
Management considerations and treatment outcomes for newly diagnosed prostate cancer in advanced age patients (≥80 years): real-world data from a single urological center over a 10-year period
Highlight box
Key findings
• Advanced age patients with prostate cancer (PCa) have distinct characteristics, such as higher prostate-specific antigen levels, positive biopsy rates, and more advanced grading and staging. In medically fit elderly patients, particularly those with localized PCa and a life expectancy of at least 5 years, definitive therapy could potentially improve survival outcomes.
What is known and what is new?
• The advanced age population with PCa has been growing annually, with conservative therapy emerging as the primary treatment choice. To date, there are no definitive guidelines specifically tailored for this demographic.
• This study demonstrated that definitive therapy could be a good choice for medically fit elderly PCa patients.
What is the implication, and what should change now?
• This study underscores the importance of prioritizing screening for this population. Additionally, it indicates that treatment options for physically fit advanced age patients with PCa should be approached more aggressively.
Introduction
Prostate cancer (PCa) is a significant global health concern, ranking as the second most common cancer and the fifth leading cause of cancer-related deaths among men in 2020. With approximately 1.4 million new cases and 375,000 deaths worldwide, the burden of PCa is expected to rise due to factors like population aging and economic growth (1,2). The average life expectancy for men has increased, and by 2040, the number of new PCa cases is projected to reach 2.3 million, with 740,000 deaths (3,4). To address the needs of the expanding advanced age population affected by PCa, it is essential to develop customized diagnostic strategies.
Considering the increased prevalence of medical comorbidities and diminished physical functional capacity in older patients, there exists a significant risk of undertreatment among elderly men who frequently present with high-grade PCa (5). For example, in the United States, only 41% of high-risk patients aged 75 and older receive curative treatment, compared to 88% of patients aged 65–74 (6). Age, while a simpler factor for determining definitive treatment in relation to life expectancy, is an inaccurate and unreliable factor. Instead, treatment decisions should not rely solely on age, but should consider factors such as life expectancy, comorbidities, geriatric assessment, tumor staging, and patient preferences (5-7). However, definitive treatment for localized disease should not be deferred in older men due to concerns about declines in quality of life (8,9). Therefore, effectively managing this population requires careful consideration of the risks and benefits of definitive treatment, as these men are susceptible to both overtreatment and undertreatment of their disease.
This study aims to investigate the detection rate of PCa in patients aged 80 years or older and evaluate the clinical outcomes of different treatment modalities over a 10-year period in a large urological center. By conducting this study, we hope to enhance our understanding of PCa detection and treatment in the advanced age population. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-24-134/rc).
Methods
Study design and population
This retrospective study, conducted at The Second Hospital of Tianjin Medical University, analyzed data from patients who underwent prostate biopsy for suspected PCa between February 2012 and June 2022. The study included patients aged 80 years or older who had not previously undergone a biopsy. Exclusion criteria comprised incomplete clinical records and concurrent malignancies. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of The Second Hospital of Tianjin Medical University (No. KY2024K160) and patient informed consent was exempted due to the retrospective nature of this study.
Data collection
The following information was collected at the time of diagnosis: age, weight, height, presence of comorbidities (such as hypertension, diabetes, coronary heart disease, cerebrovascular disease, and other tumors), total prostate-specific antigen (PSA), free PSA, prostate volume (PV), PSA density (PSAD), International Society of Urological Pathology (ISUP) grading, biopsy results, and final pathology results. In addition, life expectancy was estimated based on age, and screening tools such as Geriatric 8 (G8), Comprehensive Geriatric Assessment (CGA), and Cumulative Illness Rating Score-Geriatrics (CISR-G) were utilized to screen for health status (9). Additionally, the Charlson Comorbidity Index (CCI), which predicts long-term survival regardless of age and incorporates various comorbidities, was documented for each participant (10). For elderly patients who are either unable or unwilling to undergo local treatment, palliative therapy encompasses active surveillance, watchful waiting, and androgen deprivation therapy (ADT). In contrast, definitive local therapy, such as surgery or radiation therapy, is employed for those opting for aggressive intervention. Follow-up assessments were conducted at regular intervals following treatment, and these assessments continued until PSA progression, clinical or biochemical recurrence, or death.
Definitions of survival outcomes
In this study, the following definitions were used for survival outcomes: progression-free survival (PFS) was defined as the time from the start of treatment to the time when total PSA reached the nadir plus 2 ng/mL, based on the Phoenix criteria (11). Cancer-specific survival (CSS) was defined as the time from the start of treatment to death due to tumor progression. Overall survival (OS) was defined as the time from the start of treatment to patient death, regardless of the cause.
Statistical analysis
Statistical analysis was conducted with Excel 15 (Microsoft, Redmond, CA, USA) and SPSS 22.0 (IBM Corp., Armonk, NY, USA) for baseline characteristics. Descriptive statistics provided median and interquartile range (IQR) for continuous variables and absolute/relative frequencies for categorical variables. Cross-group comparisons was performed with Chi-squared or Fisher’s exact test for categorical data, and t-test or Kruskal-Wallis test for continuous data. To minimize the risk of bias and improve the comparability of treatment effects, propensity score matching (PSM) was used to compare the oncological results between the palliative therapy and definitive therapy. Kaplan-Meier method assessed survival time, reporting median survival with 95% confidence intervals. Median follow-up was calculated via reverse Kaplan-Meier. Log-rank test compared survival distributions, and Cox proportional hazard model analyzed survival. Multivariate analysis employed stepwise variable selection (P<0.05). Missing data were not imputed.
Results
Population and clinical characteristics
Between February 2012 and June 2022, a total of 4,333 suspected PCa patients underwent prostate biopsy in our urological center. Among them, 376 (8.68%) patients were aged 80 or older, and 317 cases were pathologically confirmed as malignant tumors after biopsy. After excluding three cases with special pathologies and 18 cases with concurrent other malignancies, a total of 296 advanced age patients with PCa were eligible for inclusion (Figure 1). Table S1 presents the clinical characteristics and pathological data of the patients. The median PSA value is 37.2 ng/mL (IQR, 16.8–114.3 ng/mL), with 89.9% of cases classified as clinically significant cancer (ISUP ≥2). Of the cases, 55.4% were localized PCa, 19.9% were node-positive, and 24.66% had bone metastasis.
Regarding different treatment approaches, a majority of 256 patients (86.5%) received palliative therapy, whereas a smaller group of 40 patients (13.5%) underwent definitive therapy. An analysis of the clinical characteristics indicated that patients who were younger, exhibited lower PSA levels and PSAD, possessed a higher body mass index (BMI), had a longer anticipated lifespan, presented with fewer positive biopsy cores, demonstrated lower ISUP grades, and displayed no evidence of bone or lymphatic metastasis were more inclined to opt for the combination of definitive therapy (Table 1). In addition, patients in the definitive therapy group had significantly higher CCI scores and G8 scores compared to those in the palliative therapy group (P<0.001). Furthermore, the CGA and CISR-G scores were lower in the definitive therapy group compared to the palliative therapy group (P<0.001). During a median follow-up period of 32.5 months (31 months for the palliative therapy group and 47.5 months for the definitive therapy group), the outcomes were as follows: 3 out of 40 patients in the definitive therapy group had deceased, while 73 out of 256 patients in the palliative therapy group had passed away. Most patients were in the last 5 years, and the median follow-up period was slightly shorter compared to other studies.
Table 1
| Parameter | Total (n=296) | Palliative therapy (n=256) | Definitive therapy (n=40) | P value |
|---|---|---|---|---|
| Median age (years) | 82 [81–84] | 83 [81–85] | 81 [80–83] | <0.001 |
| Median body mass index (kg/m2) | 23.4 [21.8–25.6] | 23.2 [21.5–25.4] | 24.3 [23.0–26.5] | 0.01 |
| Median PSAD (ng/mL/cm3) | 0.84 [0.39–1.93] | 1.02 [0.43–2.12] | 0.40 [0.27–0.76] | <0.001 |
| Median PSA at biopsy (ng/mL) | 37.2 [16.8–114.3] | 43.7 [19.5–120.0] | 19.0 [10.5–41.5] | <0.001 |
| PSA (ng/mL) | <0.001 | |||
| 4–20 | 88 (29.7) | 66 (25.8) | 22 (55.0) | |
| 20.01–50 | 80 (27.0) | 70 (27.3) | 10 (25.0) | |
| 50.01–100 | 50 (16.9) | 46 (18.0) | 4 (10.0) | |
| >100 | 78 (26.4) | 74 (28.9) | 4 (10.0) | |
| CCI scores | 0.40 | |||
| 0 | 180 (60.8) | 153 (59.8) | 27 (67.5) | |
| 1 | 73 (24.7) | 65 (25.4) | 8 (20.0) | |
| ≥2 | 43 (14.5) | 38 (14.8) | 5 (12.5) | |
| Comorbidity | ||||
| Diabetes | 51 (17.2) | 47 (18.36) | 4 (10.0) | |
| Hypertension | 132 (44.6) | 110 (42.97) | 22 (55.0) | |
| CHD | 65 (22.0) | 59 (23.05) | 6 (15.0) | |
| CVD | 36 (12.2) | 32 (12.5) | 4 (10.0) | |
| Expectation of life (years) | 7.39 [6.44–7.90] | 6.91 [6.00–7.90] | 7.9 [6.97–8.43] | <0.001 |
| Screening tool, scores | ||||
| G8 | 13.6±1.49 | 13.4±1.54 | 14.0±1.14 | |
| CGA | 3.43±1.08 | 3.54±1.11 | 3.07±0.86 | |
| CISR-G | 1.00±0.62 | 1.07±0.62 | 0.78±0.57 | |
| Median number of positive cores | 8 [4–12] | 9 [5–12] | 3 [3–9] | <0.001 |
| PNI | 72 (24.32) | 64 (25.00) | 8 (20.0) | 0.54 |
| IDC-P | 30 (10.14) | 27 (10.55) | 3 (7.5) | 0.57 |
| Bone metastasis | 73 (24.66) | 72 (28.13) | 0 | <0.001 |
| Lymphatic metastasis | 59 (19.9) | 57 (22.27) | 2 (5.0) | 0.01 |
| Clinical stage | <0.001 | |||
| cT1 | 11 (3.72) | 9 (3.52) | 2 (5.0) | |
| cT2 | 170 (57.4) | 138 (53.9) | 32 (80.0) | |
| cT3 | 80 (27.0) | 74 (28.9) | 6 (15.0) | |
| cT4 | 35 (11.8) | 35 (13.7) | 0 | |
| ISUP grade | 0.01 | |||
| 1 | 30 (10.1) | 21 (8.2) | 9 (22.5) | |
| 2 | 33 (11.1) | 25 (9.8) | 8 (20.0) | |
| 3 | 39 (13.2) | 33 (12.9) | 6 (15.0) | |
| 4 | 105 (35.5) | 96 (37.5) | 9 (22.5) | |
| 5 | 89 (30.1) | 81 (31.6) | 8 (20.0) | |
| Type of local treatment | ||||
| Radical prostatectomy | 27 (9.12) | 0 | 27 (67.5) | |
| Brachytherapy | 13 (4.39) | 0 | 13 (32.5) | |
| Median time of follow-up (months) | 32.5 [22–53] | 31.0 [22.0–48.1] | 47.5 [22.0–73.0] | 0.01 |
Data are presented as median [IQR] or n (%) or mean ± SD. PSAD, prostate-specific antigen density; PSA, prostate-specific antigen; CCI, Charlson Comorbidity Index; CHD, coronary atherosclerotic heart disease; CVD, cerebrovascular disease; PNI, perineural invasion; IDC-P, intraductal carcinoma of the prostate; ISUP, International Society of Urological Pathology; IQR, interquartile range; SD, standard deviation.
Oncological results
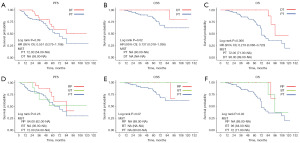
To enhance the comparability of treatment effects and minimize bias, PSM was employed to compare the oncological outcomes of palliative therapy versus definitive therapy. Following a 4:1 nearest neighbor PSM without replacement, a total of 149 patients were successfully matched within the cohort. The matching criteria included age, PSA, CCI, clinical stage, and ISUP to ensure balance across key covariates. The standardized mean differences for all selected covariates were reduced to less than 10% post-matching, indicating successful balance (Table S2). The subsequent stratified analysis using Cox proportional hazards models reaffirmed the significant positive impact of definitive therapy on PFS, CSS, and OS, as presented in Table 2 and Tables S3,S4. Factors such as lymphatic and bone metastasis, ISUP grade 5, and PSAD were identified as associated with PFS. Definitive therapy was associated with a lower risk of cancer progression compared to palliative therapy. In terms of CSS, factors such as lymphatic and bone metastasis, along with the treatment modality, were influential. A higher CCI score was linked to poorer OS, while the presence of lymphatic and bone metastasis negatively impacted OS. Definitive therapy was shown to be associated with improved OS outcomes, highlighting its benefits in enhancing oncological outcomes and patient survival. Additionally, Kaplan-Meier curve analysis further supported these findings, indicating that patients treated with definitive therapy had significantly better PFS and CSS compared to those receiving palliative therapy. The definitive therapy group showed a longer median survival time for both PFS and CSS. Moreover, in terms of OS, the definitive therapy group exhibited superior outcomes with longer median survival time and higher 5- and 10-year survival rates compared to the palliative therapy group. These results emphasize the positive impact of definitive therapy in improving survival outcomes for patients (Figure 2A-2C).
Table 2
| Parameter | Univariate analysis | Cox regression model | |||
|---|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | ||
| Age, years | |||||
| 80–84 | 1.00 (reference) | ||||
| ≥85 | 1.56 (0.95–2.55) | 0.08 | |||
| CCI | |||||
| 0 | 1.00 (reference) | 1.00 (reference) | |||
| 1 | 1.56 (0.89–2.76) | 0.12 | 1.33 (0.71–2.50) | 0.37 | |
| ≥2 | 2.37 (1.29–4.34) | 0.005 | 2.44 (1.24–4.77) | 0.009 | |
| TPSA | |||||
| 4–20 | 1.00 (reference) | 1.00 (reference) | |||
| 20.01–50 | 1.66 (0.84–3.30) | 0.15 | 1.29 (0.56–3.01) | 0.55 | |
| >50 | 2.16 (1.20–3.89) | 0.01 | 1.13 (0.52–2.45) | 0.77 | |
| Clinical stage | |||||
| T1–T2 | 1.00 (reference) | 1.00 (reference) | |||
| T3 | 2.29 (1.39–3.77) | 0.001 | 1.14 (0.56–2.30) | 0.72 | |
| T4 | 4.09 (1.89–8.86) | <0.001 | 0.79 (0.27–2.31) | 0.67 | |
| Lymphatic metastasis | |||||
| None | 1.00 (reference) | 1.00 (reference) | |||
| Yes | 4.30 (2.49–7.41) | <0.001 | 2.74 (1.23–6.14) | 0.01 | |
| Bone metastasis | |||||
| None | 1.00 (reference) | 1.00 (reference) | |||
| Yes | 4.75 (2.77–8.15) | <0.001 | 2.36 (1.13–4.95) | 0.02 | |
| PNI | |||||
| None | 1.00 (reference) | 1.00 (reference) | |||
| Yes | 1.72 (1.04–2.82) | 0.03 | 1.46 (0.82–2.60) | 0.20 | |
| ISUP | |||||
| 1 | 1.00 (reference) | ||||
| 2 | 0.44 (0.13–1.46) | 0.18 | |||
| 3 | 0.81 (0.29–2.26) | 0.69 | |||
| 4 | 1.56 (0.72–3.38) | 0.26 | |||
| 5 | 1.84 (0.82–4.12) | 0.14 | |||
| PSAD | 1.01 (0.99–1.02) | 0.44 | |||
| Therapeutic regimens | |||||
| PT | 1.00 (reference) | 1.00 (reference) | |||
| DT | 0.15 (0.05–0.48) | 0.001 | 0.15 (0.04–0.48) | 0.002 | |
OS, overall survival; CCI, Charlson Comorbidity Index; TPSA, total prostate-specific antigen; PNI, perineural invasion; ISUP, International Society of Urological Pathology; PSAD, prostate-specific antigen density; PT, palliative therapy; DT, definitive therapy; HR, hazard ratio; 95% CI, 95% confidence interval.
Subgroup analysis
In an effort to minimize treatment selection bias, we conducted a subgroup analysis focusing on patients with localized PCa and a life expectancy of over 5 years. The objective was to compare the efficacy of definitive therapy [radical prostatectomy (RP) and brachytherapy (BT)] versus palliative therapy. The estimated 5- and 10-year OS rates in the RP group were 100% and 66%, and for the BT group they were 100% and 38%, compared with those of the palliative therapy group at 60% and 15%. The analysis of Kaplan-Meier survival curves revealed a significant improvement in PFS, CSS and OS in patients who received RP compared to those who received palliative therapy (Figure 2D-2F). Similarly, patients who underwent BT also demonstrated improved CSS and OS when compared to palliative therapy (Figure 2D-2F).
Discussion
On average, PCa is diagnosed at the age of 66 years old, and men who succumb to the disease have an average age of 80 years old (12,13). Generally, younger individuals below 80 years old have better overall health, fewer underlying illnesses, more treatment options, and faster recovery rates. However, older men are often diagnosed with higher-grade and advanced-stage PCa, which puts them at a higher risk of disease progression and premature death (14). In 2008, the US Preventive Services Task Force (USPSTF) recommended against PCa screening for men aged 75 and above, citing a perceived lack of benefit from RP. However, by not screening older patients, there is a missed opportunity to detect aggressive PCa in those who are most likely to have it. The incidence of high-risk PCa increases with age, accounting for a higher percentage of cases in men aged 75 and older compared to younger men (9,15). Relying solely on age-based criteria for screening fails to consider variations in life expectancy based on overall health and other medical conditions. Older men with undiagnosed aggressive tumors face potential morbidity and mortality if their disease progresses, and therefore should not be denied the chance for treatment (12,16). In a study by Masaoka et al. (17) in 2017, using cancer registry data from the Monitoring of Cancer Incidence in Japan project from 2006 to 2008, out of 48,782 cases of PCa, 7,370 (15.1%) were individuals aged 80 or older. The proportions of localized, regional, and distant cancer among men aged 80 or above were 40.2%, 13.4%, and 17.5%, respectively. As one of the largest urological centers in Northern China, we conducted a study examining the detection rates of PCa among different age groups over the past decade. Our analysis included 4,333 individuals with suspicious PCa indicators, yielding the following rates: 78.7% for individuals aged 80 and above, 62.4% for those aged 70–80, 47.8% for those aged 60–70, and 38.3% for individuals under 60 (unpublished data). In the present study, a noteworthy observation was that among patients over 80 years old, 89.86% displayed clinically significant PCa (ISUP ≥2), with 24.66% at the metastasis stage. These findings emphasize the significance of early screenings and interventions, particularly for older individuals, as a means to enhance outcomes.
Managing PCa in patients aged 80 and above can present challenges due to limited treatment options and considerations for life expectancy and comorbidities. While age has been associated with survival, aggressive local therapy has been independently linked to better OS, even after adjusting for age (18,19). According to the US Social Security Index actuarial life table, an 80-year-old man of average health would still have a life expectancy of approximately 7.74 years, while an 85-year-old man would have a life expectancy of around 5.47 years. Several guidelines, including those from the European Association of Urology (EAU) and the National Comprehensive Cancer Network (NCCN), now emphasize considering life expectancy rather than just biological age (20,21). It is crucial for treatment decisions to be made in consultation with healthcare professionals who take into account the individual’s health status and preferences (22). According to the 2019 consensus of the International Society of Geriatric Oncology, treatment decisions should be based on the individual health status of men aged 75 and older, rather than solely relying on their age (9). It is crucial to counsel elderly patients, especially those with good overall health, on the potential risk of PCa-specific mortality if curative treatment is not pursued. The G8 screening tool simplifies health assessment for older men with localized PCa by considering age and seven items from the Mini Nutritional Assessment questionnaire. It calculates a total score from 0 to 17, with a score above 14 indicating good health and the need for standard treatment. Additionally, the CCI can evaluate overall health by looking at existing medical conditions. A higher CCI score suggests more comorbidities, which can impact treatment decisions and outcomes. In this study, we found that only 13.5% of elderly patients underwent definitive therapy after being diagnosed with PCa over a 10-year period. Those who received definitive therapy had higher G8 scores and lower CCI scores compared to those who received palliative therapy. This suggests that medically “fit” elderly patients are more inclined to opt for local curative therapy in real-world scenarios.
In regards to different treatment modalities, a study by Fischer-Valuck et al. in 2022 indicated that in elderly patients with high-risk PCa, definitive local treatments such as RP or radiotherapy (RT) with or without ADT were associated with a 50% reduction in overall mortality compared to surveillance alone or ADT alone (23). Besides, advances in treatment techniques have also led to improved outcomes and reduced complications in older patients with PCa (24,25). Moreover, external beam radiation therapy (EBRT), BT, or a combination of both can be effective for localized PCa, especially for low- to intermediate-risk disease, while surgery remains the preferred option for high-risk disease. High-dose rate BT boost has shown promising disease control rates with minimal side effects in elderly patients (26,27). Similar positive outcomes were observed in the study by Kishan et al., where among patients with Gleason scores of 9–10 PCa, treatment with EBRT plus BT combined with ADT was associated with significantly lower PCa-specific mortality and longer time to distant metastasis compared to treatment with EBRT and ADT alone or RP (28). Despite our cohort being of advanced age, these patients with better physical status should be considered for more aggressive definitive treatment regimens. Subgroup analysis of this study revealed that radical surgery resulted in longer median survival (CSS and OS) for localized elderly patients with a life expectancy of over 5 years, and radiation therapy, specifically BT without EBRT, was seen as a viable alternative to surgery for patients with mild physical limitations or who preferred non-surgical options. This study overall suggests that medically “fit” elderly patients can achieve treatment outcomes similar to younger patients in terms of effectiveness. Furthermore, the increasing use of tissue-based genetic testing in PCa, especially among younger patients, is attributed to their longer life expectancy, allowing for a more informed decision-making process (29,30). However, based on our findings that elderly patients experience better survival outcomes with more aggressive measures, the utilization of genetic testing in the elderly population may also yield promising results for our management strategies.
Our study has several important limitations that warrant consideration. Firstly, being a retrospective study makes it susceptible to biases that could impact its reliability. Additionally, the significance of addressing missing data and its implications on the strength of our findings cannot be overstated. It is imperative to validate treatment outcomes for elderly “fit” patients through prospective trials. Secondly, the disparity in the number of patients undergoing local definitive therapy versus palliative therapy may skew our survival results. With advancements in surgical and radiation techniques, more elderly patients may opt for local treatments, potentially altering our research conclusions. We plan to address these biases and any missing data in future analyses to enhance the robustness of our findings. Thirdly, our study primarily focused on survival outcomes and did not thoroughly evaluate tumor-related responses, treatment side effects, and quality of life. This gap is critical for treatment decisions, particularly in patient-reported outcomes. Future research should place more emphasis on assessing patient quality of life alongside survival outcomes, utilizing suitable health assessment tools. This is especially vital for elderly patients, where striking a balance between survival and quality of life is essential. Fourthly, since our study was conducted at a single urological center, its findings may not be universally applicable. To address this limitation, future discussions will explore how our results can be applied to different geographic or healthcare settings, taking into account variations in patient demographics, treatment modalities, and resources. Understanding the broader applicability of our findings is crucial for guiding effective clinical decisions and enhancing patient care. Acknowledging and addressing these limitations will bolster the credibility and relevance of our study in informing PCa treatment strategies tailored to elderly patients.
Conclusions
Our study underscores the significance of managing and treating PCa in patients aged 80 or older. Advanced age patients, despite being a minority, exhibit unique characteristics, such as higher PSA levels, positive biopsy rates, and pathological grading and staging. For medically fit elderly patients, especially those with localized PCa and a life expectancy of ≥5 years, definitive therapy markedly enhances survival outcomes. However, further prospective studies are needed to determine optimal diagnostic strategies and tailored treatment modalities for this unique population.
Acknowledgments
Funding: This work was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-24-134/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-134/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-134/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-134/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of The Second Hospital of Tianjin Medical University (No. KY2024K160) and patient informed consent was exempted due to the retrospective nature of this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- DeSantis CE, Miller KD, Dale W, et al. Cancer statistics for adults aged 85 years and older, 2019. CA Cancer J Clin 2019;69:452-67. [Crossref] [PubMed]
- Global Health Observatory data repository: World Health Organization; 2019 [updated 2020-12-07. Available online: http://apps.who.int/gho/data/view.main.SDG2016LEXREGv?lang=en
- Culp MB, Soerjomataram I, Efstathiou JA, et al. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur Urol 2020;77:38-52. [Crossref] [PubMed]
- Graham LS, Lin JK, Lage DE, et al. Management of Prostate Cancer in Older Adults. Am Soc Clin Oncol Educ Book 2023;43:e390396. [Crossref] [PubMed]
- Hampson LA, Cowan JE, Zhao S, et al. Impact of age on quality-of-life outcomes after treatment for localized prostate cancer. Eur Urol 2015;68:480-6. [Crossref] [PubMed]
- Bian SX, Hoffman KE. Management of prostate cancer in elderly men. Semin Radiat Oncol 2013;23:198-205. [Crossref] [PubMed]
- Hu JC, Nguyen P, Mao J, et al. Increase in Prostate Cancer Distant Metastases at Diagnosis in the United States. JAMA Oncol 2017;3:705-7. [Crossref] [PubMed]
- Boyle HJ, Alibhai S, Decoster L, et al. Updated recommendations of the International Society of Geriatric Oncology on prostate cancer management in older patients. Eur J Cancer 2019;116:116-36. [Crossref] [PubMed]
- Park JW, Koh DH, Jang WS, et al. Age-adjusted Charlson Comorbidity Index as a prognostic factor for radical prostatectomy outcomes of very high-risk prostate cancer patients. PLoS One 2018;13:e0199365. [Crossref] [PubMed]
- Horwitz EM, Thames HD, Kuban DA, et al. Definitions of biochemical failure that best predict clinical failure in patients with prostate cancer treated with external beam radiation alone: a multi-institutional pooled analysis. J Urol 2005;173:797-802. [Crossref] [PubMed]
- Clark R, Vesprini D, Narod SA. The Effect of Age on Prostate Cancer Survival. Cancers (Basel) 2022;14:4149. [Crossref] [PubMed]
- Hori M, Palmer M. Age-specific prostate cancer incidence rate in the world. Jpn J Clin Oncol 2021;51:164-5. [Crossref] [PubMed]
- Pettersson A, Robinson D, Garmo H, et al. Age at diagnosis and prostate cancer treatment and prognosis: a population-based cohort study. Ann Oncol 2018;29:377-85. [Crossref] [PubMed]
- Vatandoust S, Kichenadasse G, O'Callaghan M, et al. Localised prostate cancer in elderly men aged 80-89 years, findings from a population-based registry. BJU Int 2018;121:48-54. [Crossref] [PubMed]
- Godtman RA, Kollberg KS, Pihl CG, et al. The Association Between Age, Prostate Cancer Risk, and Higher Gleason Score in a Long-term Screening Program: Results from the Göteborg-1 Prostate Cancer Screening Trial. Eur Urol 2022;82:311-7. [Crossref] [PubMed]
- Masaoka H, Ito H, Yokomizo A, et al. Potential overtreatment among men aged 80 years and older with localized prostate cancer in Japan. Cancer Sci 2017;108:1673-80. [Crossref] [PubMed]
- Sheng W, Kirschner-Hermanns R, Zhang H. Elderly patients aged ≥ 75 years with locally advanced prostate cancer may benefit from local treatment: a population-based propensity score-adjusted analysis. World J Urol 2019;37:317-25. [Crossref] [PubMed]
- Bandini M, Pompe RS, Marchioni M, et al. Radical prostatectomy or radiotherapy reduce prostate cancer mortality in elderly patients: a population-based propensity score adjusted analysis. World J Urol 2018;36:7-13. [Crossref] [PubMed]
- NCCN. NCCN Clinical Practice Guidelines in Oncology-Prostate Cancer (version: 1.2024) (EB/OL) 2024 [Available online: https://www.nccn.org/guidelines/guidelines-detail?category=1&id=1459
- EAU Guidelines. Edn. presented at the EAU Annual Congress Paris 2024. Available online: https://uroweb.org/guidelines
- Griebling TL. Re: Localised Prostate Cancer in Elderly Men Aged 80-89 Years, Findings from a Population-Based Registry. J Urol 2019;201:838. [Crossref] [PubMed]
- Fischer-Valuck BW, Baumann BC, Brown SA, et al. Treatment patterns and overall survival outcomes among patients aged 80 yr or older with high-risk prostate cancer. Eur Urol Open Sci 2022;37:80-9. [Crossref] [PubMed]
- Traboulsi SL, Nguyen DD, Zakaria AS, et al. Functional and perioperative outcomes in elderly men after robotic-assisted radical prostatectomy for prostate cancer. World J Urol 2020;38:2791-8. [Crossref] [PubMed]
- Marotte D, Chand-Fouche ME, Boulahssass R, et al. Irradiation of localized prostate cancer in the elderly: A systematic literature review. Clin Transl Radiat Oncol 2022;35:1-8. [Crossref] [PubMed]
- Guo XX, Xia HR, Hou HM, et al. Comparison of Oncological Outcomes Between Radical Prostatectomy and Radiotherapy by Type of Radiotherapy in Elderly Prostate Cancer Patients. Front Oncol 2021;11:708373. [Crossref] [PubMed]
- Marotte D, Gal J, Schiappa R, et al. High-dose-rate brachytherapy boost for elderly patients with intermediate to high-risk prostate cancer: 5-year clinical outcome of the PROSTAGE cohort. Clin Transl Radiat Oncol 2022;35:104-9. [Crossref] [PubMed]
- Kishan AU, Cook RR, Ciezki JP, et al. Radical Prostatectomy, External Beam Radiotherapy, or External Beam Radiotherapy With Brachytherapy Boost and Disease Progression and Mortality in Patients With Gleason Score 9-10 Prostate Cancer. JAMA 2018;319:896-905. [Crossref] [PubMed]
- Bologna E, Ditonno F, Licari LC, et al. Tissue-Based Genomic Testing in Prostate Cancer: 10-Year Analysis of National Trends on the Use of Prolaris, Decipher, ProMark, and Oncotype DX. Clin Pract 2024;14:508-20. [Crossref] [PubMed]
- Chung JS, Morgan TM, Hong SK. Clinical implications of genomic evaluations for prostate cancer risk stratification, screening, and treatment: a narrative review. Prostate Int 2020;8:99-106. [Crossref] [PubMed]



