders through the incision site due to failure to adequately cover the corpora cavernosa. However, no incidents of this were reported in this cohort of patients described by Egydio et al. (42) (Figure 6).

A further advancement of the grafting, sliding, and MoST techniques is the multi-slit technique (MuST), introduced by Egydio and Kuehhas (43) (Figure 7). This technique introduced the idea of making multiple horizontal slits in the tunica albuginea, rather than one large defect, as in the MoST. Figure 7A demonstrates the horizontal slits of the technique. The MuST does not require the use of grafting and Buck’s fascia is used to cover the defects in the tunica albuginea as seen in Figure 7. Following the sliding procedure, the prosthetic is inserted through two additional proximal corporotomies (43). Injection and irrigation with alprostadil or papaverine are done throughout the sliding procedure to reduce glans ischemia, a feared complication of sliding procedures (43).

This modified technique was created to reduce the risk of bulging defects which have been linked to the large tunical defects needed for the MoST procedure (43). This updated technique was used on 138 men, of which 81 were PD patients with a mean curvature of 55 degrees. The mean follow-up following surgery was 15.2 months. All men who presented with penile curvature saw successful straightening, and of all patients, a 3.6 cm length gain was reported. The most common postoperative complication in this population was hematoma at the base of the penis in 18.8% of patients, all of which spontaneously resolved without intervention (43). An advantage of sliding techniques is the preservation and gain of length in men with severe PD with minimal residual curvature. However, sliding techniques are more complex and require highly skilled and experienced surgeons.
Surgical approach and incision
Choosing the appropriate surgical approach and incision is an equally important part of the case. The most commonly utilized surgical approaches to IPP include PS, infrapubic (IP), and SC (44); each denoted by respective incision site. The choice of approach is largely dictated by surgeon preference and comfort level with the procedure, as each approach comes with associated benefits and risks (44). Particular approaches may also lend themselves particularly well or poorly to certain intraoperative adjunct procedures; an important consideration for patients undergoing a penile implant. Previous studies indicate that the PS and IP techniques are the two most commonly utilized approaches to IPP implantation with roughly 60–85% of surgeons displaying a preference for the PS approach (44). Table 1 has been provided to address the pros and cons of each surgical approach in the context of PD patients.
Table 1
| Approach | Advantages | Disadvantages |
|---|---|---|
| Infrapubic | Direct visualization of reservoir location | Separate incision required for graft placement |
| Facilitates “scratch” technique | Possible dorsal penile nerve injury | |
| Reduced surgical time and post-op scrotal swelling allows sooner device activation | More difficult cylinder placement | |
| Penoscrotal | Lends itself to adjunctive procedures as well as plaque incision/excision | Blind reservoir placement or need for ectopic reservoir placement |
| Plication can easily be performed by retracting incision proximally or laterally | Risk of injury to urethra | |
| Less loss of length compared with infrapubic | Postoperative scrotal swelling leading to delayed device activation | |
| Subcoronal | Direct visualization of plaques for incision/excision | More invasive, leading to greater risk of complications such as glans necrosis |
| Single incision may lead to better cosmetic outcomes |
IPP, inflatable penile prosthesis; PD, Peyronie’s disease.
PS approach
Barry and Seifert first described the PS approach in 1979 (45). One benefit of the PS approach is that it allows for excellent exposure of the proximal and distal corpora cavernosa in patients with co-morbidities such as obesity or corporal fibrosis (46). Another potential benefit of this approach is minimal risk of injury to the dorsal neurovascular bundle (46). If an artificial urinary sphincter is required, this approach also allows for implantation at the same time as IPP placement (46). A significant difference in length of the penile prosthesis was found in previous studies when comparing PS to the IP approach, 22.3 vs. 20.6 cm long, respectively (47). The PS approach lends itself well to concomitant adjunctive curvature correction procedures used to treat mild to severe PD, including modeling, plication, and/or plaque incision/excision with grafting, as it is possible to extend the incision vertically along the shaft to perform any of these adjunct procedures, or address cases of distal fibrosis (46,48,49). Chung et al. also describe their use of a single upper scrotal incision to perform plication followed by IPP placement through the same incision using a PS approach (29). Limitations for this approach include lack of direct visibility when placing the reservoir into the space of Retzius, requiring “blind placement” through the inguinal canal, however, some of this risk may be mitigated with blunt finger dissection, staying closer to midline and a low threshold to initiate ectopic implantation of the reservoir if needed (46). Postoperative scrotal swelling is a potential complication of the PS approach, and resultant pain may result in a delay in device activation (46). Postoperative scrotal swelling is the most common complaint of the PS approach (46), frequent to the point that it is often regarded as an expected side effect of surgery rather than a true complication. Based on the anatomic location of the incision, there is a theoretical risk of urethral injury, however, this risk can be mitigated by proper retraction of the proximal urethra during corporal incision; use of a foley catheter, and intraoperative safety checks to identify any urethral injuries sustained during dilation (44,46).
IP approach
The IP approach was first described by DM Barrett in 1985 (50). Since inception, the IP approach has been progressively refined to minimize invasiveness and operative time. The IP approach is unique in that it allows for direct visualization of the reservoir during placement (51), but this comes at the expense of more limited access to the distal corpora cavernosa and scrotum for distal cylinder and pump placement respectively (44). In addition, it can make it challenging to perform adjunctive curvature correction procedures for PD depending on the location of the curvature or deformity. Antonini et al. described a novel “scratch technique” that can be applied in the early steps of IPP procedures utilizing an IP approach (52). Following induction of an artificial erection utilizing normal saline, the erect penis is assessed for deformities. Those with curvature >30 degrees, hourglass malformation, or penile indentation are considered candidates for the scratch technique; which involves placement of a nasal speculum through the IP incision and across the plaque; followed by opening to disrupt the plaque along the x-axis. Additional disruption longitudinally and deep is performed with a 12-blade scalpel. Once disruption is complete, the IPP insertion is continued via routine IP approach, with the option to provide additional modeling during rapid inflation following cylinder implant (52). They note that this endocavernous approach is less invasive and less time consuming in contrast to grafting (52).
Direct visualization of the reservoir also enhances the relative speed of the IP approach leading to shortened operative times (53). An additional cited advantage of the IP approach is reduction of scrotal edema/swelling post procedure, thus allowing for faster recovery and faster time to penile prosthesis activation (53). A small single center study performed by Grande et al., comprised of 42 patients (21 IP vs. 21 PS) found that 19% of IP patients were able to activate their prosthesis within 4 weeks of implant vs. 0% in the PS group. Number of first activations normalized between 4–6 weeks (33% IP vs. 38% PS) (53).
A study of urology resident perspectives regarding the IP procedure performed at the University of Maryland found that while confidence and speed using the IP approach improved rapidly over 15 trial cases, placement of the distal cylinders remained a constant challenge throughout (54). This finding was replicated in regards to pump placement as well, with residents citing both of these aspects of the IP procedure as “more difficult” or “much more difficult” when contrasted to the PS approach (54). Of note, placement of cylinders may be further complicated by severe penile plaque and fibrosis in patients with PD, and may prove to be even more difficult under these circumstances potentially limiting the utility of the IP approach for known PD patients.
Dorsal penile nerve injury, while rare, is a major irreversible complication of the IP approach, however hard data quantifying this risk is sparse in current literature. Otero et al. mentioned a theoretical risk during re-incision of the corpora for revision surgery; citing electrocautery use during re-incision of the corpora vs. the typical use of a scalpel to incise the corpora during primary implant as the potential mechanism of damage. They cite two incidents that occurred in the late 1980’s, during the infancy of the IP approach (44). In performing over 4,000 IPP implants utilizing IP approach, Perito et al. also failed to identify a single case of glandular hypoesthesia or anesthesia indicative of dorsal penile nerve injury (55). Of course, these reports do not negate this risk entirely, as it is possible that lack of data is simply a result of failure of surgeons to disclose this complication or publish on it. However, based on current literature, it would appear the dorsal penile nerve injury in the context of the IP approach is exceedingly rare in an experienced implanter.
SC approach
The SC approach was first described in 1981 for use with semi-rigid penile implants and later described by Weinberg et al. for use with IPP in 2016 (56). The SC incision is a circumferential incision that degloves the penis down to the level of the PS junction, providing full exposure of the corpora cavernosa and urethra (56). This approach allows complete access to the penile shaft to perform any of the adjunctive curvature correction or reconstructive procedures concomitantly used for PD patients during IPP placement (56). The single incision may also allow for a more optimal cosmetic appearance for the patient with less scrotal swelling and earlier pump activation training (56). In a study of 200 patients with SC placed IPPs, 92 had PD plaques that were treated after IPP placement. Additionally, 16% had their IPP revised and exchanged, all through the SC incision using a proximal corporal incision. Average surgical time was 73 min (56). Using this method, only 1.5% of patients developed an infection and one patient had a revision surgery to alleviate distal erosion at 8 months post-op (56). In addition, the SC approach may allow for easier placement of plications as well as plaque incision with grafting, due to visibility of the plaques (57). As such the benefits of SC approach are greater for patients with known PD, than for non-PD patients and may warrant its use. For low-volume implanters, or surgeons who do not anticipate plaque incision in patients with PD, the other approaches may be more appropriate due to comfort level and less risk of complications.
Degloving of the penis has fallen out of favor with some surgeons, due to the reported complications associated with the SC approach including sensory deficits, glans necrosis, skin loss or sloughing, and lymphedema (57,58). More operative time is required when compared to the PS or IP approach, likely because closure of the dartos fascia and circumcising incision are more time consuming (44,57,58). In addition, most reconstruction procedures including penile fracture repairs, penile skin flap urethroplasties and plications for PD have moved away from degloving of the penis to alternative incisions. This approach has had favorable results in high volume centers; however, widespread use may not be as favorable due to an increase in these complications (Table 1).
Postoperative considerations
Following the insertion of an IPP, immediate postoperative care is essential to having a successful surgical outcome. The Henry Mummy Wrap is commonly used to reduce postoperative inflammation and hematoma formation (59). Drain placement can also reduce postoperative pain and hematoma. A study by Tonzi and Shridharani found that drainage following surgery was not significantly altered by surgical approach (60). They also found that drainage was significant for the first 72 hours post-op, supporting the placement of a drain for this duration (60).
Patients should be instructed to wear supportive underwear for the first month after surgery and direct the penis upwards, on the abdomen if possible, to minimize swelling (61). At 2-week follow-up, PD patients are recommended to begin massage and stretch therapy, pulling the pump downward in the scrotum (19). Patients normally begin cycling their prosthetic after 4–6 weeks, but pain may be a limiting factor in this process (61). It is recommended that patients abstain from sexual intercourse for at least 6 weeks following IPP insertion or at least until full healing has occurred (62). Signs and symptoms of infection should be discussed with patients so they know when to inform the doctor or proceed to an emergency department.
Habous et al. performed a study to identify common predictors of patient satisfaction following penile implant (63). The authors found the only major predictor of low satisfaction to be surgical complications, such as infection (63). A proportion of 86.8% of patients with an IPP were satisfied with their procedure, whereas malleable device patients had a lower satisfaction rate of 76% (63). Additionally, there was no correlation between PD and IPP satisfaction rates, indicating that PD patients are just as likely to be satisfied with their device as non-PD patients (63). Another study by Khera et al. supports this finding (64). In their study, they found that of 250 patients treated for PD with IPP, satisfaction rates were more than 80% at 1- and 2-year follow-up (64). This was not significantly different from non-PD satisfaction rates, suggesting that PD has little impact on IPP postoperative satisfaction rates (64). A study by Henry et al. further supported positive outcomes for PD patients with IPP implant (65). In their study, PD patients report higher IIEF total scores and erectile hardness when compared with patients with other comorbidities such as diabetes, cardiovascular disease, and prostatectomy (65). This suggests that other ailments are more likely to cause post-IPP dissatisfaction when compared to PD.
Conclusions
IPP remains the gold standard for PD patients with moderate to severe concomitant ED refractory to standard medical therapy. In men with PD undergoing an IPP, there are multiple different surgical approaches and incisions, as well as adjunct maneuvers and procedures that can be performed to straighten the penis during IPP placement with the goal of a functionally straight erection for penetration. Physician experience and comfort levels, as well as correct patient selection and careful preoperative and postoperative counseling are imperative for a successful operation and patient satisfaction.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Martin Gross, Jay Simhan, and David Barham) for the series “Complex Penile Prosthesis Surgery” published in Translational Andrology and Urology. The article has undergone external peer review.
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-180/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-180/coif). The series “Complex Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. H.L.B. is a consultant to Boston Scientific, Coloplast and BK Ultrasound. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All clinical procedures described in this study were performed in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patients for the publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- Bernie HL. Peyronie’s Disease: Epidemiology, Pathophysiology, Evaluation. AUA Urology Core Curriculum. Updated 2023 Feb.
- Levine LA, Burnett AL. Standard operating procedures for Peyronie's disease. J Sex Med 2013;10:230-44. [Crossref] [PubMed]
- Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease: evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. [Crossref] [PubMed]
- Levine LA, Dimitriou RJ. A surgical algorithm for penile prosthesis placement in men with erectile failure and Peyronie's disease. Int J Impot Res 2000;12:147-51. [Crossref] [PubMed]
- Clavell-Hernández J, Ziegelmann MJ. Peyronie’s Disease: Surgical Management. AUA Urology Core Curriculum. Updated 2023 Feb.
- Chang C, Simhan J. Erectile Dysfunction: Surgical Management. AUA Urology Core Curriculum. Updated 2023 Mar.
- Trost LW, Baum N, Hellstrom WJ. Managing the difficult penile prosthesis patient. J Sex Med 2013;10:893-906; quiz 907. [Crossref] [PubMed]
- Habous M, Tealab A, Farag M, et al. Malleable Penile Implant Is an Effective Therapeutic Option in Men With Peyronie's Disease and Erectile Dysfunction. Sex Med 2018;6:24-9. [Crossref] [PubMed]
- Khera M, Mulcahy J, Wen L, et al. Is there still a place for malleable penile implants in the United States? Wilson's Workshop #18. Int J Impot Res 2023;35:82-9. [Crossref] [PubMed]
- Burns RT, Bernie HL. Frailty in Surgical Patients: Is it Relevant to Sexual Medicine? J Sex Med 2022;19:401-3. [Crossref] [PubMed]
- Ostrowski KA, Gannon JR, Walsh TJ. A review of the epidemiology and treatment of Peyronie's disease. Res Rep Urol 2016;8:61-70. [PubMed]
- Garaffa G, Minervini A, Christopher NA, et al. The management of residual curvature after penile prosthesis implantation in men with Peyronie's disease. BJU Int 2011;108:1152-6. [Crossref] [PubMed]
- Levine LA, Rybak J. Traction therapy for men with shortened penis prior to penile prosthesis implantation: a pilot study. J Sex Med 2011;8:2112-7. [Crossref] [PubMed]
- Canguven O, Talib RA, Campbell J, et al. Is the daily use of vacuum erection device for a month before penile prosthesis implantation beneficial? a randomized controlled trial. Andrology 2017;5:103-6. [Crossref] [PubMed]
- Mulhall J, Ahmed A, Anderson M. Penile prosthetic surgery for Peyronie's disease: defining the need for intraoperative adjuvant maneuvers. J Sex Med 2004;1:318-21. [Crossref] [PubMed]
- Chung E, Solomon M, DeYoung L, et al. Comparison between AMS 700™ CX and Coloplast™ Titan inflatable penile prosthesis for Peyronie's disease treatment and remodeling: clinical outcomes and patient satisfaction. J Sex Med 2013;10:2855-60. [Crossref] [PubMed]
- Anaissie J, Yafi FA. A review of surgical strategies for penile prosthesis implantation in patients with Peyronie's disease. Transl Androl Urol 2016;5:342-50. [Crossref] [PubMed]
- Wilson SK, Delk JR 2nd. A new treatment for Peyronie's disease: modeling the penis over an inflatable penile prosthesis. J Urol 1994;152:1121-3. [Crossref] [PubMed]
- Lucas JW, Gross MS, Barlotta RM, et al. Optimal Modeling: an Updated Method for Safely and Effectively Eliminating Curvature During Penile Prosthesis Implantation. Urology 2020;146:133-9. [Crossref] [PubMed]
- Wilson SK, Cleves MA, Delk JR 2nd. Long-term followup of treatment for Peyronie's disease: modeling the penis over an inflatable penile prosthesis. J Urol 2001;165:825-9. [Crossref] [PubMed]
- Moncada I, Krishnappa P, Ascencios J, et al. Home modeling after penile prosthesis implantation in the management of residual curvature in Peyronie's disease. Int J Impot Res 2021;33:616-9. [Crossref] [PubMed]
- Wilson SK, Carson CC. Surgical straightening with penile prosthesis. In: Levine LA, Tolowa NJ, editors. Peyronie’s Disease. A Guide to Clinical Management. New York: Humana Press, 2007:249-58.
- Krishnappa P, Fernandez-Pascual E, Carballido J, et al. Surgical Management of Peyronie's Disease With Co-Existent Erectile Dysfunction. Sex Med 2019;7:361-70. [Crossref] [PubMed]
- Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. J Urol 1965;93:230-2. [Crossref] [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. [Crossref] [PubMed]
- Cordon BH, Osmonov D, Hatzichristodoulou G, et al. Peyronie's penile plication. Transl Androl Urol 2017;6:639-44. [Crossref] [PubMed]
- Chung PH, Tausch TJ, Simhan J, et al. Dorsal plication without degloving is safe and effective for correcting ventral penile deformities. Urology 2014;84:1228-33. [Crossref] [PubMed]
- Chung PH, Scott JF, Morey AF. High patient satisfaction of inflatable penile prosthesis insertion with synchronous penile plication for erectile dysfunction and Peyronie's disease. J Sex Med 2014;11:1593-8. [Crossref] [PubMed]
- Syed AH, Abbasi Z, Hargreave TB. Nesbit procedure for disabling Peyronie's curvature: a median follow-up of 84 months. Urology 2003;61:999-1003. [Crossref] [PubMed]
- Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft: long-term follow up. J Sex Med 2008;5:2221-8; discussion 2229-30. [Crossref] [PubMed]
- Rahman NU, Carrion RE, Bochinski D, et al. Combined penile plication surgery and insertion of penile prosthesis for severe penile curvature and erectile dysfunction. J Urol 2004;171:2346-9. [Crossref] [PubMed]
- Ziegelmann MJ, Farrell MR, Levine LA. Modern treatment strategies for penile prosthetics in Peyronie's disease: a contemporary clinical review. Asian J Androl 2020;22:51-9. [Crossref] [PubMed]
- Tausch TJ, Chung PH, Siegel JA, et al. Intraoperative Decision-making for Precise Penile Straightening During Inflatable Penile Prosthesis Surgery. Urology 2015;86:1048-52. [Crossref] [PubMed]
- Perito P, Wilson S. The Peyronie’s plaque “scratch”: an adjunct to modeling. J Sex Med 2013;10:1194-7. [Crossref] [PubMed]
- Levine LA, Larsen SM. Surgical correction of persistent Peyronie's disease following collagenase clostridium histolyticum treatment. J Sex Med 2015;12:259-64. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Simultaneous penile lengthening and penile prosthesis implantation in patients with Peyronie's disease, refractory erectile dysfunction, and severe penile shortening. J Sex Med 2012;9:316-21. [Crossref] [PubMed]
- Choi JB, Lee DS. Efficacy of H-shaped incision with bovine pericardial graft in Peyronie's disease: a 1-year follow-up using penile Doppler ultrasonography. Int J Impot Res 2021;33:541-7. Erratum in: Cell Death Dis 2020;11:608 Erratum in: Int J Impot Res 2020;33:667. [Crossref] [PubMed]
- Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical therapy of Peyronie's disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res 2013;25:183-7. [Crossref] [PubMed]
- Fernández-Pascual E, Gonzalez-García FJ, Rodríguez-Monsalve M, et al. Surgical Technique for Complex Cases of Peyronie's Disease With Implantation of Penile Prosthesis, Multiple Corporeal Incisions, and Grafting With Collagen Fleece. J Sex Med 2019;16:323-32. [Crossref] [PubMed]
- Rolle L, Ceruti C, Timpano M, et al. A new, innovative, lengthening surgical procedure for Peyronie's disease by penile prosthesis implantation with double dorsal-ventral patch graft: the "sliding technique". J Sex Med 2012;9:2389-95. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE. Penile lengthening and widening without grafting according to a modified 'sliding' technique. BJU Int 2015;116:965-72. [Crossref] [PubMed]
- Egydio PH, Kuehhas FE. The Multiple-Slit Technique (MUST) for Penile Length and Girth Restoration. J Sex Med 2018;15:261-9. [Crossref] [PubMed]
- Otero JR, Manfredi C, Wilson SK. The good, the bad, and the ugly about surgical approaches for inflatable penile prosthesis implantation. Int J Impot Res 2022;34:128-37. [Crossref] [PubMed]
- Barry JM, Seifert A. Penoscrotal approach for placement of paired penile implants for impotence. J Urol 1979;122:325-6. [Crossref] [PubMed]
- Gupta NK, Ring J, Trost L, et al. The penoscrotal surgical approach for inflatable penile prosthesis placement. Transl Androl Urol 2017;6:628-38. [Crossref] [PubMed]
- Palmisano F, Boeri L, Cristini C, et al. Comparison of Infrapubic vs Penoscrotal Approaches for 3-Piece Inflatable Penile Prosthesis Placement: Do We Have a Winner? Sex Med Rev 2018;6:631-9. [Crossref] [PubMed]
- Henry GD, Mahle P, Caso J, et al. Surgical Techniques in Penoscrotal Implantation of an Inflatable Penile Prosthesis: A Guide to Increasing Patient Satisfaction and Surgeon Ease. Sex Med Rev 2015;3:36-47. [Crossref] [PubMed]
- Houlihan MD, Köhler TS, Wilson SK, et al. Penoscrotal approach for IPP: still up-to-date after more than 40 years? Int J Impot Res 2020;32:2-9. [Crossref] [PubMed]
- Barrett D, Furlow W. Penile prosthesis implantation. In: Segraves R, Schoenberg H, editors. Diagnosis and treatment of erectile disturbances: a guide for clinicians. New York: Plenum Medical Book Co.; 1985:219-4.
- Vollstedt A, Gross MS, Antonini G, et al. The infrapubic surgical approach for inflatable penile prosthesis placement. Transl Androl Urol 2017;6:620-7. [Crossref] [PubMed]
- Antonini G, De Berardinis E, Del Giudice F, et al. Inflatable Penile Prosthesis Placement, Scratch Technique and Postoperative Vacuum Therapy as a Combined Approach to Definitive Treatment of Peyronie's Disease. J Urol 2018;200:642-7. [Crossref] [PubMed]
- Grande P, Antonini G, Cristini C, et al. Penoscrotal versus minimally invasive infrapubic approach for inflatable penile prosthesis placement: a single-center matched-pair analysis. World J Urol 2018;36:1167-74. [Crossref] [PubMed]
- Kramer A, Chason J. Residents at the University of Maryland Medical System provide insight to learning infrapubic approach for IPP surgery: relative benefits but novel challenges exposed in first 15 cases. J Sex Med 2010;7:1298-305. [Crossref] [PubMed]
- Perito PE. Minimally invasive infrapubic inflatable penile implant. J Sex Med 2008;5:27-30. [Crossref] [PubMed]
- Weinberg AC, Pagano MJ, Deibert CM, et al. Sub-Coronal Inflatable Penile Prosthesis Placement With Modified No-Touch Technique: A Step-by-Step Approach With Outcomes. J Sex Med 2016;13:270-6. [Crossref] [PubMed]
- Feng CL, Langbo WA, Anderson LK, et al. Subcoronal inflatable penile prosthesis implantation: indications and outcomes. J Sex Med 2023;20:888-92. [Crossref] [PubMed]
- Henry GD. The Henry mummy wrap and the Henry finger sweep surgical techniques. J Sex Med 2009;6:619-22. [Crossref] [PubMed]
- Wilson SK, Mora-Estaves C, Egydio P, et al. Glans Necrosis Following Penile Prosthesis Implantation: Prevention and Treatment Suggestions. Urology 2017;107:144-8. [Crossref] [PubMed]
- Tonzi M, Shridharani A. Drain volume output following IPP implantation: An analysis by surgical approach. J Sex Med 2022;19:S11-2. [Crossref]
- Levine LA, Becher EF, Bella AJ, et al. Penile Prosthesis Surgery: Current Recommendations From the International Consultation on Sexual Medicine. J Sex Med 2016;13:489-518. [Crossref] [PubMed]
- Egydio PH. Surgical straightening with tunica incision and grafting technique. In Levine LA, Tolowa NJ, editors. Peyronie’s Disease. A Guide to Clinical Management, New York: Humana Press, 2007:227-39.
- Habous M, Tal R, Tealab A, et al. Predictors of Satisfaction in Men After Penile Implant Surgery. J Sex Med 2018;15:1180-6. [Crossref] [PubMed]
- Khera M, Bella A, Karpman E, et al. Penile Prosthesis Implantation in Patients With Peyronie's Disease: Results of the PROPPER Study Demonstrates a Decrease in Patient-Reported Depression. J Sex Med 2018;15:786-8. [Crossref] [PubMed]
- Henry GD, Karpman E, Brant W, et al. The Who, How and What of Real-World Penile Implantation in 2015: The PROPPER Registry Baseline Data. J Urol 2016;195:427-33. [Crossref] [PubMed]


