
Construction of early warning classification of risk in bladder spasm and its intervention plans guided by the rate adjustment card of continuous bladder irrigation after transurethral resection of the prostate (TURP): development and usability study
Highlight box
Key findings
• By combining a speed regulation card of continuous bladder irrigation (CBI) after transurethral resection of the prostate (TURP), literature retrieval and semi-structured interviews, together with specific clinical situations, and after two rounds of expert consultation, a comprehensive management plan for bladder spasm in patients with CBI was developed.
What is known and what is new?
• It is important to closely observe the color of drainage fluid during CBI, which as it may reflect real-time postoperative bleeding. When the color of the drainage fluid is abnormal, effective measures should be undertaken. In existing studies, scholars have formulated CBI programs in an attempt to quantify the relationship between the color of drainage fluid and irrigation speed, but have yet to incorporate bladder spasm prevention and control levels or design corresponding graded nursing intervention programs according to different drainage fluid colors.
• In this study, the early warning classification of bladder spasm related to CBI and a corresponding intervention plan was established. A hierarchical management of patients with CBI was developed.
What is the implication, and what should change now?
• In this study, the developed TURP CBI speed adjusting card was used to construct the early warning grade of bladder spasm related to CBI. The corresponding intervention plan using the Delphi method combined with clinical context, was utilized to create a hierarchical management of patients with CBI.
IntroductionOther Section
Benign prostatic hyperplasia (BPH) is the most common benign disease causing urinary dysfunction in middle-aged and elderly men (1,2). The “gold standard” of its surgical treatment is transurethral resection of the prostate (TURP) (3). Compared with traditional open surgery, TURP has the advantages of less trauma and faster recovery (4). This surgery integrates endoscopy and electroresection. However, due to the rich blood supply and extensive vasculature of the prostate tissue, the bleeding from local veins and capillaries cannot always be completely stopped, and significant bleeding may still occur in the short term after the surgery (5). For this reason, continuous bladder irrigation (CBI) is routinely given for 3–5 days post-surgery. However, this method can easily induce bladder spasm, with the incidence rate ranging from 11.11% to 28.57% (6). Bladder spasm not only brings physical and mental pain to patients and delays their postoperative recovery process, but also increases the medical financial burden (7). Therefore, it is important to actively take measures to effectively identify early warning signs and respond to bladder spasm. The color of the drainage fluid should be closely observed during CBI, as it can reflect real-time postoperative bleeding. When the color of the drainage fluid appears abnormal, effective countermeasures must be taken promptly. Among current studies (8,9), researchers have formulated CBI plans from the perspective of quantifying the relationship between drainage fluid color and irrigation rate. They have not yet classified prevention and control levels of bladder spasm based on different colors of drainage fluid or designed corresponding graded nursing intervention plans. Graded nursing intervention involves the division of patients according to different possible changes in their conditions, and then adopting the targeted nursing intervention (10). This study applied the developed CBI rate adjustment card after TURP, and combined the Delphi method with clinical scenarios to construct an early warning classification and corresponding intervention plans for bladder spasm associated with CBI so as to achieve graded management of patients with CBI.
MethodsOther Section
Build a research team
This team included 1 doctor, 2 masters students, and 6 undergraduates. The specific responsibilities were as follows: 1 deputy director from the nursing department was mainly responsible for project guidance and quality monitoring; 1 evidence-based qualified nurse and 1 doctor each took charge of reviewing literature and organizing information; 2 urology specialist nurses were responsible for semi-structured interviews; 2 head nurses were responsible for the selection and determination of correspondence experts; 2 postgraduate students were in charge of issuing and collecting questionnaires, and conducting data input. Members of the research team jointly created the first draft of the plan and conducted integration and data analysis of the collected information and consultation opinions. The study conformed to the provisions of the Declaration of Helsinki (as revised in 2013), and was approved by the Institutional Review Board of the First Affiliated Hospital of Soochow University [approval number: (2021)441]. Informed consent was obtained from all participants in this study.
Construct initial plans
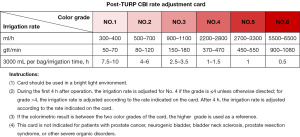
CBI rate adjustment card after TURP surgery
The CBI rate adjustment card after TURP consisted of 3 modules (6) (see Figure 1). Among them, the color scale module of CBI drainage fluid contained 6 color scales from light to dark, which was commonly seen in clinical practice; the CBI rate module contained 6 color scales in accordance with the irrigation rate; the instruction module included colorimetric methods and rate adjustment methods of the rate adjustment card, as well as contraindication groups. This rate adjustment card not only comprehensively defined the relationship between each color scale of CBI drainage fluid and the irrigation rate, but also further quantified the adjustment measurement unit of irrigation rate corresponding to each color scale. In the process of constructing the plan, we supplemented the warning grading standards of risk in bladder spasm though a scale module of CBI drainage fluid, analyzed the influencing factors of bladder spasm in patients with CBI in a comprehensive and multi-dimensional manner, and provided corresponding suggestions and countermeasures. We analyzed the early warning of risk in bladder spasm from the perspective of the color of drainage fluid, and proposed targeted nursing intervention plans.
Literature search
Computerized decision-making systems, guideline websites, professional association websites, evidence-based databases, and comprehensive databases were searched. The search time ranged from the establishment of the database to 31 December 2022. Search terms included “continuous bladder irrigation/CBI”, “prevention of bladder spasm/control of bladder spasm/intervention of bladder spasm/nursing of bladder spasm”, “therapy, management, prevention, nursing, care”. The literature inclusion criteria were as follows: (I) the research participants were patients aged ≥18 years who underwent CBI after BPH surgery; (II) research involved risk warning classification and intervention for CBI complicated by bladder spasm; (III) research types included best clinical practices and guidelines, clinical decision-making, evidence summary, expert consensus, systematic review, meta-analysis, randomized controlled trial, cohort study and cross-sectional study, and so on; (IV) the research language was English. The exclusion criteria were as follows: (I) literature where relevant information could not be extracted or could not be obtained completely; (II) duplicate articles.
After a detailed literature search, 372 relevant articles were initially obtained. Independent screening was conducted by 2 researchers according to the above literature inclusion and exclusion criteria. Finally, 367 articles were excluded and 5 English-language articles were included. Through in-depth reading, the current situation of bladder spasm in patients who underwent CBI after BPH surgery and related nursing research progress was identified. While considering actual clinical nursing issues, we also referred to the current nursing management methods, optimized the construction process of the plans, and added nursing measures accordingly.
Semi-structured interviews
On the basis of literature research and clinical practice experience, we conducted semi-structured interviews with urological medical staff who were using the CBI rate adjustment card mentioned in this study after TURP. The interview outline was as follows: (I) what do you think should be paid attention to in the prevention and control of bladder spasm after TURP? (II) If the early warning classification of risk in bladder spasm and its intervention plans are constructed based on the CBI rate adjustment card after TURP, based on your experience, how should the early warning classification be divided and how should the intervention plans be improved? (III) What are your opinions and suggestions on the nursing measures for bladder spasm prevention and control mentioned in current literature?
Among the 23 urological medical staff included in the semi-structured interviews, 17 were nurses and 6 were doctors. The interviews lasted 35.87±14.42 minutes, the total recording time was 825 minutes, and 169,100 words were transcribed. Through listening to and discussing the factors related to bladder spasm during CBI, we found that when the color of the patient’s drainage fluid fell into different color scales of the CBI rate adjustment card after TURP, the patient’s bladder spasm symptoms would change significantly. Based on this characteristic, we summarized the safe area (color scale No. 1 and 2), warning area (color scale No. 3 and 4), and dangerous area (color scale No. 5 and 6) and supplemented relevant nursing measures by comparing the changed nodes and combining with the previous research basis (6).
Formulate the first draft of plans
Through exploring the early warning classification of risk in bladder spasm and its intervention plans guided by the CBI rate adjustment card after TURP in the above various forms, we initially formulated plans including 3-level risk early warning classification standards and 20 nursing measures.
Expert correspondence inquiry
Form questionnaire of correspondence inquiry
We created a letter questionnaire about early warning classification of risk in bladder spasm and its intervention plans guided by the CBI rate adjustment card after TURP based on the first draft of plans. The questionnaire consisted of 3 parts: (I) the preface of the questionnaire included the research purpose, research content, and instructions for filling out the form; (II) for the main body of the questionnaire, experts were expected to evaluate the importance of the grading standards and corresponding intervention measures according to the Likert 5-point scoring method, assigning values with 1 to 5 points representing unimportant to very important respectively; a supplementary column was also set up; (III) the expert information survey form included a basic information survey form, judgment basis survey form, familiarity survey form, and so on.
Determine selection criteria
Consider the familiarity of medical staff with CBI after TURP. The inclusion criteria for correspondence inquiry experts were as follows: (I) experts who have been engaged in urology medical or nursing work for 10 years or more in a tertiary-level comprehensive hospital; (II) master degree or above in the medical field, bachelor degree or above in the nursing field; (III) those in the medical field have deputy senior professional titles and above, and those in the nursing field have intermediate professional titles and above; (IV) actively participate in and support consulting assignments.
Implement expert correspondence inquiry
We distributed questionnaires face-to-face, checked and accepted them in a timely manner and provided feedback to experts. After collecting the first round of questionnaires, the research team collated, analyzed, and discussed the experts’ opinions, revised and supplemented the items, and formed the second round of questionnaires and issued them again. After 2 rounds of correspondence inquiries, the experts’ opinions were unanimous, and the correspondence inquiry was concluded. The interval between 2 rounds of expert correspondence was 3 to 4 weeks.
Statistical methods
Excel 2013 (Microsoft, Redmond, Washington, USA) and SPSS 27.0 (IBM Corp., Armonk, NY, USA) software were used to enter data and conduct statistical analysis. Frequency, composition ratio, mean, and standard deviation were used to describe the general information of experts; the effective questionnaire recovery rate was used to indicate the activity of experts; the familiarity coefficient was used to indicate the familiarity of experts, the judgment coefficient was used to indicate the basis for experts’ judgment of the research content, and the authority coefficient was used to indicate the degree of expert authority. Kendall’s harmony coefficient and coefficient of variation were used to express the consistency of expert opinions. A P value <0.05 was considered as a statistically significant difference.
ResultsOther Section
General information of correspondence inquiry experts
The 28 experts in this study came from Jiangsu, Sichuan and Shanghai. Among them, 5 (17.9%) were male and 23 (82.1%) were female; age was 33–60 (43.04±5.61) years; working experience was 10–32 (21.07±6.64) years; 6 (21.4%) had a master’s degree or above, 22 (78.6%) had a bachelor’s degree; 17 (60.7%) had deputy senior professional titles or above, and 11 (39.3%) had intermediate professional titles; 23 (82.1%) in clinical nursing, 5 (17.9%) in clinical medicine.
Results of experts’ correspondence inquiry
The level of experts’ activity and authority
The effective questionnaire recovery rates for the 2 rounds of expert correspondence inquiry were both 100%, indicating that the experts were highly motivated for this study. The expert familiarity coefficients of the 2 rounds of correspondence inquiry were both 0.986, the expert judgment coefficients were both 0.917, and the expert authority coefficients were both 0.952, indicating the experts had a high degree of authority and the results were reliable.
Degree of coordination of expert opinions
In the first round of expert correspondence inquiry, the importance score of each indicator was 4.357–5.000 points, the coefficient of variation was 0.000–0.168, the Kendall harmony coefficient was 0.238, the χ2 value was 126.517, P<0.001, and the difference was statistically significant. In the second round of expert correspondence inquiry, the importance score of each indicator was 4.679–5.000 points, the coefficient of variation was 0.000–0.154, the Kendall harmony coefficient was 0.326, the χ2 value was 187.625, P<0.001, and the difference was statistically significant. All this showed that the experts’ opinions basically reached a consensus and the degree of coordination was good.
Experts’ revision opinions
In the first round of expert correspondence inquiry, 17 (60.7%) experts put forward 19 constructive opinions, based on the standard of index importance mean >4.0 points and coefficient of variation <0.25 (11). We made the following adjustments to the relevant content after group discussion and consideration of expert opinions: (I) in the basis of bladder spasm risk warning classification, “within 4 hours after surgery, when the color scale is less than or equal to 4, refer to the alert area intervention measures” was added; (II) the time for squeezing the drainage tube was changed from “every hour” to “every half hour” into the treatment measures in the warning area; (III) “Massage Hegu (LI4), Sanyinjiao (SP6), Zusanli (ST36), Yanglingquan (GB34), and other acupoints” were added into the nursing measures in the warning area and the dangerous area; (IV) “Avoiding urinary tract infections” was added into nursing measures in both warning and dangerous areas; (V) “Routine blood coagulation and D-dimer examinations” were added into the nursing measures in dangerous areas. After the second round of consultation, the experts’ opinions gradually became unified that they only recommended modifying the physical appearance of the nursing care reference tool (see Table 1 and Figure 2).
Table 1
| Levels | Treatment/care measures | Importance score (point) | Coefficient of variation | Full score rate (%) |
|---|---|---|---|---|
| Safe zone (No. 1 & 2 color scale) | 1. Observe bladder irrigation every 2 hours | 5.00 | 0 | 100 |
| 2. Encourage turning over in bed and moving limbs | 5.00 | 0 | 100 | |
| 3. Fill the air bag with 20 mL of water | 4.75±0.52† | 0.11 | 82.14 | |
| 4. Assess the need for bladder irrigation | 5.00 | 0 | 100 | |
| Warning zone (No. 3 & 4 color scale) | 1. Observe bladder irrigation every hour and evaluate symptoms of bladder spasm | 5.00 | 0 | 100 |
| 2. Reduce activities and help turn over every 2 hours | 5.00 | 0 | 100 | |
| 3. Squeeze the drainage tube every half hour | 4.86±0.45† | 0.09 | 92.86 | |
| 4. Fill the air bag with 30 mL of water | 5.00 | 0 | 100 | |
| 5. Report to the bed doctor to clarify the inducements and eliminate related factors | 5.00 | 0 | 100 | |
| 6. Provide health guidance related to bladder spasm | 5.00 | 0 | 100 | |
| 7. Massage Hegu, Sanyinjiao, Zusanli and other acupoints, and apply hot compress to the lower abdomen | 4.75±0.65† | 0.14 | 89.29 | |
| 8. Avoid urinary tract infections | 5.00 | 0 | 100 | |
| Dangerous zone (No. 5 & 6 color scale) | 1. Closely observe bladder irrigation, evaluate bladder spasm symptoms, and monitor vital signs | 5.00 | 0 | 100 |
| 2. Brake, assess the pulse of the dorsalis pedis artery, and prevent venous thrombosis | 5.00 | 0 | 100 | |
| 3. Fill the air bag with 30 mL of water | 5.00 | 0 | 100 | |
| 4. Report to the bed doctor and superior nurse to clarify the inducements and eliminate related factors | 5.00 | 0 | 100 | |
| 5. Provide health guidance related to bladder spasm and strengthen psychological care | 5.00 | 0 | 100 | |
| 6. Squeeze the drainage tube as needed. If the tube is blocked, irrigate it with positive pressure. If it is ineffective, replace the tube | 4.89±0.31† | 0.06 | 92.86 | |
| 7. Massage Hegu, Sanyinjiao, Zusanli and other acupoints, apply heat to the lower abdomen, and use painkillers correctly according to the doctor’s instructions | 4.96±0.19† | 0.04 | 96.43 | |
| 8. Avoid urinary tract infections | 5.00 | 0 | 100 | |
| 9. Fix the external urethral opening with gauze and apply gentle traction for 6 hours, and use hemostatic drugs correctly according to the doctor’s instructions | 5.00 | 0 | 100 | |
| 10. Keep the irrigation fluid temperature close to 35–37 ℃ | 4.68±0.72† | 0.15 | 82.14 | |
| 11. Electrolytes, blood routine, blood coagulation routine, and D-dimer examination | 4.96±0.19† | 0.04 | 96.43 |
†, data are presented as mean ± standard deviation. CBI, continuous bladder irrigation; TURP, transurethral resection of the prostate.

DiscussionOther Section
Scientific analysis of early warning classification of risk in bladder spasm and its intervention plans guided by CBI rate adjustment card after TURP
Based on the CBI rate adjustment after TURP, we formulated an initial draft of early warning classification of risk in bladder spasm and its intervention plans by adopting methods of literature search and semi-structured interviews. This study better ensured the completeness, accuracy, and high quality of the content compared with the method of traditional literature review, and further adopted the Delphi method to verify the scientific nature of the plans. In this study, a total of 28 experts in related fields from 3 China representative regions were consulted by correspondence inquiry. The experts all had more than 10 years of work experience and rich clinical practice background. All of them had a bachelor’s degree or above, of which 60.7% had senior professional titles. All this showed that the experts had a profound foundation in theoretical knowledge, thereby ensuring their authority and reliability. The recovery rate of effective questionnaires of the 2 rounds of expert correspondence inquiry was 100%, indicating that the experts were highly motivated to participate; the expert authority coefficient of the 2 rounds of correspondence inquiry was 0.952, indicating the credibility of the research results. After 2 rounds of correspondence inquiry, the coefficients of variation of each indicator in this study were all <0.25, and the Kendall harmony coefficients were 0.238 and 0.126, both P<0.001, indicating that when evaluating indicators, the opinions of experts were highly consistent and the results obtained had high reliability; finally, a 3-level risk warning classification standard for CBI complicated by bladder spasm and 23 nursing intervention measures were formed. Based on symptomatic treatment, this study determined the suggestions and treatments for each drainage fluid color scale, and presented them in a quantitative manner to better provide guidance for clinical practice.
Necessity analysis of early warning classification of risk in bladder spasm and its intervention plans guided by CBI rate adjustment card after TURP
During the CBI treatment after TURP, it is crucial for medical staff to observe the color of the patient’s drainage fluid. The clinical practice guidelines of the Chinese Association of Urological Surgeons (12) highlight that medical staff should fully understand the importance of early warning of bladder spasm complications, establish applicable systems and tools to scientifically assess, judge, and predict bladder spasm associated with CBI after TURP. The graded nursing intervention was implemented to divide patients according to different possible changes in their conditions, and then conduct grading of nursing resources and grading of nursing interventions for different levels (10). A study has pointed out (13) that accurate and appropriate assessment of patient’s condition and timely and effective graded nursing measures were of great significance in improving patient outcomes. Such intervention methods could rationally and optimally allocate nursing resources, reduce nursing workload, improve the risk awareness and sense of responsibility of nursing staff, and effectively prevent and reduce the occurrence of complications. The warning classification of risk in bladder spasm guided by CBI rate adjustment card after TURP constructed in this study took the color of drainage fluid in clinical patients as the main evaluation criterion in detail, and performed grading according to the specific time after surgery and the color of drainage fluid, thereby assisting nursing staff in comprehensively assessing and grading patients in nursing practice with an objective and standardized manner. By constructing the treatment plan, medical staff could carry out targeted intervention for patients based on the assessment results. This not only improved the accuracy of nursing staff’s assessment and treatment for patients’ bladder spasm, but also prevented medical staff from blindly taking various measures after the color of the drainage fluid changed. This plan could more specifically prevent and control bladder spasm during CBI after TURP, effectively improve the quality of care, and promote early recovery of patients.
Content analysis of early warning classification of risk in bladder spasm and its intervention plans guided by CBI rate adjustment card after TURP
By searching the literature, 3 grading standards for bladder spasm in patients with CBI were initially formulated. In the first round of expert correspondence inquiry, 5 nursing measures were added. There were 6 experts suggesting adding “within 4 hours after surgery, when the color comparison is ≤ No. 4 color scale, refer to the warning zone intervention measures” into the early warning classification basis of bladder spasm risk. Experts emphasized that in clinical practice, even if the color scale was No. 1 or No. 2, nursing intervention should still be carried out according to color scale No. 4 immediately after TURP. Relevant measures should be taken according to the color of the drainage fluid 4–6 hours after surgery (6); 3 experts suggested changing the time for squeezing the drainage tube from “every hour” to “every half hour” in the treatment measures in the warning area to reduce the factor of bladder spasm due to drainage tube blockage (14); 2 experts suggested adding Traditional Chinese Medicine acupoint massage to pain management (15), which was revised to “massage Hegu, Sanyinjiao, Zusanli, Yanglingquan, and other acupoints” eventually; 4 experts suggested adding measures to prevent and control urinary tract infections in warning zones and dangerous zones; in order to consider infections caused by urine leakage and blood oozing caused by bladder spasm, 3 experts suggested that the patient’s objective indicators should be used to evaluate the coagulation function and thrombosis in the nursing measures of risk area, and “blood coagulation routine and D-dimer examination” should be added (16). The second round of expert correspondence inquiry only proposed modifications to the physical appearance of the nursing measure reference tool, without adding or subtracting nursing measures.
ConclusionsOther Section
Based on CBI rate adjustment card after TURP, this study initially established the standards of early warning classification and corresponding nursing measures for bladder spasm guided by CBI through methods of literature search and semi-structured interviews, and combination with specific clinical situations. After 2 rounds of expert correspondence inquiry, comprehensive management plans for bladder spasm in patients with CBI were finally formed. The research team will subsequently conduct a multi-center randomized controlled study to verify the effectiveness of the plans and provide more comprehensive and reliable high-level evidence-based medical basis for CBI care after TURP.
AcknowledgmentsOther Section
Funding: This work was supported by
FootnoteOther Section
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-150/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-150/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-150/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013), and was approved by the Institutional Review Board of the First Affiliated Hospital of Soochow University [approval number: (2021)441]. Informed consent was obtained from all participants in this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
ReferencesOther Section
- Wei J, Zhang S, Wang B, et al. A multicenter retrospective study of transurethral prostate split for benign prostate hyperplasia. Transl Androl Urol 2022;11:213-227. [Crossref] [PubMed]
- Feng Y, Wu J, Zhu H, et al. Three-dimensional measurement and analysis of benign prostatic hyperplasia. Transl Androl Urol 2021;10:2384-96. [Crossref] [PubMed]
- He K, Liu Y, Li D, et al. Combination of transurethral resection of the prostate and flexible and rigid ureteroscopy for benign prostatic hyperplasia and ureteral calculus. Transl Androl Urol 2021;10:3395-3401. [Crossref] [PubMed]
- Lotterstätter M, Seklehner S, Wimpissinger F, et al. Transurethral resection of the prostate in 85+ patients: a retrospective, multicentre study. World J Urol 2022;40:3015-20. [Crossref] [PubMed]
- Li Z, Zheng Z, Liu X, et al. Venous Thromboembolism and Bleeding after Transurethral Resection of the Prostate (TURP) in Patients with Preoperative Antithrombotic Therapy: A Single-Center Study from a Tertiary Hospital in China. J Clin Med 2023;12:417. [Crossref] [PubMed]
- Ma ZZ, Han YX, Wang WZ, et al. The use of a homemade rate adjustment card in patients with continuous bladder irrigation after transurethral resection of the prostate. Transl Androl Urol 2020;9:2227-34. [Crossref] [PubMed]
- Deljou A, Soleimani J, Olive EJ, et al. Bladder spasms following ambulatory urologic procedures. Can J Urol 2022;29:11175-81. [PubMed]
- Fok KH, Shaikh S, Jayatunga R, et al. An Autonomous Continuous Bladder Irrigation System. J Endourol 2023;37:1063-9. [Crossref] [PubMed]
- Ding A, Cao H, Wang L, et al. A novel automatic regulatory device for continuous bladder irrigation based on wireless sensor in patients after transurethral resection of the prostate: A prospective investigation. Medicine (Baltimore) 2016;95:e5721. [Crossref] [PubMed]
- Rodenbaugh D, Vo CT, Redulla R, et al. Nursing Management of Hepatic Encephalopathy. Gastroenterol Nurs 2020;43:E35-47. [Crossref] [PubMed]
- Ma ZZ, Zhang HB, Niu ME, et al. Construction of pelvic floor muscle rehabilitation training program for patients undergoing laparoscopic radical prostatectomy. Transl Cancer Res 2022;11:392-402. [Crossref] [PubMed]
- Zeng XT, Jin YH, Liu TZ, et al. Clinical practice guideline for transurethral plasmakinetic resection of prostate for benign prostatic hyperplasia (2021 Edition). Mil Med Res 2022;9:14. [Crossref] [PubMed]
- McGaughey J, Fergusson DA, Van Bogaert P, et al. Early warning systems and rapid response systems for the prevention of patient deterioration on acute adult hospital wards. Cochrane Database Syst Rev 2021;11:CD005529. [PubMed]
- Lucas A, Ward CW. Manual and continuous bladder irrigation: Best practices. Nursing 2022;52:31-6. [Crossref] [PubMed]
- Zheng Q, Wang R, Shi Y, et al. Effects of acupoint massage combined with relaxation therapy on patients with postoperative fatigue syndrome after lumbar surgery. Medicine (Baltimore) 2021;100:e25849. [Crossref] [PubMed]
- Cosmi B, Legnani C, Libra A, et al. D-Dimers in diagnosis and prevention of venous thrombosis: recent advances and their practical implications. Pol Arch Intern Med 2023;133:16604. [Crossref] [PubMed]


