
Real-world clinical effectiveness of nonsurgical treatments for female with POP-Q stage II cystocele: a retrospective analysis of therapeutic efficacy
Highlight box
Key findings
• Patients with pelvic organ prolapse quantification (POP-Q) stage II cystocele seemed to benefit more from pelvic floor muscle training (PFMT) + pessary treatment, with greater improvement both in quality-of-life scores and the anatomical outcomes. When PFMT combined with radiofrequency (RF), stress urinary incontinence (SUI) was resolved better.
What is known and what is new?
• In general, females with POP-Q stage II cystocele have traditionally been recommended to PFMT.
• In order to achieve better effectiveness, we combined PFMT with pessary or non-ablative RF.
• The combination of 2 treatment strategies seems to be superior to PFMT only.
What is the implication, and what should change now?
• Individualized treatment should be implemented based on the specific situation of the patient.
• It should be noted that although the complete recovery rate of cystocele in the above 3 nonsurgical groups was unlikely, it can still delay the further occurrence or aggravation of prolapse to a certain extent.
• This real-world data may help clinicians to develop a more comprehensive diagnosis and treatment plan.
Introduction
Cystocele is a common urogynecological condition among parous, postmenopausal, and elderly people over 65 years old (1), which refers to the prolapse of 2/3 of the bladder in the vagina and is accompanied by dysuria or urinary incontinence (UI). According to the international evaluation method of pelvic organ prolapse quantification (POP-Q), patients with cystocele of stage II and below are mainly treated conservatively, including pelvic floor muscle training (PFMT), pelvic floor myoelectric stimulation, magnetic stimulation, biofeedback treatment, and so on (2). In addition, pessary (3), non-ablative radiofrequency (RF) technology (4), carbon dioxide laser technology (5), and other technologies are developing rapidly. They are widely used in uterine prolapse and stress urinary incontinence (SUI) (6-8), but there are few reports on the treatment of patients with cystocele. In our pelvic floor disease center, patients with POP-Q stage II cystocele receive PFMT combined with pessary, PFMT and non-ablative RF, or PFMT only. Therefore, the objective of this retrospective study was to evaluate the outcomes of the above treatments in improving the anatomy and function of cystocele over a 1-year period. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-486/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Ethics Committee of the Second Hospital of Tianjin Medical University (No. KY2022K065). The informed consent was waived by the Ethics Committee of the Second Hospital of Tianjin Medical University due to the retrospective nature of this study. This study was registered at Chinese Clinical Trial Registry (registration number ChiCTR2200059780). This was a retrospective study carried out at Tianjin Female Pelvic Floor Dysfunction Treatment Center between January 2020 and January 2022 to present the real-world effectiveness of nonsurgical treatments. All screened and eligible female patients in our center had dominant symptoms of cystocele, and they were determined to have stage II cystocele using the POP-Q system and trans-labial pelvic floor ultrasound (9). Enrolled patients, with or without UI, were respectively assigned to only pelvic floor muscle treatment (PFMT group), PFMT combined with pessaries (PFMT + P group), or PFMT combined with non-ablative radiofrequency (PFMT + RF group). The PFMT group was equivalent to the control group, whereas the other 2 groups received pessary or RF treatment combined with PFMT. The assignment of each patient to a specific treatment type depended on the doctor’s treatment recommendations and personal circumstances. We conducted follow-up examinations after the 3 treatments mentioned above at 3 time points (1, 6, and 12 months).
The exclusion criteria included female patients with uterine prolapse and/or rectocele, POP-Q stage ≥ III or stage I, hysterectomy, previous surgery or intervention of pelvic organ prolapse (POP) or SUI, other physical therapies for pelvic floor disorders other than the above 3; use of vaginal estrogen in the last 6 months; unexplained vaginal bleeding, copper intrauterine device, the presence of any type of cancer; pelvic inflammatory disease, concurrent sexual transmitted disease, and other concomitant illnesses or medications affecting wound healing or sexuality.
The specific implementation of 3 different treatment methods is as follows.
PMFT
Every patient was referred to a pelvic therapist. Treatment commenced with an examination of the function of the pelvic floor using Glazer assessment (Weisi Medical Technology Co., Ltd., Nanjing, China; Biological stimulation feedback instrument, product model: SA9800). Patients who were unable to contract or relax their pelvic floor muscles were firstly instructed on how to do this. They received feedback during digital palpation or, if necessary, by applying myofeedback or electrical stimulation (Weisi Medical Technology Co., Ltd., Nanjing, China; Biological stimulation feedback instrument, product model: SA9800). Participants with an overactive pelvic floor performed relaxation exercise instead of contraction exercises. When they had become able to contract or relax their pelvic floor, they practiced the training through face-to-face consultation and started the exercises at home (3–5 times a week, 2–3 times a day).
PMFT + P management
A specialist gynecologist in our center assessed and inserted a vaginal pessary for the patients in the PFMT + P group. When the following 3 criteria were met, it was determined that the pessary (Aobo Jin Pharmaceutical Technology Co., Ltd., Jiangsu, China; Product Registration Certificate No.: SXZZ No. 20172180766) was the appropriate size: (I) 1 or half single finger space present between the pessary and the vaginal wall after the insertion; (II) the pessary would not slip out during urination, defecation, or physical activities such as walking, coughing, and straining; (III) no discomfort/expulsion/difficulty was experienced during urination or defecation. A successfully fitted vaginal pessary was defined as being able to be retained by the patient without experiencing discomfort after a 2-week period since the implantation. If the pessary slipped out, the patient was offered a reassessment and replacement with another pessary. It was considered unsuccessful if the gynecologist was unable to provide an adequately fitting pessary after at least 3 attempts, or if the patient did not plan to use the pessary after fitting. Patients returned to our center for cleaning and maintenance of the pessary every month. Patients were also asked perform pelvic floor muscles exercises at home (3–5 times a week, 2–3 times each day).
PMFT + RF technology
Non-ablative RF can generate electromagnetic wave currents with thermal effects, which can mediate the acute inflammatory process and promote the formation of new collagen and elastin (10). A Likert scale was used to measure the stage of satisfaction with the treatment. Patients began receiving RF therapy when the muscle strength increased to a certain level through PFMT. The RF (Wuhan Banbiantian Medical Technology Development Co., Ltd., China; Vaginal radiofrequency therapy device, Electrode model: BBT-MS402) was a monopolar configuration, including 2 electrodes: 1 was the intracavity electrode placed in the vagina, which needed to be placed with a non-lubricated condom and water-soluble gel, and the other was the scattered electrode located in the lumbosacral region. The RF worked in the form of capacitive electrical transmission. During clinical procedures, the temperature was set at 45 ℃, with a frequency of 300 kHz to 1 MHz. The patient was placed in the lithotomy position, and the physiotherapist repeated semicircular movements in the vagina to maintain the temperature at 45 ℃. The movements were repeated on the whole vaginal wall. Patients in the RF group received 3–5 vaginal treatments using the RF device at 4-week intervals (11). The 4-week period between applications allowed adequate healing of the vaginal tissues that had been subjected to RF. The procedures were performed by an experienced urogynecologist. Patients were also asked perform pelvic floor muscles exercises at home (3–5 times a week, 2–3 times each day).
Follow-up
The number of cases in the center during the study period determined the sample size. Follow-up time points were scheduled at 1, 6, and 12 months after the treatments (baseline). Follow-up included Pelvic Floor Distress Inventory-20 questionnaire (PFDI-20), Persian version urinary incontinence quality of life questionnaire (I-QOL), and an examination of the pelvic floor muscle function by Glazer assessment at 4 time points. POP-Q measurement (point Ba) and bladder neck-symphyseal distance (BSD) were assessed using ultrasound at 12 months. Patients in the PFMT + P group removed their pessary by themselves (or with the assistance of their gynecologist) at least 48 hours before re-assessments. For the questionnaires, the calculation method was questionnaire scores at each time point after treatment minus baseline scores, respectively. In the POP-Q measurement, we considered a Ba point rise of ≥1 cm compared to baseline as improvement, and a drop of ≥1 cm as deterioration. Data collectors and analysts were blinded to the grouping situation. The main potential influencing factors on the experimental results were type of treatment received and the quality of completion of the treatment by the patients. Therefore, a specialized physiotherapist or urogynecologist provided professional guidance and correction to the patient before each treatment, and then conducted monthly supervision.
Statistical analysis
Our primary outcome was to assess whether the deltas (i.e., relative differences between follow-up and baseline calculated per patient) were statistically different among the 3 groups, which were used to control for confounding factors among groups. Individuals with missing data or loss to follow up were excluded. Data were analyzed using SPSS 19.0 (IBM Corp, Chicago, IL, USA). Mean score difference between groups was analyzed by t-tests; one-way analysis of variance (ANOVA) was used to assess the differences of ΔPFDI-20, ΔI-QOL, ΔBSD at rest, ΔBSD on max value, and pelvic floor electromyography evaluation between multiple groups. A P value <0.05 was considered statistically significant. Point Ba improvement was compared using chi-squared test or Fisher’s exact test. Statistical tests were 2-sided, with a 5% significance level.
Results
Participants and descriptive statistics
Considering the inclusion criteria, exclusion criteria, and follow-up requirements, there were 277 patients with stage II cystocele who visited our center between January 2020 and January 2022. A total of 147 patients were ultimately included and completed the planned treatments and follow-up (Figure 1). The main reasons for exclusion were that the participant did not complete the corresponding treatment as required or did not submit the questionnaires. Firstly, we summarized the baseline characteristics of the enrolled patients (Table 1). Among the 147 patients, 30 patients were successfully fitted with a pessary; the mean age of wearing formal pessary was 56.25±14.87 years; 22 of the patients were fitted with ring pessaries with support, 8 were fitted with Gellhorn pessaries; 27 patients received PFMT and RF, with the mean age of 34.07±4.94 years; 90 patients received PFMT, with the mean age of 40.13±11.59 years. A total of 87 patients experienced mild to moderate UI. All of the point Ba in the POP-Q system of patients were ≥0 in the PFMT + P group. There were no important adverse events or unintended effects in each study condition.
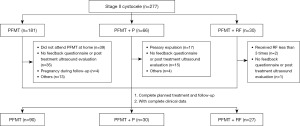
Table 1
| Characteristics | PFMT (n=90) | PFMT + P (n=30) | PFMT + RF (n=27) | F | P value | ||
|---|---|---|---|---|---|---|---|
| PFMT vs. PFMT + P | PFMT vs. PFMT + RF | PFMT + P vs. PFMT + RF | |||||
| Age (years) | 40.13±11.59 | 56.25±14.87 | 34.07±4.94 | 7.733 | 0.039 | 0.267 | 0.008 |
| BMI (kg/m2) | 23.68±5.37 | 25.72±3.82 | 22.58±2.91 | 0.447 | 0.533 | 0.808 | 0.395 |
| No. of vaginal deliveries (times) | 2.15±2.86 | 3.51±2.47 | 1.10±0.98 | 5.109 | 0.042 | 0.736 | 0.026 |
| History of urinary incontinence | 50 (55.56) | 17 (56.67) | 20 (74.07) | – | Pearson P=0.238 | ||
| Postmenopausal | 38 (42.22) | 28 (93.33) | 0 | – | Fisher P=0.000 | ||
| Chronic cough | 4 (4.44) | 3 (10.00) | 2 (7.41) | – | Fisher P=0.487 | ||
| Constipation | 8 (8.88) | 5 (16.67) | 2 (7.41) | – | Fisher P=0.468 | ||
| Ba (POP-Q) (cm) | −0.75±2.94 | 0.86±1.87 | 0.17±3.06 | 9.115 | 0.006 | 0.374 | 0.021 |
| PFDI-20 | 59.81±33.7 | 66.25±28.35 | 62.34±17.83 | 0.039 | 0.812 | 0.825 | 0.987 |
| I-QOL | 61.27±21.32 | 56.65±14.39 | 59.57±19.27 | 0.082 | 0.725 | 0.753 | 0.970 |
Data are shown as mean ± standard deviation or n (%). BMI, body mass index; PFMT, pelvic floor muscle training; PFMT + P, PFMT combined with pessary; PFMT + RF, PFMT combined with non-ablative radiofrequency; POP-Q, pelvic organ prolapse quantification; Ba, point Ba in the POP-Q measurement; PFDI-20, Pelvic Floor Distress Inventory-20 questionnaire; I-QOL, Persian version urinary incontinence quality of life questionnaire.
Questionnaire scores
Questionnaire baseline and follow-up scores are summarized in Table 2. The pelvic floor symptoms were improved in 3 groups, as can be seen by decreased scores in PFDI-20 from baseline to follow-up times. In the PDFI-20 questionnaire, there was no difference in the scores’ evolution at 3 time points among the 3 groups (P>0.05). Inter-group comparison revealed that the PFMT + P group showed more significant improvement compared to the other 2 groups at 6 and 12 months (P<0.05). However, no difference was found in pairwise comparison between the PFMT and PFMT + RF groups (P>0.05). A similar trend was revealed via comparison of the evolution of I-QOL scores in PFMT + RF group with the other 2 groups.
Table 2
| Variables | PFMT | PFMT + P | PFMT + RF | F | P values | ||
|---|---|---|---|---|---|---|---|
| PFMT vs. PFMT + P | PFMT vs. PFMT + RF | PFMT + P vs. PFMT + RF | |||||
| ΔPFDI-20 | |||||||
| 1 month | 8.31±1.99 | 9.56±2.26 | 10.29±11.27 | ||||
| 6 months | 5.73±6.91 | 14.28±8.57 | 7.43±8.41 | 5.831 | 0.002 | 0.548 | 0.019 |
| 12 months | 1.68±5.87 | 9.78±8.25 | 4.71±6.67 | 6.253 | 0.001 | 0.225 | 0.048 |
| ΔI-QOL | |||||||
| 1 month | 10.43±13.49 | 5.13±24.45 | 6.83±25.00 | ||||
| 6 months | 7.77±10.47 | 3.82±23.43 | 22.81±16.69 | 4.541 | 0.574 | 0.040 | 0.006 |
| 12 months | 5.35±8.02 | 3.47±22.06 | 19.73±18.04 | 3.752 | 0.782 | 0.043 | 0.015 |
Data are presented as mean ± standard deviation. PFMT, pelvic floor muscle training; PFMT + P, PFMT combined with pessary; PFMT + RF, PFMT combined with non-ablative radiofrequency; PFDI-20, Pelvic Floor Distress Inventory-20 questionnaire; I-QOL, Persian version urinary incontinence quality of life questionnaire.
Physical examination and ultrasound
At the 12-month post-treatment follow-up, there was difference among the groups in terms of stage improvement of cystocele (point Ba). Meanwhile, the proportion of patients with improvement (Ba point rose by ≥1 cm) in the PFMT + P group was also better than in the other 2 groups (Table 3).
Table 3
| ΔBa | PFMT (n=90) | PFMT + P (n=30) | PFMT + RF (n=27) | P value§ |
|---|---|---|---|---|
| Improvement† | 14 (15.6%) | 13 (43.3%) | 7 (25.9%) | 0.03 |
| The same | 62 (68.9%) | 13 (43.3%) | 18 (66.7%) | |
| Deterioration‡ | 14 (15.6%) | 4 (13.3%) | 2 (7.4%) |
†, improvement ≥1 cm POP-Q stage; ‡, deterioration ≥1 cm POP-Q stage; §, Chi-square test, Fisher exact test, 2-sided. POP-Q, pelvic organ prolapse quantification; Ba, point Ba in the POP-Q measurement; PFMT, pelvic floor muscle training; PFMT + P, PFMT combined with pessary; PFMT + RF, PFMT combined with non-ablative radiofrequency.
Similar to the Ba change in physical examination, patients who accepted PFMT + P achieved better improvement of BSD on maximum Valsalva maneuver at 12 months after treatment (Table 4).
Table 4
| Variables | PFMT (n=15) | PFMT + P (n=7) | PFMT + RF (n=6) | F | P values | ||
|---|---|---|---|---|---|---|---|
| PFMT vs. PFMT + P | PFMT vs. PFMT + RF | PFMT + P vs. PFMT + RF | |||||
| ΔBSD at rest | −1.98±4.79 | 1.56±6.60 | 2.70±3.11 | ||||
| ΔBSD on max value | −7.54±7.31 | −28.27±28.90 | −5.03±13.27 | 4.596 | 0.010 | 0.753 | 0.017 |
Data are presented as mean ± standard deviation. BSD, bladder neck-symphyseal distance; PFMT, pelvic floor muscle training; PFMT + P, PFMT combined with pessary; PFMT + RF, PFMT combined with non-ablative radiofrequency.
Pelvic floor muscle function
Pelvic floor muscle function was examined by Glazer assessment before the treatment and at 1, 6, and 12 months after treatment. Among the 3 treatment groups, at 1, 6, and 12 months, the maximum values of rapid contraction in the PMFT group and PMFT + P group were significantly higher than the baseline values before treatment (P<0.05). In the PMFT + RF group, the maximum values of rapid contraction were significantly higher than the baseline values before treatment, but there was no significant statistical difference (P>0.05). Among the 3 treatment groups, the maximum value of rapid contraction showed a gradually decreasing trend with the passage of treatment time (Figure 2A).
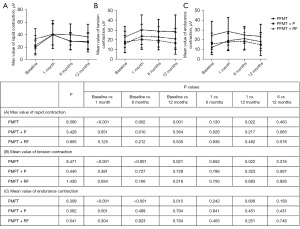
At the follow-up time points after the treatments, the mean values of tension contraction and endurance contraction showed the same trend of change in the 3 groups. In the PMFT group, the mean values of tension contraction and endurance contraction were significantly increased compared to the baseline values before treatment (P<0.05). In the PMFT + P group and PMFT + RF group, there was no statistical difference (P>0.05) in the mean values of tension contraction and endurance contraction compared to the baseline values before treatment. Among the 3 treatment groups, the average value of tension contraction and endurance contraction decreased slightly with the passage of treatment time, but there was no statistical difference (P>0.05) (Figure 2B,2C).
Discussion
Cystocele is a chronic disease which has been defined as bladder descent into the vagina, even beyond the level of the hymen (12). If it is left unchecked, affected patients will experience negative impacts on their well-being, psychological, and sexual life with the progression of the condition (13). The main causes of cystocele include weakened levator ani structure, excessive stretching of pelvic fascia, and defect of the endopelvic fascia, among others (14). Most patients will not experience symptoms until the protrusion exceeds the hymen opening. It has been confirmed that the regression of stage I prolapse is not uncommon, therefore, it is appropriate to observe and closely follow-up the mild asymptomatic cases. Broadly, physical therapy has represented the main treatment strategy for management of the stage II cystocele to slow down disease progression. Conservative management mainly includes 2 types: PFMT and vaginal pessaries (12). PFMT enhances pelvic floor support by strengthening the systemic contraction of levator ani muscles. Currently, the International Consultation on Incontinence has listed short-term PFMT as an A-level recommendation (15). However, how to better improve cystocele and UI symptoms on the basis of PFMT and maintain the long-term effects remains to be clarified. We combined pessary or RF with PFMT. All treatment options were offered to the participants and thoroughly discussed before the treatments.
This may be the first study to compare the clinical effects of PFMT, pessary, and non-ablative RF on improving the anatomy and function of female stage II cystocele.
We measured therapeutic efficacy both by quality-of-life scores and the anatomical outcome including POP-Q assessment and trans-labial ultrasound. The Ba point and BSD were respectively used at 12 months after treatment to evaluate the improvement of cystocele. In terms of improving the effective rate of cystocele, the PFMT + P group (43.3%) was significantly better than the other 2 groups (15.6% and 25.9%); for most patients, half or more of the above 3 groups maintained their original prolapse state (Ba point remained roughly unchanged); only a small number of patients experienced further exacerbation of prolapse. From the corresponding ultrasound indicators, we found that the improvement of ΔBSD in the PFMT + P group was more obvious, which was consistent with the improvement trend of POP in physical examination, and also reflects the consistency of 2 detection methods for evaluating the stage of prolapse (Ba point in POP-Q system and numerical description of BSD in ultrasound examination) (16). Compared with other reported figures (17-20), prolapse-specific symptoms reduced significantly in the patients of the PFMT + P group, measured by the PFDI-20 at 6 and 12 months, which may be related to the direct improvement of cystocele and restoration of bladder urination function by the uterine support from the perspective of physical support.
In the PFMT + RF group, this study showed the benefit of PFMT + RF in stage II cystocele patients with SUI, by significantly improving the I-QOL of patients via long-term use than PFMT only or combined pessary. Cystocele was a result of weakness at the pubic-bladder cervical fascia and levator ani muscle complex. The pathophysiology of SUI is similar to that of cystocele, both of which are caused by weak pelvic floor support structures. In fact, SUI is often present in patients with cystocele. Its onset is mainly due to reduced support from the pelvic floor and the vaginal connective tissue around the bladder neck and urethra (21). Abdelaziz et al. reported that bipolar RF was more efficacious than monopolar RF and the effect after 6 months of treatment was worse than at 3 months (22). In our study, the effect could be sustained until 12 months after treatment, possibly due to the use of monopolar RF combined with PFMT and an increase in treatment frequency. It is considered that the body will increase the support of connective tissue by promoting the regeneration of fibrin and elastin for some time after RF treatment.
PFMT helps patients to improve their pelvic floor muscle strength, endurance, power, relaxation, or a combination of these parameters by developing structured and personalized exercise plans (23). PFMT can be assisted by vaginal cones and electrical muscle stimulation, and so on. Meanwhile, it can achieve synchronous recovery of type I and type II muscle fibers (24), which were accurately identified by Glazer assessment. Although the function of type I and type II muscle was improved significantly in the PFMT group compared to that of the other 2 groups, the clinical relevance of the small difference was doubtful. There are, however, several possible explanations for this difference. Patients in the PFMT + P group were mainly middle aged and elderly patients and with Ba ≥0 who were sometimes concerned that PFMT may affect the pessary and then failed to perform PFMT as required. PFMT can effectively enhance the type I muscle function and should be persisted with for a long time. Pessary and RF were found to have little effect on enhancing the contraction force of muscle fibers. They mainly play a physical support and fascia regeneration role in the treatment of cystocele, rather than playing a role by enhancing pelvic floor muscle strength (25,26). In fact, the results in this study showed that the 3 treatments improve cystocele through different mechanisms; this discrepancy prompts further exploration into the underlying mechanisms and factors influencing these distinct treatment outcomes, and it will be beneficial for the clinical significance or potential consequences of patient outcomes and treatment strategies.
Similar to other retrospective studies, the limitation of this study is its ability to produce causality and control for all possible confounding factors. Of course, we will also further extend the observation period to monitor the duration of the effectiveness of each treatment. In addition, the expression ability of the patients is also an important factor affecting the results. Therefore, we need to conduct further validation in prospective randomized controlled trials.
Conclusions
Patients with POP-Q stage II cystocele in the PFMT + P group seemed to benefit more than those in the other 2 groups, with greater improvement both in quality-of-life scores and the anatomical outcomes. When PFMT is combined with RF, SUI can be resolved better. Individualized treatment should be taken based on the specific situation of the patient. In addition, it should be noted that although the complete recovery rate of cystocele in the above 3 groups was unlikely, it can still delay the further occurrence or aggravation of prolapse to a certain extent. Moreover, the combination of 2 treatment strategies seems to be superior to PFMT only.
Acknowledgments
We would like to acknowledge Ms. Hongmei Wang, Ms. Dongchao Shan and Ms. Haisu Yu for their contributions to this study.
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-486/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-486/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-486/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-486/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Medical Ethics Committee of the Second Hospital of Tianjin Medical University (No. KY2022K065). The informed consent was waived by the Ethics Committee of the Second Hospital of Tianjin Medical University due to the retrospective nature of this study. This study was registered at Chinese Clinical Trial Registry (registration number ChiCTR2200059780).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kalis V, Kovarova V, Rusavy Z, et al. Trans-obturator cystocele repair of level 2 paravaginal defect. Int Urogynecol J 2020;31:2435-8. [Crossref] [PubMed]
- Bø K, Anglès-Acedo S, Batra A, et al. International urogynecology consultation chapter 3 committee 2; conservative treatment of patient with pelvic organ prolapse: Pelvic floor muscle training. Int Urogynecol J 2022;33:2633-67. [Crossref] [PubMed]
- Coolen AWM, Troost S, Mol BWJ, et al. Primary treatment of pelvic organ prolapse: pessary use versus prolapse surgery. Int Urogynecol J 2018;29:99-107. [Crossref] [PubMed]
- Robinson D, Flint R, Veit-Rubin N, et al. Is there enough evidence to justify the use of laser and other thermal therapies in female lower urinary tract dysfunction? Report from the ICI-RS 2019. Neurourol Urodyn 2020;39:S140-7. [Crossref] [PubMed]
- Bhide AA, Khullar V, Swift S, et al. The use of laser in urogynaecology. Int Urogynecol J 2019;30:683-92. [Crossref] [PubMed]
- Naumann G. Quo Vadis Urogynecology 2020 - Innovative Treatment Concepts for Urinary Incontinence and Pelvic Organ Prolapse. Geburtshilfe Frauenheilkd 2021;81:183-90. [Crossref] [PubMed]
- Hu JS, Pierre EF. Urinary Incontinence in Women: Evaluation and Management. Am Fam Physician 2019;100:339-48. [PubMed]
- Kolumbán S, Kovács K, Majoros A, et al. Conservative and surgical treatments performed for symptomatic pelvic organ prolapse and stress urinary incontinence in Hungary. Orv Hetil 2022;163:2072-8. [PubMed]
- Vereeck S, Pacquée S, Jacquemyn Y, et al. Does Cystocele Type Vary Between Vaginally Parous and Nulliparous Women? J Ultrasound Med 2023;42:809-13. [Crossref] [PubMed]
- Liu JF, Shen W, Huang D, et al. Expert consensus of Chinese Association for the Study of Pain on the radiofrequency therapy technology in the Department of Pain. World J Clin Cases 2021;9:2123-35. [Crossref] [PubMed]
- Kolodchenko Y. Nonablative, Noncoagulative Multipolar Radiofrequency and Pulsed Electromagnetic Field Treatment Improves Vaginal Laxity and Sexual Function. Womens Health Rep (New Rochelle) 2021;2:285-94. [Crossref] [PubMed]
- Makajeva J, Watters C, Safioleas P. Cystocele. Treasure Island (FL): StatPearls Publishing; 2024.
- Aboseif C, Liu P. Pelvic Organ Prolapse. Treasure Island (FL): StatPearls Publishing; 2024.
- Song C, Wen W, Pan L, et al. Analysis of the anatomical and biomechanical characteristics of the pelvic floor in cystocele. Acta Obstet Gynecol Scand 2023;102:1661-73. [Crossref] [PubMed]
- Huang YC, Chang KV. Kegel Exercises. Treasure Island (FL): StatPearls Publishing; 2024.
- Xu H, Wu W, Wang X, et al. A predictive model of choosing pessary type for women with symptomatic pelvic organ prolapse. Menopause 2021;28:1279-86. [Crossref] [PubMed]
- Aimjirakul K, Pumtako M, Manonai J. Quality of Life After Treatment for Pelvic Organ Prolapse: Vaginal Pessary versus Surgery. Int J Womens Health 2023;15:1017-25. [Crossref] [PubMed]
- Limbutara W, Bunyavejchevin S, Ruanphoo P, et al. Patient-reported goal achievements after pelvic floor muscle training versus pessary in women with pelvic organ prolapse. A randomised controlled trial. J Obstet Gynaecol 2023;43:2181061. [Crossref] [PubMed]
- Mao M, Ai F, Kang J, et al. Successful long-term use of Gellhorn pessary and the effect on symptoms and quality of life in women with symptomatic pelvic organ prolapse. Menopause 2019;26:145-51. [Crossref] [PubMed]
- Pizzoferrato AC, Thuillier C, Vénara A, et al. Management of female pelvic organ prolapse-Summary of the 2021 HAS guidelines. J Gynecol Obstet Hum Reprod 2023;52:102535. [Crossref] [PubMed]
- Wu YM, Welk B. Revisiting current treatment options for stress urinary incontinence and pelvic organ prolapse: a contemporary literature review. Res Rep Urol 2019;11:179-88. [Crossref] [PubMed]
- Abdelaziz A, Dell J, Karram M. Transvaginal radiofrequency energy for the treatment of urinary stress incontinence: A comparison of monopolar and bipolar technologies in both pre- and post-menopausal patients. Neurourol Urodyn 2021;40:1804-10. [Crossref] [PubMed]
- Espiño-Albela A, Castaño-García C, Díaz-Mohedo E, et al. Effects of Pelvic-Floor Muscle Training in Patients with Pelvic Organ Prolapse Approached with Surgery vs. Conservative Treatment: A Systematic Review. J Pers Med 2022;12:806. [Crossref] [PubMed]
- Zhu H, Zhang D, Gao L, et al. Effect of Pelvic Floor Workout on Pelvic Floor Muscle Function Recovery of Postpartum Women: Protocol for a Randomized Controlled Trial. Int J Environ Res Public Health 2022;19:11073. [Crossref] [PubMed]
- Kiefner B, Schwab F, Kuppinger M, et al. Evaluating compliance and applicability of postpartum pessary use for preventing and treating pelvic floor dysfunction: a prospective multicenter study. Arch Gynecol Obstet 2023;308:651-9. [Crossref] [PubMed]
- Fu L, Long S, Li Q, et al. The efficacy and safety of temperature controlled dual-mode radiofrequency in women with vaginal laxity. BMC Womens Health 2023;23:121. [Crossref] [PubMed]
(English Language Editor: J. Jones)


