
Iatrogenic ureteroarterial fistula treated by the placement of Allium stent: a case report and literature review
Highlight box
Key findings
• Ureteroarterial fistula (UAF) could be treated by Allium stent placement in an emergency setting.
What is known and what is new?
• UAF is a life-threatening condition which could occur during urologic procedure. The treatment of UAF remains a huge challenge for urologists, especially in an emergency setting.
• Here we report the first UAF case which was successfully treated by the placement of Allium stent.
What is the implication, and what should change now?
• Intraureteral repair with Allium stent is a feasible option for the treatment of UAF in an emergent setting.
• During balloon dilation of ureteral stricture in patients with history of pelvic irradiation, oncologic surgery or chronic ureteral stent, beware of the risk of iatrogenic UAF.
Introduction
Ureteroarterial fistula (UAF) is a rare complication that may occur in patients with long-term indwelling ureteral stents (1-3), and the treatment experience for UAF remains limited. Its treatment remains a huge challenge for urologists, especially in an emergency setting. Traditional treatment option includes open surgical repair (OSR), endovascular repair and intraureteral occlusion (1-3). In this study, we present a case of intraoperative UAF in a patient with chronic indwelling ureteral stent due to post-radiotherapy ureteral stricture, who was successfully treated by the placement of Allium stent. We present this article in accordance with the CARE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-24-191/rc).
Case presentation
On May 5, 2020, a 62-year-old woman presented to Peking University People’s Hospital’s outpatient department complaining of bilateral chronic flank pain. She was previously diagnosed with refractory hydronephrosis and treated by indwelling double-J ureteral stent. However, hydronephrosis was not relieved satisfactorily. Additionally, the patients suffered from long term lower urinary tract symptoms, especially with recent aggravated gross hematuria, and recurrent ureteral calculus. All of these prompted her to pursue a definitive management.
The patient underwent radical hysterectomy in 2017 for cervical cancer and received adjuvant radiotherapy. Three months after hysterectomy, she was diagnosed with bilateral hydronephrosis, left renal calculi and long segment bilateral ureteral stricture. Since then, bilateral double J stents had been indwelled because of persistent hydronephrosis and repetitive urinary tract infection, and she was required to undergo an exchange of urinary stents every 10 months.
She was admitted into our inpatient on the same day. Laboratory examinations upon admission precluded any surgical or anesthesia contraindication, except elevated red blood cells and white blood cells in routine urine test. After consultation with surgeons, she underwent interventional urologic procedure and the implantation of Allium ureteral stent (Allium Medical Solutions Ltd., Caesarea, Israel) was proposed.
The operation took place with the patient in the lithotomy position and under spinal anesthesia. Using a rigid cystoscope, the bladder was accessed, and a guide wire was then inserted retrogradely into the left ureter. The exact location and extent of the ureteral stricture were determined through retrograde radiography, guided by fluoroscopy, which revealed a long segment stenosis from 5 cm below ureteropelvic junction to ureteral meatus. Subsequently, a 6 cm/21 F ureteral balloon dilation catheter was placed at the site of obstruction, and the stricture was dilated to 25 atm pressure for a duration of 3 min. Then it was dilated from top to bottom step by step. After confirming that the narrowed segment was dilated satisfactorily under fluorescence, a 10 mm/12 cm Allium ureteral stent was inserted along the guide wire. Then it was deployed in the narrowed ureter under fluoroscopy (Figure 1A,1B). Two Allium stents were inserted in series after balloon dilatation.
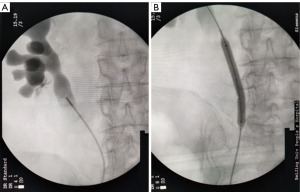
Then the right side was inspected and long segment stenosis below renal pelvis was confirmed by fluoroscopy. A stepwise dilation was conducted from renal pelvis downwards. Fluoroscopy confirmed that the stricture segment was dilated satisfactorily. However, when the balloon was pulled out of external urethral orifice, massive hemorrhage spurted out. And blood pressure dropped quickly, from 125/60 mmHg to 65/40 mmHg in about 5 min, even with the administration of positive vasoactive agents. Urgent arterial blood gases test revealed hemoglobin dropped to 7.2 g/dL from a preoperative basis of 13 g/dL. Intravenous infusion was accelerated and urgent blood transfusion was delivered. Cystoscopy found obvious hemorrhage flowing out from right ureteral orifice. The vascular surgeon was promptly requested for urgent consultation. A clinical diagnosis of UAF induced by balloon dilatation was made and angiography was suggested. However, another patient was concurrently under operation in the digital subtraction angiography room. Considering the instable hemodynamics, we made use of previous guide wire and inserted three Allium stents (30 F/12 cm) in series (Figure 2). Afterwards, hemorrhage subsided instantly and hemodynamic parameters gradually stabilized with blood pressure elevating to about 120/60 mmHg. The intraoperative blood loss reached 1,000 mL and the patient received 260 mL concentrated red blood cells.

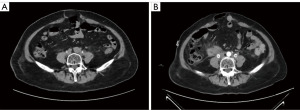
Postoperative enhanced abdominal pelvic computed tomography (CT) was performed, which suggested the relief of bilateral hydronephrosis. Additionally, a fresh hematoma (4.3 cm × 2.9 cm) was found in front of right ureter adjacent to the inferior margin of kidney, indirectly confirming the clinical diagnosis of UAF (Figure 3A,3B). The patients recovered uneventfully following surgery and was discharged after 7 days. The patient was followed up for 3 years without recurrent hematuria. Also, biliteral hydronephrosis was significantly alleviated. However, the patients finally had the stents removed and underwent ileal ureter replacement for recurrent urolithiasis and infection after 3 years.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
UAF is a relatively rare yet potentially life-threatening condition. It involves an abnormal connection between a ureter and an artery, typically the iliac artery. There has been a notable increase in reported cases of UAF due to the improvement of detection tools (1,2).
Risk factors for UAF include a history of pelvic irradiation, pelvic oncologic surgery and chronic indwelling ureteral stent (3). In addition, it was reported that UAF happened following vascular surgery performed on the iliac vessels (4). A potential mechanism of UAF is the adhesion of ureter and artery and their impaired wall. As to this case, the patient has history of pelvic irradiation, oncologic surgery and chronic ureteral stent. It needs to be emphasized that UAF occurred after balloon dilatation of the ureter with impaired wall. Thus, without dilatation or with dilatation under lower pressure, the fistula may have been prevented. It is thus imperative to stress that in patients at high risk of UAF, normal urologic procedure must be performed under extreme caution.
The typical initial presentation of UAF patients is hematuria, without accompanying symptoms, which frequently resolves without treatment (5). Despite guidelines indicating urological evaluation for hematuria, the lack of awareness about UAF often leads to delayed diagnosis. Hematuria is a common presentation of many different urological conditions (6), including but not limited to radiative cystitis, ureteral stent placement or urinary infection (7). Hence promptly identifying those patients at risk for UAF (e.g., pelvic surgery/radiation, indwelling stents etc.) is of clinical importance given the potential lethality of UAF.
The diagnosis of UAF remains difficult when there is clinical suspicion, as confirming this condition through various imaging tests can be difficult. A recent systematic review of 442 patients found angiography, the best diagnostic modality up to now, carried a sensitivity of 62%, and in 972 imaging tests of all kinds performed to diagnose UAF, only 46% effectively confirmed the presence of UAF (5). Considering the difficulty of diagnosis, proactive angiography is thus put forward, i.e., manipulation of ureteral stent or vascular catheter at the suspected UAF site during angiography, which theoretically has better sensitivity (8). However, proactive angiography could deteriorate hemorrhage and thus should only be performed under controlled circumstances.
Comparison with similar researches
Currently, endovascular repair with stent implantation, OSR, urologic approaches, and combination therapy are all treatment modalities for UAF. Traditionally, OSR, i.e., local reconstruction or ligation of the iliac artery with or without extra-anatomical bypass, was the standard treatment for UAF. However, since initial description of the procedure in 1996 (9), treatment paradigm has shifted towards less invasive endovascular repair. However, in the intraoperative scenario, the sudden occurrence of UAF still poses a huge challenge to urologist, especially when facing hemodynamic instability and lack of vascular surgeons. Under such condition, OSR is usually the only option, which is highly invasive and challenging in an emergency setting.
It was previously reported that a small amount of UAF patients was successfully treated by urologic approach, mainly through embolization of ureter. A 73-year-old female was treated by ultrasound-guided percutaneous nephrostomy and intraureteral multiple metallic coils insertion. She was free of further hemorrhage with perpetual left nephrostomy (10). Another 82-year-old woman with refractory, transfusion-dependent bleeding was treated with retrograde ureteral stump embolization using Tornado coils and a slurry of thrombin-soaked gelfoam, resulting in prompt resolution of hematuria. However, both procedures require the adequate occlusion of ureter, which significantly impair the physiological function of ureter and kidney (11).
Key findings
According to the case herein, Allium stent offers a real possibility for the intraureteral repair (IUR) of UAF.
Explanations of findings
The Allium ureteral stent is a self-expanding, large-caliber nitinol (nickel-titanium) stent. The stent is covered with a new biocompatible, biostable polymer, which prevents the ingrowth of surrounding structures and makes it non-permeable for fluids. The Allium comes in two caliber (24 F and 30 F) and in two lengths (10 and 12 cm). It has a main body with high radial force and soft end segment (Figure 4). It has shown good efficacy in some benign conditions such as post radiotherapy stricture, ureteroenteric anastomotic stricture after urinary diversion or post ureteroscopy stricture.

The substantial diameter and robust radial support force make it possible to successfully plug the leakage with IUR. Such procedure is easy to master in contrast to OSR. Its micro-invasiveness certainly surpasses OSR. It is time-saving against emergency scenario in comparison to OSR or endovascular repair, as the delay from re-cleansing, re-draping and position change are eliminated. It largely preserves the physiological function of ureter, unlike ureteral occlusion therapy. It could be administered during urologic operation by a urologist, rather a vascular surgeon or radiologist. This is meaningful especially in grass-root medical institutions like community hospitals. Moreover, for patients with primary ureteral stricture, primary disease could be simultaneously treated.
Strengths and limitations
In this case report, we present a patient suffering from intraoperative UAF who was successfully treated by ureteral stents placement. We provide details about the epidemiology, clinical diagnosis, treatment and prognosis of the disease. More importantly, we verify the effectiveness of Allium stent in the treatment of this rare and urgent disorder.
Implications and actions needed
Consequently, further in-depth studies are warranted to validate our experiences of the application of Allium stent in the treatment of UAF.
Conclusions
IUR with Allium stent could be a feasible treatment option for UAF, especially in an emergent setting.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-24-191/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-191/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-191/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- van den Bergh RC, Moll FL, de Vries JP, et al. Arterioureteral fistulas: unusual suspects-systematic review of 139 cases. Urology 2009;74:251-5. [Crossref] [PubMed]
- Omran S, Schäfer H, Kapahnke S, et al. Endovascular and open surgical options in the treatment of uretero-arterial fistulas. Vascular 2021;29:672-81. [Crossref] [PubMed]
- Fox JA, Krambeck A, McPhail EF, et al. Ureteroarterial fistula treatment with open surgery versus endovascular management: long-term outcomes. J Urol 2011;185:945-50. [Crossref] [PubMed]
- Ongaro L, Rizzo M, Claps F, et al. Arterioureteral fistula: An unusual cause of haematuria 10 years after the implantation of a synthetic iliac-femoral stent. Asian J Urol 2023;10:563-4. [Crossref] [PubMed]
- Kamphorst K, Lock TMTW, van den Bergh RCN, et al. Arterio-Ureteral Fistula: Systematic Review of 445 Patients. J Urol 2022;207:35-43. [Crossref] [PubMed]
- Khadhouri S, Gallagher KM, MacKenzie KR, et al. Developing a Diagnostic Multivariable Prediction Model for Urinary Tract Cancer in Patients Referred with Haematuria: Results from the IDENTIFY Collaborative Study. Eur Urol Focus 2022;8:1673-82. [Crossref] [PubMed]
- Bolenz C, Schröppel B, Eisenhardt A, et al. The Investigation of Hematuria. Dtsch Arztebl Int 2018;115:801-7. [PubMed]
- Yamasaki K, Omori K, Takaoka E, et al. Successful management by provocative angiography and endovascular stent of Ureteroarterial fistula in a patient with a long-term indwelling ureteral stent. Jpn J Clin Oncol 2010;40:267-70. [Crossref] [PubMed]
- Kerns DB, Darcy MD, Baumann DS, et al. Autologous vein-covered stent for the endovascular management of an iliac artery-ureteral fistula: case report and review of the literature. J Vasc Surg 1996;24:680-6. [Crossref] [PubMed]
- Inoue T, Hioki T, Arai Y, et al. Ureteroarterial fistula controlled by intraluminal ureteral occlusion. Int J Urol 2002;9:120-1. [Crossref] [PubMed]
- Jacobs BL, Maranchie JK. Embolization with Tornado coils to control bleeding from an arterioureteral fistula. Can J Urol 2007;14:3770-2. [PubMed]


