Comparison of laparoscopic and open cystectomy for bladder cancer: a single center of 110 cases report
Introduction
Radical cystectomy with lymph node dissection is the gold standard treatment for invasive and superficial high grade bladder tumors which have recurred after conservative treatment (1,2).
Radical cystectomy remains one of the most invasive surgical procedures in urology, with a mortality and complication rate of 1% to 2% and up to 25%, respectively (3,4). Historically, the first cystectomy was performed by Bernhard Bardenheuer (1839-1913) in January, 1887 in Koln, Germany. In 1949, Marshall and Whitmore gave the first detailed description of radical cystectomy (5). Progressively, the technique was improved and made safer. In the recent two decades, the use of laparoscopy to infiltrate bladder cancer has increased very rapidly. In 1992, Parra et al., published a case report on a laparoscopic cystectomy that was performed on a 27 year-old paraplegic woman with a pre-existing cutaneous diversion whose neurogenic bladder was removed for pyocystis (6). In 1993, Sanchez de Badajoz reported the first laparoscopic radical cystectomy for bladder cancer (7). In 2000, Gill published the first two cases of laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally (8). In 2004, Basillote et al. compared 13 laparoscopic cystectomies with 11 open cystectomies and found that there was no significant difference in operative time, blood loss and complications. However, there was a significant reduction in postoperative use of analgesics, time needed to regain fluid and solid intake, and hospital stay in the laparoscopic group (9). In 2007, Hernal et al. compared 30 laparoscopic cystectomies with 35 open cystectomies and found cystectomy using laparotomy was associated with a reduced use of analgesics and less blood loss (10). In 2009, Guillotreau et al. compared 38 laparoscopic cystectomies with 30 open cystectomies and found laparoscopic cystectomy was associated with a more rapid return to normal bowel function, less blood loss and low morbidity (11).
However, the series in these studies were small. In this study, we compare the operative time, rate of complications, blood loss, and hospital days of laparoscopic cystectomy vs. open cystectomy for bladder cancer.
Materials and methods
Between January 2004 and March 2011, we performed laparoscopic radical cystectomy in 45 patients with bladder cancer. Patients included 6 women and 39 men with a mean age of 59.7±11.1 yr. At the same time, we performed open radical cystectomy in 65 patients, which included 11 women and 54 men with a mean age of 64.6±9.3 yr. Before surgery all patients underwent a chest X-ray, cystoscope, ultrasound of the urologic system, and CT of the abdomen and pelvis.
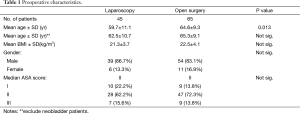
Preoperative parameters studied were patient age, body mass index, gender, ASA score. The details are presented in Table 1.
Full table
Statistical analysis
Quantitative values were compared with Student's t-test. Qualitative values were compared using the chi-square test or Fisher's exact test and P<0.05 was considered statistically significant. Statistical analysis was performed using SPSS software, 2006, ver. 15.0 (SPSS Institute).
Results
Preoperative characteristics are shown in Table 1. The groups were comparable in terms of sex, BMI, and ASA score. The mean age is younger in the laparoscopy group than the open surgery group. However, because the neobladder patients are relatively young, when we excluded the neobladder patients, there was no significant difference between the two groups.
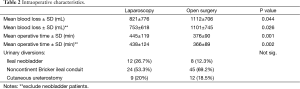
Intraoperative data is shown in Table 2. Operative time differed significantly between the 2 groups (LS group 445±119 min, Open surgery group 376±90 min, P<0.05). The operative time of open surgery group was less. However, total blood loss was significantly less in the LS group. According to the urinary diversions, the two groups are also comparable. Regardless of this, the number of neobladder patients in LS group was higher and neobladder patients were relatively younger than the rest of the patients in the group. Therefore, we also did a comparison of the two groups, excluding neobladder patients.
Full table
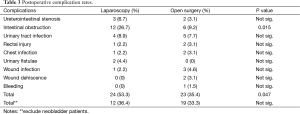
Postoperative complication rates are shown in Table 3. Except intestinal obstructions [LS group 12 (26.7%), Open surgery group 6 (9.2%), P=0.015], there was no significant difference between the two groups in postoperative complication rates.
Full table
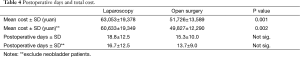
Postoperative days in hospital and total costs are shown in Table 4. Mean cost differed significantly between the 2 groups [LS group 63,053±19,378 yuan (about $10,000), Open surgery group 51,726±13,589 yuan (about $8200), P<0.05]. However, there was no significant difference between the two groups in postoperative days in hospital.
Full table
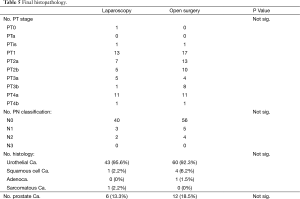
Histopathological details are shown in Table 5. Comparing the two groups with Fisher's exact test, no significant differences were found in pTNM stage, histology and occasional prostate cancer rates.
Full table
Discussion
The laparoscopic technique has been shown to provide significant benefits in various urological procedures (11). The laparoscopic cystectomy is one of the most complex surgical procedures in urology. In recent years, laparoscopic cystectomy has progressed very rapidly. However, there are limited studies comparing laparoscopic cystectomy with open cystectomy, and most series in these studies were small (4,9-12). The results in these studies indicate that blood loss and postoperative complication rates appear to be less after laparoscopic cystectomy compared to open surgery. But the results are not consistent.
In this study we compared the operative time, rate of complications, blood loss, and hospital days of laparoscopic cystectomy vs. open cystectomy for bladder cancer. Our study indicates that Laparoscopic cystectomy can reduce intraoperative blood loss significantly. Similarly, Hernal et al. determined that performing cystectomy via laparotomy was associated with less blood loss (10). The operative time of laparoscopic cystectomy is longer than the open surgery (LS group 445±119 min, Open surgery group 376±90 min). But Basillote et al. compared 13 laparoscopic cystectomies with 11 open cystectomies and found no significant difference in operative time (9). However, it is certainly likely that with further experience, our operative time will decrease further. Laparoscopic cystectomy initially appeared to have higher complication rates than open surgerydue to the inclusion of neobladder patients, who are typically associated with higher intestinal obstruction rates. No significant differences are found between the two groups when these patients are excluded. In addition, wound infection and wound dehiscence are lower in the LS group than in the open group (2.2% vs. 7.7%), although there is no statistically significant difference. Therefore, laparoscopic cystectomy is at least not associated with higher complication rates than open surgery and may even be improved with further experience.
About the hospital day, our data is much different from other studies. In our study, the mean hospital day is about 15 days. But in the study of Ashok K. Hemal et al., the mean hospital day is about 10 days (10). The most possible reason is that in China, the bed-fee (the cost of a patient stay in hospital for one day) is much cheaper (less than 50 yuan, about 8 $/d) than in the U.S. or Euro, so the patients in China are expected to want to stay in the hospital for a longer period of time.
As for the final histopathology, we found that there was no significant difference in pTNM stage, histology and occasional prostate cancer rates. It indicates the two groups are comparable, especially important for further oncologic outcome research.
Conclusions
According to our study, we conclude that: Laparoscopic cystectomy can reduce intraoperative blood loss significantly. Open cystectomy requires less operative time and has a lower cost than laparoscopic cystectomy for bladder cancer. There is no statistically significant difference in postoperative complication rates in the hospital between the two groups.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Oosterlinck W, Lobel B, Jakse G, et al. Guidelines on bladder cancer. Eur Urol 2002;41:105-12. [PubMed]
- Stenzl A, Cowan NC, De Santis M, et al. The updated EAU guidelines on muscle-invasive and metastatic bladder cancer. Eur Urol 2009;55:815-25. [PubMed]
- Skinner DG, Crawford ED, Kaufman JJ. Complications of radical cystectomy for carcinoma of the bladder. J Urol 1980;123:640-3. [PubMed]
- Vordos D, Hoznek A, Gettman M, et al. Laparoscopic Cystectomy- Evolution of A New Technique. EAU Update Series 2005;3:147-55.
- Skinner DG. Technique of radical cystectomy. Urol Clin North Am 1981;8:353-66. [PubMed]
- Parra RO, Andrus CH, Jones JP, et al. Laparoscopic cystectomy: initial report on a new treatment for the retained bladder. J Urol 1992;148:1140-4. [PubMed]
- Sánchez de Badajoz E, Gallego Perales JL, Reche Rosado A, et al. Arch Esp Urol 1993;46:621-4. [Radical cystectomy and laparoscopic ileal conduit]. [PubMed]
- Gill IS, Fergany A, Klein EA, et al. Laparoscopic radical cystoprostatectomy with ileal conduit performed completely intracorporeally: the initial 2 cases. Urology 2000;56:26-9. [PubMed]
- Basillote JB, Abdelshehid C, Ahlering TE, et al. Laparoscopic assisted radical cystectomy with ileal neobladder: a comparison with the open approach. J Urol 2004;172:489-93. [PubMed]
- Hemal AK, Kolla SB. Comparison of laparoscopic and open radical cystoprostatectomy for localized bladder cancer with 3-year oncological followup: a single surgeon experience. J Urol 2007;178:2340-3. [PubMed]
- Guillotreau J, Gamé X, Mouzin M, et al. Radical cystectomy for bladder cancer: morbidity of laparoscopic versus open surgery. J Urol 2009;181:554-9. [PubMed]
- Jackson CL. Urologic laparoscopy. Surg Oncol Clin N Am 2001;10:571-8. [PubMed]


