
Time to complication after primary pediatric hypospadias repair with transverse preputial island flap urethroplasty
Highlight box
Key findings
• In this study, we investigated time to first complication following transverse preputial island urethroplasty. More than 90% of complications after the transverse preputial island urethroplasty of hypospadias occurred within 1 year, with those related to proximal hypospadias presenting earlier than those of midshaft/distal hypospadias.
What is known and what is new?
• It is known that the incidence of complications after hypospadias surgery is high, and that complications tend to occur in a concentrated period after surgery, but late complications are not uncommon. The longer the follow-up period, the more complications we will find.
• Our study found that more than 90% of complications after the transverse preputial island urethroplasty of hypospadias occurred within one year, with those related to proximal hypospadias presenting earlier than those of midshaft/distal hypospadias. Urethral diverticula appeared later than other complications.
What is the implication, and what should change now?
• This suggests that surgeons should conduct frequent follow-ups within first year post-operation to detect these complications as early as possible. Thereafter, parents were contacted by telephone every 3 months during the first postoperative year to monitor the development of complications. Given the delayed onset of complications, it is essential for surgeons to educate both patients and parents about hypospadias and make them aware of the possibility of long-term complications.
Introduction
Hypospadias is one of the most common congenital malformations in men with an incidence of approximately five to fifty per ten thousand (1). The aim of surgical repair of hypospadias is to restore normal voiding and sexual function as well as achieving a good cosmetic outcome. Various methods have been proposed for the repair of hypospadias, but the transverse preputial island urethroplasty is still widely used in China, especially for moderate and severe cases due to its convenient prepuce of the penis (2). The incidence of complications after the transverse preputial island urethroplasty for hypospadias ranges from 34% to 59% (3-5). The best follow-up time after hypospadias repair is still controversial. Some studies suggest that most complications occur within 1 year after the surgery, while others report a significant number of complications occurring 1 year or later (6-10). However, little is currently known about the time to first occurrence of postoperative complications. Therefore, the aim of this study is to describe the time to first complication after the transverse preputial island urethroplasty based on severity of hypospadias and age stratification and pay attention to the time of occurrence of different types of complications. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-24-135/rc).
Methods
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of Beijing Children’s Hospital, Capital Medical University (No. [2023]-E-118-R) and individual consent for this retrospective analysis was waived. This study is a collection of hypospadias cases diagnosed at Beijing Children’s Hospital Affiliated to Capital Medical University between December 2018 and December 2019. The inclusion criteria were as follows: children with hypospadias who underwent their first hypospadias operation in our hospital using the transverse preputial island urethroplasty, with complete clinical data. The exclusion criteria included incomplete clinical data, other surgical methods, staging operation and not repaired for the first time in our hospital. The clinical data collected included age at the time of operation, curvature, severity of hypospadias (distal, midshaft, proximal), type of complications, follow-up time and the time of the first postoperative complications. The age at operation was divided into two categories: age at least 18 months and age less than 18 months, as most children begin toilet training around the age of 18 months. The severity of hypospadias was classified based on the position of the urethral orifice after the correction of the penile curvature, including distal (distal third of penile shaft to glans), mid (penoscrotal junction to distal third of penile shaft) and proximal (perineum to penoscrotal junction). The main complications of interest were urethral fistula, urethral stricture, urethral diverticulum and persistent chordee. For children with multiple complications, only the first complication was considered. The time to complication was defined as the interval between the first postoperative complication and the operation. This data were collected through electronic medical record inquiry and telephone follow-up to the parents of the children. The degree of penile curvature was measured by the surgeon using a protractor under anesthesia. All erection tests were performed with tourniquet. After the hypospadias repair surgery, the catheter is kept for 3–4 weeks. Within 5 days after the surgery, second-generation cephalosporin is administered intravenously to prevent infection. The scrotal dressing is removed on the 5th postoperative day and oral second-generation cephalosporin is taken for 1 week. The hospital stay is about 1 week. All parents of the children were registered with their phone numbers during their hospital stay, and they were regularly contacted by phone to confirm the appearance of complications.
Surgical techniques
A circumferential incision was made proximal to the corona that reached the depth of the Buck fascia, allowing for degloving and chordee release. Subsequently, we transected the urethral plate if the penis could not be straightened owing to severe chordee and dropped back the meatus to the penoscrotal junction or the proximal shaft. Dorsal plication was performed if the chordee was still present. The flap length was determined as the distance from the retracted meatus to the glans tip after straightening the curvature. A twelve millimeters wide rectangular flap was harvested from the inner prepuce, and the mobilized foreskin was rolled into a tube over a catheter. The glans channel was then created, and the neourethra was transposed ventrally and brought through the channel. Choose a 6- or 8-gauge catheter based on the size of the glans. Additional fixation of the transverse preputial island flap (TPIF) to the midline of the corpus was performed. The neourethra was anastomosed with the native urethra, and the distal meatus was attached to the top of the glans with interrupted fine sutures.
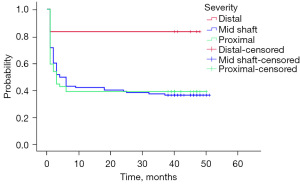
Statistical analyses
The statistical analysis of the data was performed using SPSS version 27.0. Descriptive statistics were performed to assess basic patient demographic information. The measurement data that did not obey the normal distribution were described by the median and interquartile range (IQR). Comparative statistical analysis was performed with Mann-Whitney U test for nonparametric continuous variables. The counting data were described using the number of cases and percentage, and inter-group comparisons were made using the Chi-squared test. A univariate survival analysis was performed using Kaplan-Meier curves for clinical variables and time to complication.
Results
Between December 2018 and December 2019, a total of 172 children underwent the transverse preputial island urethroplasty for hypospadias in Beijing Children’s Hospital affiliated with Capital Medical University. A total of 7 children were lost to contact, so a total of 165 children were included in the study. During the follow-up period, complications occurred in 101 cases (61.2%). The incidence of complications among distal, middle, and proximal hypospadias was 16.7% (1/6), 63.8% (67/105), and 61.1% (33/54), respectively (P=0.07). The median operative age of all children was 23.0 months (IQR, 19.0–29.0 months), and the median operative ages of distal, middle, and proximal hypospadias were 21.5 (IQR, 15.5–24.5), 23.0 (IQR, 19.0–29.5), and 24.0 (IQR, 19.75–29.5) months, respectively. The median follow-up time for all children was 45.0 months (IQR, 40.0–48.0 months), and the median follow-up times for distal, middle, and proximal hypospadias were 46.0 (IQR, 40.7–48.0), 45.0 (IQR, 40.5–48.0), and 45.0 (IQR, 40.0–47.0) months, respectively. Before the operation, the degree of penile curvature in all patients was ≥30°, and the median degree of penile curvature was 60.00° (IQR, 45.00°–80.00°). The median degree of penile curvature in distal, middle, and proximal hypospadias cases was 72.50° (IQR, 60.00°–92.50°), 60.00° (IQR, 45.00°–72.50°), and 67.50° (IQR, 50.00°–80.00°), respectively. The incidences of urethral fistula, urethral stricture, urethral diverticulum, and penile curvature were 32.7%, 13.3%, 13.9%, and 1.2%, respectively (Table 1).
Table 1
| Variables | Distal (n=6) | Midshaft (n=105) | Proximal (n=54) | Overall | P |
|---|---|---|---|---|---|
| Complication | 1 (16.7) | 67 (63.8) | 33 (61.1) | 101 (61.2) | 0.07 |
| Fistula | 1 (16.7) | 36 (34.3) | 17 (31.5) | 54 (32.7) | 0.22 |
| Diverticulum | 0 | 16 (15.3) | 6 (11.1) | 22 (13.9) | 0.66* |
| Stenosis/stricture | 0 | 13 (12.4) | 10 (18.5) | 23 (13.3) | 0.22* |
| Persistent chordee | 0 | 2 (1.9) | 0 | 2 (1.2) | – |
| Age (months) | 21.5 [15.5–24.5] | 23.0 [19.0–29.5] | 24.0 [19.75–29.5] | 23.0 [19.0–29.0] | 0.46 |
| ≥18 | 4 (66.7) | 91 (86.7) | 48 (88.9) | 143 (86.6) | 0.32 |
| <18 | 2 (33.3) | 14 (13.3) | 6 (11.1) | 22 (13.3) | |
| Curvature (°) | 72.50 [60.00–92.50] | 60.00 [45.00–72.50] | 67.50 [50.00–80.00] | 60.00 [45.00–80.00] | 0.08 |
| Time to complication (months) | 1.0 [–] | 2.0 [1.0–3.0] | 1.0 [1.0–2.5] | 1.0 [1.0–3.0] | 0.04 |
| Follow-up duration (months) | 46.0 [40.7–48.0] | 45.0 [40.5–48.0] | 45.0 [40.0–47.0] | 45.0 [40.0–48.0] | 0.69 |
Data are presented as n (%) or median [interquartile range]. *, Chi-square test was used to compare the midshaft group with the proximal group.
Out of the 101 children who experienced complications, 94.1% of the complications occurred within 1 year, whereas in five cases, complications occurred after 1 year. The median time of occurrence of complications was 1.0 (IQR, 1.0–3.0 months). The median time of occurrence of complications for midshaft/distal and proximal hypospadias was 2.0 (IQR, 1.0–3.0) and 1.0 (IQR, 1.0–2.5) months, respectively (P=0.04). The median time of complications for patients with surgical age at least 18 months and less than 18 months was 1.0 (IQR, 1.0–3.0) and 2.0 (IQR, 2.0–19.5) months, respectively (P=0.004). Kaplan-Meier survival analysis showed that age less than 18 months and the severity of hypospadias were statistically significant (P=0.005 and P=0.04, respectively) (Figures 1,2). Among all the children, the median complication-free survival time was 4.0 months (IQR, 1.0–41.50 months). Kaplan-Meier survival analysis revealed no significant difference in age (P=0.26) and hypospadias severity (P=0.17) (Figures 3,4). The median time of occurrence of urethral fistula, urethral diverticulum, urethral stricture, and penile curvature was 1.0 (IQR, 1.0–2.0), 3.0 (IQR, 2.0–6.0), 1.0 (IQR, 1.0–3.0), and 10.0 months (P<0.001), respectively. The time to urethral diverticulum was significantly longer than that of urethral fistula and urethral stricture.



Discussion
In this study, the overall incidence of complications after hypospadias repair using the transverse preputial island urethroplasty was found to be 61.2%, and the median follow-up time was 45.0 months. The incidence of distal complications was 16.7%, while the incidence of proximal complications was higher at 61.1%. The median follow-up time for distal and proximal complications was 46.0 and 45.0 months, respectively, which is consistent with the incidence reported in previous studies (3-5). Currently, the specific follow-up time for postoperative complications of hypospadias remains unclear. This study offers a comprehensive analysis of the time to first complication following the transverse preputial island urethroplasty for hypospadias repair, based on a large sample size from a tertiary children’s hospital.
Several previous studies have confirmed that postoperative complications for hypospadias procedures occur more frequently in certain postoperative periods (6-9). Kim et al. revealed that complications from repair of proximal hypospadias with curvature >30° are likely to occur within 2 years of surgery. In all patients, the median time for postoperative complications was more than 1 year (6). Snodgrass and colleagues evaluated the development of complications after TIP in 887 patients and found that 14.1% of the patients experienced complications after the procedure, with 81% of these complications occurring within 1 year, and a median time for complications of 6 months (7). In our study, the median time for complications to occur was 1 month, and approximately 94% of complications appeared within the first year. The early onset of complications after hypospadias surgery highlights the importance of more frequent follow-up during the first 2 years after surgery.
In contrast, a single institution series by Lucas et al. showed a median time for complications of 14.5 months, with a similar incidence of complications within 1 year and 1–5 years (47%), and 6.5% of complications occurring after 5 years (11). The study by Spinoit et al. showed 47.37% of complications occurred within first year post-surgery (12). During a long-term follow-up of Cambareri et al. that spanned up to 25 years, with an average follow-up of 47 months, 54% of patients developed complications after 1 year, and 31% after 3 years (13). Differences in the severity of hypospadias, curvature and surgical techniques may explain the differences in results. Compared with these researches, we found a higher incidence of meso-proximal hypospadias (96.3%) and more severe curvature, with a median curvature of 60.00° (IQR, 45.00°–80.00°).
In our study, five children experienced complications after 1 year, with the longest time to develop complications being 37 months. Obviously, longer follow-up typically reveals more complications. Long-term complications are not uncommon in some reports, as noted in previous studies (8-10,14). In some reports on urethral fistula after hypospadias surgery, although more than 70% of cases occur within 1 year after the operation, it may take more than a decade to detect all cases. Wood et al. performed a probability analysis of 26 patients in whom a urethral fistula developed after hypospadias repair and found that it took 150 months to detect 95% of the fistulas, and up to 17 years to identify all of the urethral fistulas (8). Liao et al. evaluated 112 children with urethral fistula (9). They revealed that 73% of cases occurred within 1 year, with a median time of 8.5 months after the operation. The longest duration was 13.9 years after the operation. The research of 151 children with urethral fistula by Ashley W. Johnston et al., twelve cases of urethral fistula occurred after 5 years, with the latest appearing 15.8 years after the operation (10). Nuininga et al. reported on 126 children who underwent single-stage hypospadias repair and were followed up for at least 10 years. The overall incidence of complications was 54%, with 31.5% of complications occurring after 5 years. The longest time for complications to develop was 14 years (14).
Various factors can cause delayed complications, and currently, there is no reliable method to predict the time when they may occur. In a study of 82 Tanner two-five patients, Snodgrass and colleagues found that the occurrence time of complications was bimodal, with 80% of the complications happening before puberty and 15% occurring during adulthood. Only 5% of patients experienced complications during puberty. The authors suggested that there were relatively fewer complications during the penile growth process in adolescence (15). In some reports on the complications of hypospadias in adulthood, it is suggested that postoperative complications of hypospadias can be a lifelong problem, and relying solely on surgeon follow-up is impractical (16,17). Detecting complications early and dealing with them in a timely manner are essential to reduce the psychological impact on children, improve satisfaction with the appearance of genitals, and potentially enhance sexual function (18). It is crucial for parents and patients who are entering puberty to understand the disease fully, pay close attention to urination, and regularly update surgeons on any feedback or concerns they may have.
In the postoperative follow-up of patients with hypospadias, various factors need to be considered, including sexual psychology, function, and cosmetic results in adolescence and adulthood. In a questionnaire survey of 43 patients with hypospadias by Jiao et al., 53.5% of patients expressed dissatisfaction with the appearance of the penis, primarily due to the small size of the penis or persistent downward curvature. Additionally, 23% of the patients had issues with erectile quality, with patients who had proximal hypospadias being more likely to face problems with penile appearance and erectile quality when compared with patients who had distal hypospadias (19). In study by Liu et al., 102 children with a median age of 24, 29.4% of patients expressed dissatisfaction with the appearance of the penis, and 30% had erectile problems (18). The level of sexual inhibition was positively correlated with the number of operations and the patients’ age at the time of the completion of the operation. Furthermore, the authors found that the incidence of sexual depression in people with a high understanding of hypospadias was lower than that of those with a lower understanding of the disease. Compared to the distal type, patients with proximal hypospadias are more likely to be dissatisfied with the appearance of the penis and experience erection and ejaculation problems. Rynja et al. conducted a meta-analysis on the sexual psychology and cosmetic effects of patients who underwent hypospadias repair in adulthood, finding that compared to the control group, patients were less satisfied with the appearance of the penis and their sexual life (20). In our study, complications in adulthood could not be evaluated due to the surgical age and follow-up time of the patients.
We utilized Kaplan-Meier curve for complication-free survival analysis and compared the median time of complications with different degrees of hypospadias, revealing that the time to complications was related to the severity of hypospadias. The median time for complications of midshaft/distal hypospadias was longer than that of proximal hypospadias (P=0.038), consistent with the findings of Lucas et al. (11). Kim’s study also demonstrated that complications of proximal hypospadias occurred earlier than other types (6). We also discovered that postoperative complications appeared earlier in children with a surgical age at least 18 months (P=0.005). We speculate that after 18 months of age, most parents initiate toilet training for their children, and thus they pay more attention to their children’s urination, leading to an earlier detection of complications. Moreover, we compared the occurrence time of complications according to the type of complications and noted that the occurrence of urethral diverticulum was later than that of urethral fistula and urethral stricture. Formation of a urethral diverticulum is not uncommon following transverse preputial island urethroplasty. Reasons for its formation may be associated with the presence of a distal stricture, inelastic prepuce, and unsmooth prepuce. This causes urine to become blocked or turbulent as it passes through the formed urethra, gradually forming a diverticulum locally. This is a relatively slow process, so urethral diverticulum often appears later than urethral stenosis and urethral fistula.
Our study has several limitations. Firstly, our follow-up duration was limited, and we only focused on surgical complications, and we did not pay attention to the psychosexual effects and sexual function of children as they entered adolescence and adulthood. As our study was retrospective, some medical records of the children were missing during follow-up, which could potentially impact the final results. Additionally, even though our center is the largest pediatric urological institution in China, the proficiency and habits of surgeons with different qualifications in hypospadias repair may affect the occurrence of complications in varying ways.
Conclusions
More than 90% of complications after the transverse preputial island urethroplasty of hypospadias occur within 1 year, with those related to proximal hypospadias presenting earlier than those of midshaft/distal hypospadias. This suggests that surgeons should conduct frequent follow-ups within first year post-operation to detect these complications as early as possible. Thereafter, parents were contacted by telephone every 3 months during the first postoperative year to monitor the development of complications. Given the delayed onset of complications, it is essential for surgeons to educate both patients and parents about hypospadias and make them aware of the possibility of long-term complications. Similarly, surgeons should also consider the need for long-term follow-up care.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-24-135/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-135/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-135/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-135/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the ethics board of Beijing Children’s Hospital, Capital Medical University (No. [2023]-E-118-R) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Springer A, van den Heijkant M, Baumann S. Worldwide prevalence of hypospadias. J Pediatr Urol 2016;12:152.e1-7. [Crossref] [PubMed]
- Duckett JW Jr. Transverse preputial island flap technique for repair of severe hypospadias. Urol Clin North Am 1980;7:423-30. [Crossref] [PubMed]
- Dewan PA, Dinneen MD, Winkle D, et al. Hypospadias: Duckett pedicle tube urethroplasty. Eur Urol 1991;20:39-42. [Crossref] [PubMed]
- Cousin I, Basmaison C, Cousin E, et al. Complication rates of proximal hypospadias: meta-analyses of four surgical repairs. J Pediatr Urol 2022;18:587-97. [Crossref] [PubMed]
- Cui X, He Y, Huang W, et al. Clinical efficacy of transverse preputial island flap urethroplasty for single-stage correction of proximal hypospadias: a single-centre experience in Chinese patients. BMC Urol 2020;20:118. [Crossref] [PubMed]
- Kim JK, Shiff M, Chua ME, et al. Time to event analysis for post-hypospadias repair complications: a single-surgeon experience. World J Urol 2021;39:3913-9. [Crossref] [PubMed]
- Snodgrass W, Villanueva C, Bush NC. Duration of follow-up to diagnose hypospadias urethroplasty complications. J Pediatr Urol 2014;10:208-11. [Crossref] [PubMed]
- Wood HM, Kay R, Angermeier KW, et al. Timing of the presentation of urethrocutaneous fistulas after hypospadias repair in pediatric patients. J Urol 2008;180:1753-6. [Crossref] [PubMed]
- Liao AY, Smith GH. Urethrocutaneous fistulae after hypospadias repair: When do they occur? J Paediatr Child Health 2016;52:556-60. [Crossref] [PubMed]
- Johnston AW, Jibara GA, Purves JT, et al. Delayed presentation of urethrocutaneous fistulae after hypospadias repair. J Pediatr Surg 2020;55:2206-8. [Crossref] [PubMed]
- Lucas J, Hightower T, Weiss DA, et al. Time to Complication Detection after Primary Pediatric Hypospadias Repair: A Large, Single Center, Retrospective Cohort Analysis. J Urol 2020;204:338-44. [Crossref] [PubMed]
- Spinoit AF, Poelaert F, Groen LA, et al. Hypospadias repair at a tertiary care center: long-term followup is mandatory to determine the real complication rate. J Urol 2013;189:2276-81. [Crossref] [PubMed]
- Cambareri GM, Yap M, Kaplan GW. Hypospadias repair with onlay preputial graft: a 25-year experience with long-term follow-up. BJU Int 2016;118:451-7. [Crossref] [PubMed]
- Nuininga JE. Long-term outcome of different types of 1-stage hypospadias repair. J Urol 2005;174:1544-8; discussion 1548. [Crossref] [PubMed]
- Snodgrass W, Bush N. Do New Complications Develop during Puberty after Childhood Hypospadias Repair? J Urol 2022;208:696-701. [Crossref] [PubMed]
- Myers JB, McAninch JW, Erickson BA, et al. Treatment of adults with complications from previous hypospadias surgery. J Urol 2012;188:459-63. [Crossref] [PubMed]
- Barbagli G, De Angelis M, Palminteri E, et al. Failed hypospadias repair presenting in adults. Eur Urol 2006;49:887-94; discussion 895. [Crossref] [PubMed]
- Liu G, Yuan J, Feng J, et al. Factors affecting the long-term results of hypospadias repairs. J Pediatr Surg 2006;41:554-9. [Crossref] [PubMed]
- Jiao C, Wu R, Xu X, et al. Long-term outcome of penile appearance and sexual function after hypospadias repairs: situation and relation. Int Urol Nephrol 2011;43:47-54. [Crossref] [PubMed]
- Rynja SP, de Jong TP, Bosch JL, et al. Functional, cosmetic and psychosexual results in adult men who underwent hypospadias correction in childhood. J Pediatr Urol 2011;7:504-15. [Crossref] [PubMed]


