
Penile prosthesis in priapism: a systematic review of outcomes and complications
Highlight box
Key findings
• Penile prosthesis (PP) emerges as a promising therapeutic avenue for treating priapism, particularly in cases of ischemic priapism with a duration exceeding 36 hours or recurrent priapism resistant to medical interventions.
What is known and what is new?
• Priapism is an infrequent condition characterized by persistent penile erection lasting over 4 hours without sexual stimulation, leading to significant morbidity and complications, such as erectile dysfunction and penile fibrosis. The surgical management of priapism presents considerable challenges. Our comprehensive review aims to assess the role of PP implantation in the treatment of priapism.
What is the implication, and what should change now?
• The existing evidence on this subject is of very low quality, underscoring the need for larger, well-designed studies to investigate priapism-related PP implantation thoroughly. Such studies should evaluate long-term outcomes, patients’ satisfaction, and complications as primary endpoints.
Introduction
Priapism is a persistent erection of the penis in the absence of sexual stimulation that lasts greater than 4 hours. It is a rare condition with an estimated incidence rate of 1–1.5 cases per 100,000 people (1). Priapism is classified into three types: ischemic, non-ischemic, and recurrent ischemic. Priapism is associated with significant morbidity and complications, including erectile dysfunction and penile fibrosis, and often requires prompt medical and/or surgical intervention (2).
For cases of ischemic, low-flow, or veno-occlusive priapism that fail conservative treatment and shunt procedures, immediate insertion of a penile prosthesis (PP) may be the best option to preserve erectile function and prevent penile shortening due to corporal fibrosis (3). Per the American Urologic Association (AUA), immediate PP implantation is recommended for priapism episodes that last more than 36 hours and is considered the first-line treatment in ischemic priapism lasting more than 72 hours (4).
Non-ischemic, arterial, or high-flow priapism is an erection caused by unregulated cavernous arterial inflow, which does not cause rigidity or pain, and emergency treatment is typically unnecessary (5). However, long-term exposure to high oxygen levels can cause corporal fibrosis and result in erectile dysfunction. Despite the potential benefits of non-ischemic priapism in preventing fibrosis and erectile dysfunction in the short term, patients with this subtype of priapism may still require PP implantation as a last resort, typically after unsuccessful selective embolization (6).
Recurrent, stuttering, or intermittent priapism is characterized by recurrent, painful, prolonged erections that resolve spontaneously and generally last less than ischemic priapism. Medical management has demonstrated efficacy in decreasing the frequency and duration of episodes; however, in cases of medically refractory recurrent priapism, PP implantation is considered to mitigate the risk of future ischemic episodes; however, such occurrences are infrequent (7).
The surgical management of priapism presents considerable challenges influenced by various factors. Of particular significance is the scarcity of published literature concerning the optimal timing for PP implantation in priapism cases. Immediate implantation is considered to have a greater risk of infection compared to delayed implantation (8). Nevertheless, a consensus on the precise timeline distinguishing immediate, early, and delayed implantation remains elusive. Discrepancies arise from various studies, where delayed implantation is defined as occurring beyond 3 weeks, 3 months, or 4 months following the initial onset of priapism (9-11). Consequently, comparing outcomes and complication rates across these studies becomes challenging due to the substantial variations in the defined timelines. According to multiple urologic guidelines, implantation is only recommended when other less invasive treatments, like phosphodiesterase inhibitors and intracavernosal injections, have proven ineffective in treating priapism (12,13). We herein provide a systematic review that aims to evaluate PP in the management of priapism. Specifically, we will provide a descriptive, comprehensive review assessing the long-term complications, outcomes, and satisfaction rate of patients who receive PP following an episode of priapism. We present this article in accordance with the PRISMA reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-23-224/rc).
Methods
A systematic literature search in the databases PubMed, Embase, and Scopus was performed. The search terms used were “priapism” AND (“penile prosthesis” OR “penile implant” OR “penile prostheses” OR “penile prosthesis implantation” OR “penile prosthesis implantations”). All the studies in the English language and published up to 2022 were included for evaluation.
The PRISMA statement was followed. Criteria for the exclusion of the studies were: case report studies, number of patients <5 cases, expert opinions, comments, letters to the editor, non-English language, experimental studies in animals, papers that only describe techniques, and studies in population with no priapism previously to the PP implantation. Two reviewers independently screened each record.
The measured outcomes included satisfaction rate, sexual intercourse achievement, and penile length. The reasons for exclusion are presented in the flow diagram (Figure 1). Regarding the quality of the studies, all the included papers were rated based on the GRADE system.

Results
A total of 717 English-language studies were collected of which 17 were selected for this review from 2002 to 2022. The reasons for exclusion are described in Figure 1. According to the GRADE system, the included studies have a very low quality of evidence.
The outcomes of penile prostheses implantation are summarized in Table 1. Most of the studies describe the outcomes of an early PP implant; however, Durazi et al. describe the results in a delayed approach to PP implant, and some of the papers do not specify the time when the prosthesis was implanted (early or delayed) (9-12,14). Of these selected papers, five compare the outcomes of early placement (EP) vs. delayed placement (DP) PP implants after priapism (8-11,26).
Table 1
| Author, year | N and age (years) | Surgical technique | Etiology priapism | PP device | Operative time | Follow-up | Intraoperative complications | Post-operative complications | Outcomes |
|---|---|---|---|---|---|---|---|---|---|
| Salman, 2023 (8) | N: 42; EP: 23; DP: 19 | EP: <1 week | SC anemia [6]; drugs [15]; idiopathic [17]; other [4] | AMS spectra implant or TUBE malleable implant | N/R | EP: 11±5.5 months | EP: N/R | Distal erosion (P<0.005): EP [2]; DP: [0] | Implant length: EP: 22±1 cm; DP: 20.7±1 cm |
| Age: EP: 55±9.5; DP: 54±13 | DP: ≥3 months | DP: 15±4.5 months | DP: corporal perforation [7] | Infection: EP [4]; DP [2] | Implant girth: EP: 11±0.5 mm; DP: 10±0.7 mm | ||||
| Penile edema (P<0.005): EP [6]; DP [0] | |||||||||
| Johnson, 2019 (9) | N: 126; EP: 88; DP: 38 | EP: <3 weeks; MPP [83]; IPP [5] | N/R | N/R | N/R | EP: median 17.8 [3–76] months | N/R | EP: infection [7]; curvature [1]; erosion [1] | EP: >90% achieved sexual intercourse; >90% satisfaction rate |
| Age: N/R | DP: >3 weeks; MPP [19]; IPP [19] | DP: median 18.6 [3–28] months | DP: infection [9]; erosion [2]; mechanical failure [1] | DP: 86.8% achieved sexual intercourse; 60.5% satisfaction rate | |||||
| Zacharakis, 2014 (10) | N: EP: 68; DP: 27 | EP: MPP [64]; IPP [4] | SC anemia [39]; medication [27]; idiopathic [29] | N/R | N/R | EP: median 17 [15–24] months | N/R | EP: infection [5]; curvature [1] | EP: easier dilation; satisfaction rate >90% |
| Age: EP: mean 42 [26–63]; DP: mean 45 [28–69] | DP: MPP [12]; IPP [15] | DP: median 21 [20–24] months | DP: infection [5]; erosion [1]; mechanical failure [1] | DP: satisfaction rate 60% | |||||
| Penile shortening: EP: 3%; DP: 40% | P<0.001 | ||||||||
| P<0.001 | |||||||||
| Elhawy, 2021 (11) | N: 72 | MPP [2] | Medication [38]; idiopathic: 34 | Genesis, coloplast | N/R | Median 43 [38–64] months | N/R | Glans edema: EP [3]; DP [1] | EP: median girth 11 mm; median hospital length 3 days |
| Age: 41.2±17.4 | EP [8] | Wound infection: EP [4]; DP [3] | DP: girth median 9.5 mm; median hospital length 1 day | ||||||
| DP [16] | Post-operative pain: EP [3]; DP [1] | ||||||||
| Distal fibrosis: EP [0]; DP [1] | |||||||||
| P>0.05 | |||||||||
| Durazi, 2008 (14) | N: 17 | DP: MPP [11]; two-piece IPP [4]; three-piece IPP [2] | SC anemia [16]; medication [1] | MPP (AMS 650) | N/R | Median 6 [2–9] years | Urethral injury [2] | Penile edema [4]; superficial hematoma [3] | 100% satisfaction rate; penile length median 16 [14–20] cm |
| Age: median 22 [18–28] | Two-piece (Ambicor) | ||||||||
| Three-piece (700CX) | |||||||||
| Ralph, 2009 (15) | N: 50 | EP: MPP [43], three-piece IPP [7] | SC [5]; medication [18]; Idiopathic [24]; other [3] | MPP: Genesis and Acuform; Coloplast; AMS 650 | N/R | Median 15.7 [4–60] months | N/R | Infection [3]; distal erosion [3]; short rods distal [2]; auto-inflation [1] | 96% satisfaction rate; no patient complained of penile shortening |
| Age: mean 46 [25–73] | IPP: AMS CX 700 | ||||||||
| Zacharakis, 2015 (16) | N: 10 | Early insertion MPP | N/R | MPP (Coloplast Genesis) | N/R | Median 13.5 [3–24] months | N/R | Pump malfunction [1]; mild curvature [1] | 80% satisfaction rate after MPP, and 90% after IPP; exchange with upsizing of cylinders by a median of 1 cm in either one or both corporal bodies (range, 0–3 cm) |
| Age: mean 41.3 [26–58] | Posterior exchange to IPP | IPP (AMS 700 or Coloplast Titan) | |||||||
| Razzaghi, 2010 (17) | N: 14 | Early MPP | N/R | N/R | N/R | Median 13.9 [11–38] months | N/R | N/R | 100% satisfaction rate; 64.2% achieved sexual intercourse; no penile shortening |
| Age: mean 44 [29–55] | |||||||||
| Nic an Ríogh, 2019 (18) | N: 6 | Early insertion: MPP | Drugs [5]; malignancy [1] | N/R | N/R | N/R | N/R | N/R | 100% achieved sexual intercourse |
| Age: 37–63 | |||||||||
| Rees, 2002 (19) | N: 8 | Early implant: MPP [6]; IPP [2] | SC [1]; medication [4]; idiopathic [3] | MPP Acuform | N/R | Mean 17 [5–35] months | N/R | Penile deformity due to fibrosis [1] | 100% satisfaction rate and achieved sexual intercourse; no penile shortening |
| Age: mean 41 [27–58] | IPP AMS 700CX | ||||||||
| Salem, 2010 (20) | N: 12 | Early MPP | SC anemia [1]; medication [7]; idiopathic [4] | N/R | N/R | Median 15 [6–36] months | Proximal corpora perforation [1] | N/R | 100% achieved sexual intercourse |
| Age: N/R | |||||||||
| Uberoi, 2011 (21) | N: 8 | Three-pieces IPP [7]; MPP [1] | SC anemia [2]; medication [3]; idiopathic [3] | N/R | Mean 85 min | 2–57 months | N/R | N/R | 87.5% satisfaction rate |
| Age: mean 35.9 [18–52] | |||||||||
| Vagnoni, 2019 (22) | N: 6 | Early implant soft-silicone PP | SC [2]; idiopathic [4] | Soft-silicone PP Virilis ITM | Median 82 [62–180] min | Median 9 [3–17] months | N/R | Transient reduction of penile sensitivity | 100% satisfaction rate; no significant loss of penile length or penile curvature |
| Age: mean 41 [18–47] | |||||||||
| Sedigh, 2011 (23) | N: 5 | Early insertion: IPP [4]; MPP [1] | N/R | Coloplast Titan OTR [1] | 94±31.3 min | N/R | Penile hematoma [5] | Initial reduced penile sensibility [5]; no infection or erosion | IIEF-5: Q5 mean value 4; 100% achieved sexual intercourse; No penile shortening |
| Age: median 56 [33–73] | AMS 700 LGX [1] | ||||||||
| AMS 700 CX [1] | |||||||||
| AMS (MPP) | |||||||||
| Baumgarten, 2018 (24) | N: 18 | MPP [16]; IPP [2] | N/R | N/R | N/R | Mean 4.8 [1–36] months | N/R | Infection [4] | 83% satisfaction rate |
| Age: mean 43.9 [0–62] | |||||||||
| Bella, 2012 (25) | N: 7 | N/R | N/R | N/R | N/R | N/R | N/R | N/R | EHS: 4 at 6 months; IIEF-5 increased over 17 points (mean) from the baseline |
| Age: N/R | |||||||||
| Hawksworth, 2019 (26) | N: 19; EP: 2; DP: 17 | EP [2] | N/R | N/R | N/R | N/R | N/R | EP: 1 infection with PP removal | 7 answered EDITS questions: 6 were satisfied (85.7%) |
| Age: mean 41 [21–86] | DP [17] |
A comprehensive overview of studies focusing on PP implantation post-priapism. The table lists key study details including author and year, sample size (n), surgical technique timing, etiology of priapism, type of PP device used, operative time, follow-up duration, intraoperative and postoperative complications, and overall patient outcomes. Data are presented as mean ± SD, [number], mean [range], or median [range]. N, number; PP, penile prosthesis; EP, early placement; DP, delayed placement; SC, sickle cell; N/R, not reported; MPP, malleable penile prosthesis; IPP, inflatable penile prosthesis; EHS, erection hardness score; EDITS, erectile dysfunction inventory of treatment satisfaction; SD, standard deviation.
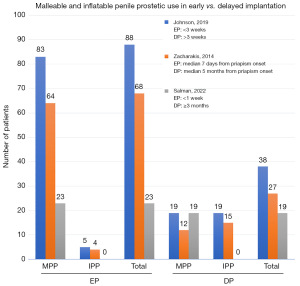
Various researchers’ approaches to EP of penile implants are elucidated. Johnson [2019] conducted a study with a sample size (n) of 126 participants and defined the EP group as comprising 70% of the total patients, wherein surgery took place within 3 weeks of the priapism incident (9). Conversely, Elhawy [2021] investigated 24 individuals receiving malleable PP (MPP), accounting for 33% of the cohort, and considered EP to entail implantation after 72 hours, with a median implantation time of 7 days (11). Additionally, in a study conducted by Zacharakis [2014] with a sample size of 68 participants (n=68; 100%), EP was defined similarly to Elhawy’s approach (10,11). Finally, Salman [2023] undertook research with a sample size of 42 participants, accounting for 55% of the total, and classified EP as implantation during the first week following the occurrence of priapism (8). Figure 2 shows the frequency of MPP and inflatable PP (IPP) in the EP or DP settings, as described by Johnson, Zacharakis, and Salman (8-10).
The most common causes of priapism described in all papers are sickle cell anemia (SCA), the use of medication (primarily injectable drugs, to achieve an erection), and idiopathic. Nic an Ríogh [2019] described one case of priapism due to malignancy. Overall studies show a higher satisfaction rate ranging between 80% and 100% compared to baseline, with sexual intercourse achievement ranging between 64.2% and 100% (9,14-20).
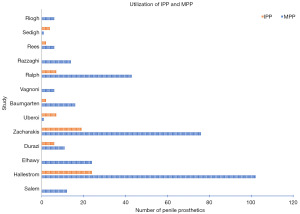
Most of the patients had a MPP implant either early or delayed after the priapism episode, Figure 3 shows the relation between the number of IPP and MPP in the different papers. Only two studies used a higher number of IPP compared to MPP—Uberoi et al. of a series of eight patients, seven had a three-piece IPP implant, and only one had an MPP (8,14-16,21,22) and Sedigh et al. had only one MPP implant vs. four IPP (23). Zacharakis et al. [2015] describe a series of 10 patients with early MPP implant after priapism with later exchange to IPP (16). This protocol showed upsizing of cylinders by a median of 1 cm in both corporal bodies (range 0–3 cm), and two complications (one pump malfunction, and mild curvature) (16).
The majority of studies examining the occurrence of penile shortening after priapism have not found evidence to support this phenomenon (15,17,19,22,23). However, Zacharakis [2014] reported this complication in his series, and it was observed more frequently in patients who underwent DP implants compared to those who received early implants (40% vs. 3%, P<0.001) (10).
Elhawy et al. compared the median girths between patients who underwent EP insertion and those who received DP insertion. The median bending for the EP group was 11 mm, while for the DP group, it was 9.5 mm (11). The study also examined the occurrence of complications in these groups. Although the EP group had a higher number of gland edema, wound infection, and post-operative pain, the DP group had a higher incidence of distal fibrosis. However, none of these differences were statistically significant.
The most frequently reported complications following PP procedures include infection (range, 6–50%), erosion (range, 1–9%), curvature (range, 1–10%), and mechanical issues with the device, such as malfunction or auto-inflation (range, 2–5%) (8-11,14-16,19,24,27). Sedigh [2011] and Vagnoni [2019] found that all patients initially experienced a decrease in penile sensitivity, but this was a temporary side effect (22,23).
The majority of studies did not employ validated questionnaires to assess sexual function outcomes and only relied on descriptions of patient satisfaction, reported as percentages (range, 60–100%) (9-11,14-17,21-24). However, Bella et al. used the IIEF-5 to evaluate patients and demonstrated a significant increase of over 17 points (mean) from the baseline in sexual function after the penile implant post-priapism event (25).
Discussion
Priapism is a rare but potentially serious condition that causes prolonged and painful erections. It is typically classified into three types, ischemic, non-ischemic, and recurrent with the former being the most common form. Initial management of ischemic priapism typically involves aspiration and irrigation of the corpora cavernosa with sympathomimetic agents. However, if this fails, invasive treatments such shunts and surgical interventions may be necessary. Implantation of a PP is the most effective treatment for post-priapism erectile dysfunction. It can be performed in an immediate or delayed fashion with an IPP or MPP. In this review, we aimed to evaluate the characteristics of patients who underwent PP insertion for the treatment of refractory ischemic priapism.
Placing a PP during the delayed setting may pose a significant challenge due to the presence of widespread fibrosis in the corpora. Expanding the corpora requiring extended corporotomies and the use of special tools increases the likelihood of complications such as distal/proximal crossover, perforation, or urethral injury. Additionally, the procedure’s duration significantly increases the risk of postoperative infection compared to first-time implants (28).
The patient-reported satisfaction rates were observed to be more favorable among individuals who underwent IPP insertion, ranging from 80% to 100%, compared to those who received MPP with satisfaction rates ranging from 60.5% to 100%. However, it is noteworthy that several studies lacked a standardized approach in assessing patient satisfaction rates (9-11,14-16,21-24,27). Furthermore, as extensively documented in the literature, patients with priapism face a heightened risk of infection, erosion, and contracture in comparison to individuals with no prior history of erectile dysfunction (28). Penile deformity is a known complication with IPP insertion in the acute setting and has been postulated to be from contracture of the corporal scarring on a deflated cylinder (28,29). In the delayed setting, patient satisfaction was lower and presented the surgeon with a higher degree of operative difficulty given the fibrosis and scarring that occurs over time. Furthermore, fibrosis tends to cause some degree of penile shortening, and patients may still experience a loss of length after implantation, which is one of the most reported reasons for dissatisfaction among men with a PP. Given the low patient satisfaction rates, it has been recommended to perform PP implantation in the acute setting (26,27,29,30). It should be noted that no studies reviewed were powered to demonstrate a superiority of immediate vs. delayed implantation, and thus any conclusion is merely based on available published evidence.
While the available evidence suggests that PP insertion is a safe and effective option for managing priapism, there are some limitations to consider. Firstly, these procedures are invasive and may carry risks such as infection, device malfunction, and erosion. Additionally, the long-term effects of these devices on sexual function and patient satisfaction are not well understood. Further research is needed to better understand the optimal patient selection, device selection, and postoperative care protocols for IPP and MPP insertion in the management of priapism.
Conclusions
The purpose of this review is to evaluate the characteristics and outcomes of patients undergoing treatment for ischemic priapism with insertion of a PP. Studies specifically looking at delayed vs. immediate implantation of PP are limited. Also, to date there are no trials comparing IPP vs. MPP insertion for ischemic priapism. Until more data is available, clinical management of ischemic priapism with prosthesis insertion should be approached as a shared decision-making process. Counseling should include the increased risk of infection and erosion in these patients as well as concern for penile shortening in the delayed setting.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Martin Gross, Jay Simhan, and David Barham) for the series “Complex Penile Prosthesis Surgery” published in Translational Andrology and Urology. The article has undergone external peer review.
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-23-224/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-23-224/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-23-224/coif). The series “Complex Penile Prosthesis Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Stein DM, Flum AS, Cashy J, et al. Nationwide emergency department visits for priapism in the United States. J Sex Med 2013;10:2418-22. [Crossref] [PubMed]
- Cherian J, Rao AR, Thwaini A, et al. Medical and surgical management of priapism. Postgrad Med J 2006;82:89-94. [Crossref] [PubMed]
- Muneer A. Insertion of Penile Implants in Patients with Priapism: When Is the Right Time? Eur Urol Focus 2023;9:49-50. [Crossref] [PubMed]
- Bivalacqua TJ, Allen BK, Brock G, et al. Acute Ischemic Priapism: An AUA/SMSNA Guideline. J Urol 2021;206:1114-21. [Crossref] [PubMed]
- Muneer A, Alnajjar HM, Ralph D. Recent advances in the management of priapism. F1000Res 2018;7:37. [Crossref] [PubMed]
- Yücel ÖB, Pazır Y, Kadıoğlu A. Penile Prosthesis Implantation in Priapism. Sex Med Rev 2018;6:310-8. [Crossref] [PubMed]
- Johnson MJ, McNeillis V, Chiriaco G, et al. Rare Disorders of Painful Erection: A Cohort Study of the Investigation and Management of Stuttering Priapism and Sleep-Related Painful Erection. J Sex Med 2021;18:376-84. [Crossref] [PubMed]
- Salman B, Elsherif E, Elgharabawy M, et al. Early versus delayed penile prosthesis insertion for refractory ischemic priapism. Arab J Urol 2022;21:76-81. [Crossref] [PubMed]
- Johnson M, Hallerstrom M, Chiriaco G, et al. PD44-01 a comparison between early and delayed penile prosthesis insertion in men with refractory ischaemic priapism. J Urol 2019;201:e821. [Crossref]
- Zacharakis E, Garaffa G, Raheem AA, et al. Penile prosthesis insertion in patients with refractory ischaemic priapism: early vs delayed implantation. BJU Int 2014;114:576-81. [Crossref] [PubMed]
- Elhawy MM, Fawzy AM. Outcomes of low-flow priapism and role of integrated penile prosthesis management. Afr J Urol 2021;27:1-8. [Crossref]
- Barham DW, Chang C, Hammad M, et al. Delayed placement of an inflatable penile prosthesis is associated with a high complication rate in men with a history of ischemic priapism. J Sex Med 2023;20:1052-6. [Crossref] [PubMed]
- Medina-Polo J, García-Gómez B, Alonso-Isa M, et al. Clinical guidelines on erectile dysfunction surgery: EAU-AUA perspectives. Actas Urol Esp (Engl Ed) 2020;44:289-93. [Crossref] [PubMed]
- Durazi MH, Jalal AA. Penile prosthesis implantation for treatment of postpriapism erectile dysfunction. Urol J 2008;5:115-9. [PubMed]
- Ralph DJ, Garaffa G, Muneer A, et al. The immediate insertion of a penile prosthesis for acute ischaemic priapism. Eur Urol 2009;56:1033-8. [Crossref] [PubMed]
- Zacharakis E, Deluca F, Raheem A, et al. Does Early Insertion of a Malleable Prosthesis Still Allow Later Upsizing of Cylinders in Patients with Ischemic Priapism? J Sex Med 2015;12:190.
- Razzaghi MR, Rezaei A, Javanmard B, et al. S105 the immediate insertion of a penile prosthesis for prolonged ischemic priapism. Eur Urol Suppl 2010;6:584. [Crossref]
- Nic an Ríogh AU, Breen K, Mohan P. Immediate penile prosthesis for the management of ischemic priapism. Eur Urol Suppl 2019;18:e2527. [Crossref]
- Rees RW, Kalsi J, Minhas S, et al. The management of low-flow priapism with the immediate insertion of a penile prosthesis. BJU Int 2002;90:893-7. [Crossref] [PubMed]
- Salem EA, El Aasser O. Management of ischemic priapism by penile prosthesis insertion: prevention of distal erosion. J Urol 2010;183:2300-3. [Crossref] [PubMed]
- Uberoi V, Munarriz R. Penile Prosthesis Placement in Patients with Erectile Dysfunction and Corporal Fibrosis after Priapism: Outcomes, Satisfaction and Complications. J Sex Med 2011;8:26.
- Vagnoni V, Franceschelli A, Gentile G, et al. PS-07-015 Soft-silicone penile prosthesis implant in the management of delayed or refractory ischemic priapism. J Sex Med 2019;16:S25. [Crossref]
- Sedigh O, Rolle L, Negro CL, et al. Early insertion of inflatable prosthesis for intractable ischemic priapism: our experience and review of the literature. Int J Impot Res 2011;23:158-64. [Crossref] [PubMed]
- Baumgarten A, Shah B, Binner M, et al. PD18-10 Penile Prosthesis Placement in the Setting of Prolonged Refractory Ischemic Priapism: A Single Institution Experience. J Urol 2018;199:e393. [Crossref]
- Bella AJ, Wang R, Shamloul R, et al. 3-Piece Inflatable Penile Prosthesis Insertion Post Distal t-Shunt for Priapism with Dilation/Corporal Snake Maneuver and Comparison to Post al-Ghorab Shunt IPP Outcomes. J Sex Med 2012;9:236.
- Hawksworth DJ, Koomson AB, Burnett AL. Satisfaction with inflatable penile prosthesis in patients with history of ischemic priapism. Eur Urol Suppl 2019;18:e1617. [Crossref]
- Ridgley J, Raison N, Sheikh MI, et al. Ischaemic priapism: A clinical review. Turk J Urol 2017;43:1-8. [Crossref] [PubMed]
- Mishra K, Loeb A, Bukavina L, et al. Management of Priapism: A Contemporary Review. Sex Med Rev 2020;8:131-9. [Crossref] [PubMed]
- Chung PH, Scott JF, Morey AF. High patient satisfaction of inflatable penile prosthesis insertion with synchronous penile plication for erectile dysfunction and Peyronie's disease. J Sex Med 2014;11:1593-8. [Crossref] [PubMed]
- Scherzer ND, Dick B, Gabrielson AT, et al. Penile Prosthesis Complications: Planning, Prevention, and Decision Making. Sex Med Rev 2019;7:349-59. [Crossref] [PubMed]


