
Genital masculinizing reconstruction for untreated intersex individuals in adulthood: a case report
Highlight box
Key findings
• Achieving penile straightening and lengthening is possible as an initial surgery in adulthood for Intersex patients.
What is known and what is new?
• Sex assignment and determination of gender are significant challenges both from societal and surgical considerations.
• The international recommendations and legislations regarding the management of intersex individuals are evolving to promote self-determination of gender prior to any surgery, leading to new surgical challenges: the surgical possibilities are not the same in adulthood as in childhood.
What is the implication, and what should change now?
• This case illustrates the feasibility of delayed masculinizing surgery in cases of severe congenital genital anomalies and its impact on sexual satisfaction.
Introduction
Background
“Intersex” is a term rooted in a binary framework of sex used in the medical context to describe individuals exhibiting congenital variations in the genitalia that deviate from typical norms (1). Androgen insensitivity syndrome (AIS) is a rare variation of sexual development affecting individuals with a 46,XY chromosomal pattern. Androgens and their receptors are critical for male development stages, including sexual differentiation, spermatogenesis, and gonadotropin regulation (2). AIS encompass a diverse range of phenotypes. In partial androgen insensitivity syndrome (PAIS), individuals may present with a normal male genital and reproductive system. However, they may also exhibit various anomalies such as micropenis, severe hypospadias, bifid scrotum, undescended testis, and infertility (3).
In contemporary times, the assignment of sex and determination of the appropriate gender in individuals born with genital ambiguity pose significant challenges, including issues of parental responsibility, medical liability, and the right to self-determination (4,5).
Following the International Consensus Conference on Intersex Management [2005], the deciding process on gender and sex assignment has evolved into a multifactorial approach, considering comprehensive data on various intersex conditions. In France, the 2021 Bioethics Law regulates the care of intersex children, advocating for delaying surgeries until the child can provide informed consent.
Rationale and knowledge gap
This new context introduces novel challenges for healthcare practitioners (6,7). It is crucial to highlight several key points: from a surgical standpoint, which reconstruction techniques can be deferred and at what age gender-affirming surgeries should be postponed, considering in both aesthetic and societal factors? Additionally, what legislations govern these interventions? Given the current trend of delaying surgeries, there is an opportunity to explore innovative surgical approaches aimed at optimizing outcomes. This is especially pertinent for the intricate process of genital masculinization, acknowledged as one of the most challenging aspects of these procedures.
Objective
To illustrate this debate, we present a case involving genital reconstruction and penile straightening without urethroplasty in an adult patient with late diagnosis of PAIS, who did not receive treatment during childhood. We present this case in accordance with the CARE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-24-450/rc).
Case presentation
A 30-year-old patient was born in Sub-Saharan Africa and assigned female at birth due to genital variation. Raised in a female social role, he developed gender dysphoria in adolescence regarding his gynecomastia and genitalia, and adopted a male identity. Although he was identified as a man attracted to women but he was unable to have penetrative sexual intercourse. Clinical examination revealed severe perineoscrotal hypospadias, a microphallus (6 cm stretched penile length), and ventral curvature during erection. The testes were normally sized and located in a bifid scrotum (Figure 1). Hormonal analysis showed increased plasma testosterone (>15 ng/mL, normal range =3 to 8.5 ng/mL) and follicle-stimulating hormone (FSH) levels (13.2 IU/L normal range =5 to 15 IU/L). The karyotype was 46,XY and genetic analysis identified a rare known heterozygous variant in the androgen receptor (gene: AR, transcript NM_000044, genotype c.2239G>A, p.Val747Meth) (8) confirming the diagnosis of PAIS. The patient’s spermogram was normal allowing for gamete cryopreservation.
The patient was evaluated by our multidisciplinary gender team, including a psychiatrist, endocrinologist, plastic surgeon, urologist, and reproductive biologist. Following his mastectomy, he expressed a desire for genital masculinization and was referred to our institution for surgery, which was covered by national health insurance.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Surgery
First, an antibiotic prophylaxis with cefazolin was administered. A complete degloving of the penis was performed, with an incision made behind the urethral meatus. The urethral plaque was released and transected to correct the penile curvature. An erection test was conducted using an intra-cavernous injection of saline solution, revealing a persistent residual curvature of 40 degrees. The penile length remained at 6 cm. The residual curvature was corrected by a cavernotomy with a double-Y albugineal incision on the ventral aspect of the penis after releasing the neurovascular bundlescover. The cavernotomy performed enables gentle dilation of the corpus cavernosum before the implantation of a 100D4 ZEPHYR® implant (Zephyr Surgical Implants, Geneva) for metoidioplasty. Subsequently, the implant was fixed to the tunica albuginea of the corpus cavernosum. As in Peyronie’s disease incision-patch surgery, a Surgisis® patch was used to cover the cavernotomy and secured with four simple continuous sutures with polydioxanone (PDS) 3/0 (Figure 2). The use of a heterologous graft (Surgisis®) in this case allows for the preservation of autologous tissue for skin coverage or future urethroplasty. This resulted in a 2-cm increase in penile length.
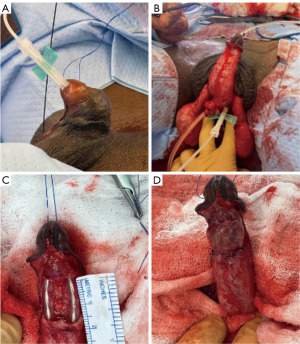
To achieve the skin coverage of the penile shaft, two scrotal flaps (8 cm × 3 cm) were harvested medially and sutured with interrupted stiches (9). A urethrostomy was performed at the peno-scrotal junction using separate VICRYL® 3/0 sutures. The two scrotal flaps were sutured along the penile shaft in two layers. Urinary and suprapubic catheters were left in place for 7 and 14 days, respectively, and a dressing was applied.
Due to the skin defect requiring the creation of two scrotal flaps, it was not possible to perform the urethroplasty during the same surgical session. A two-stage urethroplasty with a buccal mucosa graft will be performed for the urethral reconstruction.
Post-operative
The postoperative outcomes were uneventful and the patient was discharged after 4 days. At 6 months post-surgery, the patient achieved excellent results with no skin retraction or recurrent chordee. Starting from 3 months post-operatively, he was able to engage in satisfying frequent heterosexual intercourse without difficulty, reporting spontaneous erections with the prosthesis (Figure 3). After artificial insemination using his sperm collected after ejaculation, his partner became pregnant.
The modified EDITS (Erectile Dysfunction Inventory of Treatment Satisfaction) score [which is an EDITS without the question #5 and #6 (concern how quickly the treatment works and his duration)] was assessed at 30/36. The QoLSPP (quality of life and sexuality with penile prosthesis) score was assessed at 68/75 [question #2 was excluded (concerns three-piece prostheses)]. The patient reported satisfaction and continence with his urethrostomy and was considering future urethral reconstruction to urinate in standing position.
Discussion
Key findings
This case report illustrates the feasibility of delayed masculinizing surgery in adults with severe congenital genital anomalies, its safety and effectiveness in terms of patient satisfaction. This illustration is not intended to establish a general rule regarding the optimal age for performing surgery but aims to provide an example of the potential for delayed genital reconstruction and penile straightening in adulthood.
It should be emphasized that the surgical possibilities differ between childhood and adulthood. Specifically, incision-patch and scrotal flaps are not feasible in children, as they do not grow proportionately with age. The use of intra-cavernous implants proves effective in mitigating long-term tissue retraction and minimizing the risk of ventral curvature recurrence, especially in this case where vacuum therapy was not possible due to the small size and diameter of the penis. As the penile diameter did not allow for the placement of other implants, a 100 D4 ZEPHYR® implant for metoidioplasty was used. The main advantage of this type of penile prosthesis is that it enables spontaneous erections while maintaining sufficient penile rigidity, which facilitates sexual penetration and standing urination (after urethral reconstruction).
Strengths and limitations
Deciding on the most suitable timing for gender-affirming surgery in patients with PAIS raises numerous inquiries, including considerations about social acceptance and the impact of growing up with less conventional genitalia and, subsequently, gender identity. Other factors include determining the appropriate age for legal responsibility regarding non-vital surgeries and recognizing individual autonomy and self-determination. In this case report, our patient was raised as a girl in Africa and had never undergone genital surgery.
Comparison with similar research
Historically, gender assignment heavily relied on the visual assessment of genitalia. Decades ago, newborns with 46,XY variations in sex development used to be assigned female gender, accompanied by early gonadectomy and genital feminization surgery (10). Currently, there are not reports in the literature of masculinizing surgery in adult patients with PAIS. Apart from gonadal management, specific studies for PAIS in pediatric patients are limited (11).
In the contemporary context, some teams recently advocate postponing definitive procedures to allow the child to participate in the decision-making process, while others advocate early surgical intervention. No studies have ever demonstrated any advantages or drawbacks of early versus late genital surgery in children.
Implications and actions needed
From an epidemiological perspective, Babu’s 2021 meta-analysis reported a prevalence of gender incongruence in individuals with PAIS of 12% in those raised as female and 25% in those raised as male with no significant difference between the sex of rearing (12).
Furthermore, the sex assigned at birth appears to be a significant factor in the development of gender identity in adulthood (13). The primary goal of sex assignment should be alignment with the patient’s objectives, considering factors such as sociability, sexual satisfaction, and procreative capability. Minimal medical procedures, an overall gender-appropriate appearance, stable gender identity, and psychosocial well-being should also be considered (14).
In 2021, France implemented legal regulations for the management of intersex individuals, as outlined in Article 30 of the August 2, 2021, Bioethics Law (https://www.legifrance.gouv.fr/jorf/article_jo/JORFARTI000043884437). Following to its European neighbors and international recommendations (1,15) (Table 1), France bans unnecessary surgeries before a minor can provide informed consent.
Table 1
| Organization/country | Date | Legislative text | Text content | Child’s consent | Surgery age |
|---|---|---|---|---|---|
| Council of Europe | 2017/10 | Recommendations | Member states should end medically unnecessary “normalizing” treatments of intersex persons, including irreversible genital surgery and sterilization, when it is enforced or administered without the free and fully informed consent | Yes | Minor |
| Deferred until such time as the child is able to participate in the decision | |||||
| United Nations Committees | 2015 | Recommendations | Non-consensual gender-conforming interventions cut disturbingly across a vast array of human rights given that the victims are children who are targeted for invasive medical intervention because of their gender differences and perceived disabilities | Yes | Minor |
| World Health Organization (WHO) | 2015 | Recommendations | Irreversible invasive medical interventions should be postponed until a child is sufficiently mature to make an informed decision, so that they can participate in decision-making and give full, free, and informed consent | Yes | Minor |
| France | 2021/08 | Bioethics Law, Article 30 | Cases discussed in multidisciplinary teams meeting in reference centers. Consent from the minor must be systematically sought | Yes | Minor |
| Banned unnecessary surgeries prior minor can give his/her informed consent | |||||
| Germany | 2021/03 | Circular 19/24686 | Banned unnecessary surgeries. Surgical procedures must be approved by a family court except in the case of a vital threat | Yes | Minor |
| Parents can only authorize genital surgery if the intervention cannot be postponed until a later self-determined decision | |||||
| Greece | 2022/07 | Law no. 4958/2022, Articles 17 to 20 | Prohibit medical operations and procedures performed on intersex children. Can only be performed on intersex minors who have reached the age of 15 years. Case-by-case exceptions will be made in instances | Yes | >15 years |
| Malta | 2015/04 | Law of the Gender Identity, and Sex Characteristics Act | Prohibits sex assignment’s treatment/surgical intervention on the sexual characteristics of a minor that could be deferred when the minor is capable to provide informed consent | Yes | Minor |
| The minor gives informed consent through the person exercising parental authority or the tutor of the minor | |||||
| Portugal | 2018/08 | Law 38/2018 | Banned non-consensual treatment/surgeries on intersex children | Yes | Minor |
| Spain | 2023/02 | Trans Law | Banned unnecessary surgeries for children under 12 years. Older children can request to undergo surgery if wanted | Yes | >12 years |
We can observe that despite the earlier recommendations for legislation in 2015, European countries were slow to implement regulations regarding genital surgeries in intersex individuals. As for France, its legislation provides a framework for the management of these patients.
Conclusions
This report details an unprecedented case outlining the surgical management of masculinizing genital reconstruction in an adult patient with a late diagnosis of PAIS. To our knowledge, this description remains unpublished. The management of our patient demonstrates that delaying genital reconstruction surgery is possible. However, it raises important questions about the societal acceptability of intersex conditions during childhood and adolescence, as well as their own suffering.
Patient perspectives
This surgery has changed my life and enhanced my confidence to have sexual intercourses. I can now have penetrative sex, and my partner is pregnant. I’m very happy that I have had this surgery, and if I had to do it again, I would.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-24-450/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-24-450/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-24-450/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for the publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Coleman E, Radix AE, Bouman WP, et al. Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. Int J Transgend Health 2022;23:S1-S259. [Crossref] [PubMed]
- Krause W. Androgens in the demography of male life course--a review. Soc Biol 2006;53:4-12. [PubMed]
- Koçyiğit C, Sarıtaş S, Çatlı G, et al. A Novel Mutation in Human Androgen Receptor Gene Causing Partial Androgen Insensitivity Syndrome in a Patient Presenting with Gynecomastia at Puberty. J Clin Res Pediatr Endocrinol 2016;8:232-5. [Crossref] [PubMed]
- Mouriquand PD, Gorduza DB, Gay CL, et al. Surgery in disorders of sex development (DSD) with a gender issue: If (why), when, and how? J Pediatr Urol 2016;12:139-49. [Crossref] [PubMed]
- Fisher AD, Ristori J, Fanni E, et al. Gender identity, gender assignment and reassignment in individuals with disorders of sex development: a major of dilemma. J Endocrinol Invest 2016;39:1207-24. [Crossref] [PubMed]
- Weidler EM, Grimsby G, Garvey EM, et al. Evolving indications for surgical intervention in patients with differences/disorders of sex development: Implications of deferred reconstruction. Semin Pediatr Surg 2020;29:150929. [Crossref] [PubMed]
- Ehua AM, Moulot MO, Agbara KS, et al. Disorders of sex development: Challenges in a low-resource country. Arch Pediatr 2023;30:10-3. [Crossref] [PubMed]
- Matias PM, Donner P, Coelho R, et al. Structural evidence for ligand specificity in the binding domain of the human androgen receptor. Implications for pathogenic gene mutations. J Biol Chem 2000;275:26164-71. [Crossref] [PubMed]
- Mendel L, Neuville P, Allepot K, et al. Bilateral Pedicled Scrotal Flaps as an Alternative to Skin Graft in Penile Shaft Defects Repair. Urology 2023;176:206-12. [Crossref] [PubMed]
- Zucker KJ. Evaluation of sex- and gender-assignment decisions in patients with physical intersex conditions: a methodological and statistical note. J Sex Marital Ther 2002;28:269-74. [Crossref] [PubMed]
- Mansour M, Raya M, Jrdy AA, et al. Urethral reconstruction using amniotic membrane allograft in hereditary androgen insensitivity syndrome: a case series. J Surg Case Rep 2023;2023:rjad652. [Crossref] [PubMed]
- Babu R, Shah U. Gender identity disorder (GID) in adolescents and adults with differences of sex development (DSD): A systematic review and meta-analysis. J Pediatr Urol 2021;17:39-47. [Crossref] [PubMed]
- Callens N, Van Kuyk M, van Kuppenveld JH, et al. Recalled and current gender role behavior, gender identity and sexual orientation in adults with Disorders/Differences of Sex Development. Horm Behav 2016;86:8-20. [Crossref] [PubMed]
- Raveenthiran V. Neonatal Sex Assignment in Disorders of Sex Development: A Philosophical Introspection. J Neonatal Surg 2017;6:58. [Crossref] [PubMed]
- Garland J, Slokenberga S. Protecting the Rights of Children with Intersex Conditions from Nonconsensual Gender-Conforming Medical Interventions: The View from Europe. Med Law Rev 2019;27:482-508. [Crossref] [PubMed]




