
Tracking and analysis of benign prostatic hyperplasia and prostate cancer burden globally: 1990–2021 epidemiological trends
Highlight box
Key findings
• Global incidence of benign prostatic hyperplasia (BPH) and prostate cancer (PCa) surged by 115.23% and 161.66% (1990–2021), driven by aging populations.
• PCa-related mortality and disability-adjusted life-years (DALYs) declined (age-standardized rates), yet incidence remained stable.
• Geographical disparities: highest BPH burden in Eastern Europe and Asia; PCa concentrated in high-income North America and Australasia.
• Age-specific peaks: BPH (65–69 years); PCa (≥85 years).
• Smoking-related PCa DALYs decreased annually, signaling successful prevention.
What is known and what is new?
• Known: BPH and PCa are major aging-related conditions, but prior studies lacked global longitudinal comparisons and recent data.
• New: this study analyzes 1990–2021 global data to reveal sociodemographic drivers of BPH and PCa burdens, including age-region disparities and smoking’s evolving role.
What is the implication, and what should change now?
• Prioritize region-specific strategies: allocate resources to high-burden regions (e.g., BPH in Eastern Europe and Asia; PCa in high-income North America and Australasia).
• Strengthen early detection: capitalize on declining PCa mortality by expanding screening in underserved areas.
• Research non-smoking drivers: investigate metabolic syndromes and genetic factors associated with PCa to address the residual burden.
Introduction
Benign prostatic hyperplasia (BPH) stands as the predominant benign condition responsible for urinary difficulties among middle-aged and elderly males. Characterized by the anatomical enlargement, proliferation of prostate epithelial and stromal cells, this condition frequently results in bladder outlet obstruction and compression, ultimately causing lower urinary tract symptoms (LUTS) (1). A comprehensive review and meta-analysis encompassing 32 studies from 25 countries has revealed that the lifetime prevalence of BPH is estimated at 26.20%, with a 95% confidence interval (CI) ranging from 22.80% to 29.60% (2). Prostate cancer (PCa) is recognized as the most prevalent malignancy affecting the male urogenital system. The latest GLOBOCAN statistics from the World Health Organization in 2018 revealed that PCa occupies the second position in terms of male malignancy incidence globally, narrowly trailing lung cancer (3). Ample evidence indicates that the burden of BPH and PCa varies significantly across the globe (4,5), potentially attributed to regional differences in risk factors among populations, access to healthcare, and varying screening and diagnostic practices within different healthcare systems.
Given the aging of the population, socio-economic development, and advancements in disease prevention and management, there are likely to be certain changes in the spectrum and burden of diseases. However, to our knowledge, there is still a lack of up-to-date and comprehensive epidemiological data on simultaneously tracking and analyzing the two common prostatic diseases, BPH and PCa. Previous studies have primarily focused on describing the burden of either BPH or PCa individually (4,6,7), or the burden of BPH in relation to other benign urological diseases (8), without analyzing the differences in incidence rates and disability-adjusted life-years (DALYs) across different age groups. Additionally, some of these studies have limited their comparisons to the disease burden between only two regions or countries (7,9), potentially overlooking the global variability and complexity of these prostatic conditions. The present study aims to address this gap in knowledge.
The Global Burden of Disease Study 2021 (GBD 2021) serves as a crucial source of information and guidance for informed health policy decisions, quantifying the health impacts of various diseases, injuries, and risk factors. The epidemiological statistics derived from the regularly updated GBD dataset could provide valuable insights to policymakers in diverse countries and territories worldwide, facilitating in the improvement of public health. In this study, we utilized the GBD 2021 dataset to reveal the epidemiological patterns and burden of BPH and PCa over the past 32 years, considering multiple dimensions like global trends, regional and national variations, age groups, sociodemographic index (SDI), and human development index (HDI). Furthermore, we analyzed the risk factors attributable to PCa from 1990 to 2021, aiming for a comprehensive understanding of its epidemiology. We present this article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-2025-12/rc).
Methods
Data source and evaluation indicators
This study utilized the extensive data from the GBD 2021 database, which conducted a comprehensive analysis of the incidence, age-standardized rates (ASR), and DALYs for 371 diseases and injuries across various age and sex groups in 204 different countries and territories globally. The Global Health Data Exchange GBD Results Tool (http://ghdx.healthdata.org/) was utilized to retrieve the incidence and DALYs of both BPH and PCa, along with their corresponding ASR and 95% uncertainty intervals (UI). DALYs, a standard metric for quantifying the burden of diseases, are derived by summing the years of life lost (YLL) and years lived with disability (YLD) (10,11).
The SDI, a composite measure of development status, demonstrates a robust correlation with health outcomes. It spans a range from 0 to 1, with 1 indicating the utmost level of development and 0 representing the lowest level of development. Based on their SDI quintiles, the 21 global geographic regions were classified into five distinct categories: low (<0.45), low-middle (≥0.45 and<0.61), middle (≥0.61 and <0.69), high-middle (≥0.69 and <0.80), and high (≥0.80) (12). This classification provided a nuanced understanding of the varying development levels across the globe. Age was segmented into seventeen distinct categories: 0–4, 5–9, 10–14, 15–19, 20–24, 25–29, 30–34, 35–39, 40–44, 45–49, 50–54, 55–59, 60–64, 65–69, 70–74, 75–79, 80–84 and over 85 years of age. Detailed data sources and modeling methodologies were comprehensively outlined in GBD 2021 (13).
The HDI is a comprehensive measure encompassing life expectancy, living standards, and education (14). It integrates economic and social indicators to indicate imbalances between economic growth and societal progress. Additionally, it underscores the all-round development of individuals, including health, education, living conditions, environmental well-being, and personal liberties. The HDI serves as a crucial indicator of a country’s overall national strength and can be accessed via the World Bank’s website (http://hdr.undp.org/en/content/human-development-index-hdi/). To investigate the factors influencing EAPCs, we assessed the relationship between EAPC and ASRs in 1990 and HDI in 2021 at the national level using scatter plots and Pearson correlation analysis.
The assessment of GBD risk factors follows a comprehensive seven-step comparative risk evaluation framework, which has been extensively described in previous publications (13). In the analysis, the risk factors for PCa encompassed smoking, which references previously published researches (15). The deaths and DALYs pertaining to PCa are accessible through the GBD 2021 results tool. In addition, we utilized joinpoint regression analysis program (version 5.1.0) to identify global temporal trends in age-standardized DALY rates (ASDR) and age-standardized mortality rates (ASMR) for the risk factor of smoking in PCa patients from 1990 to 2021. The annual average percentage change (AAPC) was calculated as the geometric mean of the annual percentage change (APC) values. The detailed methodology is available in prior literature (9).
To minimize bias arising from variations in data availability and quality across countries, the GBD study utilizes standardized data collection and validation methods, supplemented by predictive statistical modeling for regions with sparse data. These measures ensure robust and comparable burden estimates globally (10). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Statistical analysis
The ASR (per 100,000 population) was calculated by summing the products of age-specific rates (ai, i representing the rate for the ith age group) and the population counts (or weight wi) within each corresponding age group i of the designated reference standard population. Subsequently, this sum was normalized by dividing it by the aggregate sum of the standard population weights: . To evaluate the temporal trend of ASR within a specified time frame, we employed the estimated annual percentage changes (EAPC). Given that the natural logarithm of ASR exhibits a linear relationship with time, we estimated the EAPC using a linear regression model: y = α + βx + ε, where y represents ln (ASR), x denotes the calendar year, and ε accounts for the error term. The EAPC was computed as 100 × (exp(β) − 1), and its corresponding 95% CI: was derived from the linear regression model. If both the estimated EAPC value and its lower 95% CI: exceed 0, it indicates an upward trend in ASR. Conversely, if both the estimated EAPC value and its upper 95% CI are less than 0, it signifies a downward trend in ASR. Statistical analysis and data visualization were conducted utilizing R software (version 4.1.2). P value <0.05 was deemed statistically significant.
Results
Global incidence, mortality, and DALYs for BPH and PCa
In 2021, globally, there were 6,406,000 incident cases of BPH (95% UI: 50.00 to 79.95) and 506,000 incident cases of PCa (95% UI: 4.81 to 5.25). Compared to 1990, incident cases of BPH and PCa increased by 115.23% and 161.66%, respectively. PCa caused 432,000 deaths (95% UI: 3.82 to 4.64) globally in 2021, which is 2.04 times higher than in 1990. The DALYs for BPH and PCa were 2,236,000 (95% UI: 13.46 to 34.03) and 8,142,000 (95% UI: 71.77 to 88.09), respectively, representing increases of 2.21 and 1.96 times compared to 1990. The age-standardized incidence rate (ASIR) of PCa increased from 32.64/100,000 population (95% UI: 30.86 to 33.86) in 1990 to 34.05/100,000 population (95% UI: 31.27 to 36.00) in 2021. In contrast, the ASDR decreased from 275.66/100,000 population (95% UI: 251.66 to 292.14) in 1990 to 217.83/100,000 population (95% UI: 192.65 to 235.53) in 2021, while the ASMR fell from 16.35/100,000 population (95% UI: 15.02 to 17.28) in 1990 to 12.63/100,000 population (95% UI: 11.16 to 13.55) in 2021. For BPH, from 1990 to 2021, both ASIR and ASDR have declined to a certain extent. Overall, the EAPC of ASIR for BPH was 0.03 (95% CI: −0.02 to 0.08), and for PCa, it was −0.06 (95% CI: −0.20 to 0.08). Therefore, the ASIR for both diseases did not show significant changes over the study period. Additionally, the ASMR and ASDR of PCa demonstrated a decreasing trend (EAPC: −1.05, 95% CI: −1.14 to −0.95; −0.96, 95% CI: −1.05 to −0.88). Moreover, the ASDR of BPH showed no significant trend with an EAPC of 0 (95% CI: −0.05 to 0.05) (Table 1). Generally, over the past 32 years, there had been a significant decline in the ASDR and ASMR for PCa, with the notable decrease occurring between 1994 and 2013 (Figure 1).
Table 1
| Disease burden and outcomes | BPH | PCa |
|---|---|---|
| 1990† | ||
| Incident case (×100,000) | 64.06 (50.00 to 79.95) | 5.06 (4.81 to 5.25) |
| Deaths (×100,000) | – | 2.12 (1.94 to 2.24) |
| DALYs (×100,000) | 10.11 (6.06 to 15.56) | 41.47 (37.54 to 44.02) |
| ASIR | 335.00 (262.28 to 414.7) | 32.64 (30.86 to 33.86) |
| ASMR | – | 16.35 (15.02 to 17.28) |
| ASDR | 57.48 (34.56 to 87.77) | 275.3 (251.66 to 292.14) |
| 2021† | ||
| Incident case (×100,000) | 137.88 (109.08 to 170.15) | 13.24 (12.17 to14.00) |
| Deaths (×100,000) | – | 4.32 (3.82 to 4.64) |
| DALYs (×100,000) | 22.36 (13.46 to 34.03) | 81.42 (71.77 to 88.09) |
| ASIR | 326.12 (258.88 to 400.32) | 34.05 (31.27 to 36.00) |
| ASMR | – | 12.63 (11.16 to 13.55) |
| ASDR | 55.12 (33.21 to 83.48) | 217.83 (192.65 to 235.53) |
| 1990–2021‡ | ||
| Incident case (%) | 115.23 | 161.66 |
| Deaths (%) | – | 103.77 |
| DALYs (%) | 121.17 | 96.33 |
| ASIR (EAPC, 95% CI) | 0.03 (−0.02 to 0.08) | −0.06 (−0.20 to 0.08) |
| ASMR (EAPC, 95% CI) | – | −1.05 (−1.14 to −0.95) |
| ASDR (EAPC, 95% CI) | 0 (−0.05 to 0.05) | −0.96 (−1.05 to −0.88) |
†, all data are reported as numbers or rates (per 100,000 persons with 95% uncertainty intervals); ‡, percentage represents the change in cases; EAPC represents the change in rates. ASIR, age-standardized incidence rate; ASMR, age-standardized mortality rate; ASDR, age-standardized DALYs rate; BPH, benign prostatic hyperplasia; CI, confidence interval; DALYs, disability-adjusted life-years; EAPC, estimated annual percentage change; PCa, prostate cancer.

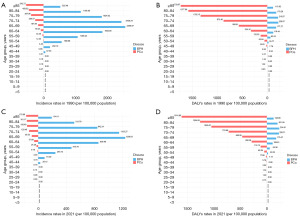
Globally, we also conducted an analysis of the incidence rates and DALYs rates associated with BPH and PCa across various age cohorts in male patients, as depicted in Figure 2. In both 1990 and 2021, the age group with the highest incidence rates of BPH was 65–69 years, whereas for PCa, the incidence rates and DALYs rates continued to increase with age, peaking in the age group older than 85 years in both years.
Regional and national incidence, mortality, and DALYs for BPH and PCa
Overall, over the past 32 years, the EAPC of ASIR for both prostate diseases in most regions was above zero. Particularly for PCa, only high-income North America (EAPC =−1.25, 95% CI: −1.38 to −1.12) and Australasia (EAPC =−0.83, 95% CI: −1.47 to −0.19) had exhibited negative estimated EAPCs. The regions with the highest increases in ASIR for BPH patients were high-income North America, with EAPCs of 0.47 (95% CI: 0.38 to 0.56). For PCa, the regions with the highest EAPCs of ASIR were Eastern Europe (EAPC =3.27, 95% CI: 3.08 to 3.47). From 1990 to 2021, the regions with the largest increases in ASDR and ASMR for PCa were Eastern Europe, with EAPCs of 1.51 (95% CI: 1.41 to 1.60) and 1.48 (95% CI: 1.39 to 1.57), respectively. Additionally, high-income North America, Australasia and Western Europe showed the most significant decreasing trends in ASDR and ASMR for PCa (Table 2).
Table 2
| Geographic regions | EAPC of ASIR (95% CI) | EAPC of ASDR (95% CI) | EAPC of ASMR (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| BPH | PCa | BPH | PCa | PCa | |||
| Global | 0.03 (−0.02 to 0.08) | −0.06 (−0.20 to 0.08) | 0 (−0.05 to 0.05) | −0.96 (−1.05 to −0.88) | −1.05 (−1.14 to −0.95) | ||
| Andean Latin America | 0.18 (0.15 to 0.22) | 1.47 (1.33 to 1.62) | 0.14 (0.10 to 0.17) | −0.11 (−0.24 to 0.03) | −0.11 (−0.25 to 0.04) | ||
| Australasia | 0.10 (0 to 0.20) | −0.83 (−1.47 to −0.19) | 0.03 (0 to 0.07) | −2.67 (−3.05 to −2.29) | −2.74 (−3.06 to −2.43) | ||
| Caribbean | 0.21 (0.19 to 0.24) | 1.30 (1.11 to 1.50) | 0.17 (0.15 to 0.19) | 0.36 (0.21 to 0.51) | 0.21 (0.05 to 0.38) | ||
| Central Asia | 0.02 (−0.01 to 0.05) | 1.76 (1.43 to 2.09) | 0.05 (0.03 to 0.07) | 0.79 (0.55 to 1.02) | 1.03 (0.75 to 1.31) | ||
| Central Europe | −0.22 (−0.28 to −0.16) | 2.27 (2.04 to 2.49) | −0.13 (−0.23 to −0.02) | 0.49 (0.31 to 0.67) | 0.45 (0.25 to 0.64) | ||
| Central Latin America | 0.15 (0.12 to 0.18) | 1.43 (1.10 to 1.76) | 0.13 (0.10 to 0.16) | −0.22 (−0.43 to 0) | −0.31 (−0.54 to −0.09) | ||
| Central SubSaharan Africa | 0.03 (0.02 to 0.05) | 0.93 (0.77 to 1.09) | 0.06 (0.05 to 0.07) | 0.57 (0.45 to 0.70) | 0.64 (0.51 to 0.77) | ||
| East Asia | −0.21 (−0.35 to −0.06) | 1.93 (1.78 to 2.09) | −0.25 (−0.41 to −0.09) | −0.2 (−0.39 to −0.01) | −0.24 (−0.46 to −0.01) | ||
| Eastern Europe | −0.02 (−0.05 to 0.01) | 3.27 (3.08 to 3.47) | 0.02 (0 to 0.04) | 1.51 (1.41 to 1.60) | 1.48 (1.39 to 1.57) | ||
| Eastern SubSaharan Africa | 0.02 (0 to 0.03) | 0.59 (0.54 to 0.65) | 0.04 (0.02 to 0.05) | 0.18 (0.15 to 0.21) | 0.15 (0.12 to 0.19) | ||
| High-income Asia Pacifc | −0.08 (−0.18 to 0.01) | 2.35 (1.83 to 2.87) | −0.13 (−0.21 to −0.06) | 0 (−0.28 to 0.28) | −0.09 (−0.37 to 0.20) | ||
| High-income North America | 0.47 (0.38 to 0.56) | −1.25 (−1.38 to −1.12) | 0.2 (0.13 to 0.27) | −2.25 (−2.4 to −2.1) | −2.40 (−2.55 to −2.26) | ||
| North Africa and Middle East | 0.13 (0.12 to 0.14) | 2.81 (2.72 to 2.91) | 0.12 (0.11 to 0.13) | 0.51 (0.44 to 0.58) | 0.38 (0.30 to 0.46) | ||
| Oceania | 0.12 (0.10 to 0.13) | 0.76 (0.72 to 0.80) | 0.14 (0.13 to 0.16) | 0.53 (0.48 to 0.58) | 0.50 (0.44 to 0.55) | ||
| South Asia | 0.21 (0.16 to 0.25) | 0.97 (0.83 to 1.12) | 0.24 (0.21 to 0.27) | 0.08 (−0.06 to 0.22) | 0.21 (0.07 to 0.35) | ||
| Southeast Asia | −0.1 (−0.18 to −0.03) | 1.87 (1.81 to 1.93) | −0.12 (−0.21 to −0.02) | 0.81 (0.74 to 0.88) | 0.79 (0.71 to 0.88) | ||
| Southern Latin America | 0.38 (0.28 to 0.48) | 0.86 (0.48 to 1.24) | 0.33 (0.28 to 0.37) | −0.55 (−0.87 to −0.22) | −0.45 (−0.78 to −0.13) | ||
| Southern SubSaharan Africa | 0.11 (0.09 to 0.13) | 1.41 (1.27 to 1.55) | 0.10 (0.08 to 0.12) | 0.94 (0.73 to 1.14) | 0.89 (0.69 to 1.09) | ||
| Tropical Latin America | −0.25 (−0.36 to −0.14) | 0.95 (0.60 to 1.31) | −0.31 (−0.43 to −0.20) | −0.11 (−0.44 to 0.22) | −0.03 (−0.36 to 0.30) | ||
| Western Europe | 0.38 (0.25 to 0.50) | 0.41 (0.08 to 0.75) | 0.21 (0.18 to 0.24) | −1.68 (−1.82 to −1.55) | −1.85 (−1.99 to −1.72) | ||
| Western SubSaharan Africa | 0 (−0.01 to 0.01) | 1.25 (1.20 to 1.31) | 0.04 (0.03 to 0.05) | 0.80 (0.76 to 0.84) | 0.87 (0.83 to 0.92) | ||
ASIR, age-standardized incidence rate; ASDR, age-standardized DALYs rate; ASMR, age-standardized mortality rate; CI, confidence interval; BPH, benign prostatic hyperplasia; DALYs, disability-adjusted life-years; EAPC, estimated annual percentage change; PCa, prostate cancer.
As shown in the Figure 3, in 2021, the countries and territories with the highest and lowest ASIR for BPH were Lithuania (691.36/100,000 population) and South Korea (126.90/100,000 population), while the highest ASIR for PCa were observed in Bermuda (196.12/100,000 population). From 1990 to 2021, the highest increase in BPH cases was observed in the United Arab Emirates (1,505.30%). For PCa, the greatest increase in cases occurred in South Korea (1,620.90%). Regarding BPH, the largest increase in ASIR was observed in the Austria (EAPC =0.72). The greatest increase in ASIR of PCa was observed in South Korea (EAPC =4.35), while the most remarkable decrease was seen in Canada (EAPC =−2.22).

Burden of BPH and PCa by SDI
We analyzed the correlation between the ASIR of BPH and PCa and the level of SDI across 21 geographical regions. From 1990 to 2021, the overall ASIR of BPH decreased with increasing SDI (Figure 4A), whereas the ASIR of PCa increased with increasing SDI (Figure 4B). Our analysis revealed an M-shaped relationship between SDI and the ASIR and ASDR of BPH, especially in 2021 (Figure 4C,4D). At the regional level, the expected values showed two peaks at SDI values of around 0.45 and 0.72 for BPH, and one peak at approximately 0.82 for PCa. In 2021, our analysis demonstrated that the relationship between SDI and the ASIR, ASDR, and ASMR of PCa formed a W-shape (Figure 4E-4G). In 2021, the ASIR and ASDR of BPH in Eastern Europe, categorized as a high SDI region, stood as the highest, while the ASIR of PCA in both high-income North America, belonging to the high SDI level, reached its peak. For PCa in 2021, the Southern Sub-Saharan Africa region, which was classified as middle SDI, exhibited the highest ASDR and ASMR.

Factors influencing the EAPC of BPH and PCa
We examined the relationships between EAPCs and ASRs in 1990, as well as HDI in 2021, across 204 countries or territories. Regarding BPH and PCa, a significant negative association was observed between the ASIR in 1990 and EAPCs (ρBPH=−0.28, P<0.001; ρPCa=−0.46, P<0.001) (Figure 5A). Additionally, our analysis showed a significant positive correlation between HDI in 2021 and EAPCs for BPH, including ASIR (ρ=0.39, P<0.001) and ASDR (ρ=0.26, P<0.001) (Figure 5B). For PCa, a significant negative correlation was observed between HDI in 2021 and EAPCs of ASDR (ρ=−0.53, P<0.001), while no correlation was found for ASIR (ρ=−0.09, P=0.22) (Figure 5C).

Attributable risk factors for PCa
Figure 6 illustrates that, globally, the ASDR and ASMR for PCa attributed to smoking had been declining in most regions over the past 32 years, with the fastest decline occurring between 1994 and 2013. Compared to 1990, the DALYs rate and death rate for PCa patients attributable to smoking have significantly decreased across all age groups by 2021. The age group of 75–79 years exhibited the most significant decline in DALYs rate for PCa, with a reduction of 53.49%. Additionally, patients aged 65–69 years experienced the greatest decrease in death rate, showing a decline of 49.30%. From 1990 to 2021, Australasia experienced the highest percentage declines in ASDR and ASMR attributed to smoking-related PCa, with reductions of 70% and 71.92%, respectively.

Discussion
This study utilized the latest GBD 2021 data to conduct the first comprehensive assessment of the estimated burden and trends of BPH and PCa at global, regional, and national levels from 1990 to 2021. Over the past 32 years, our study has identified a significant increase in global incident cases, deaths, and DALYs associated with these two common urological conditions among elderly males. The LUTS caused by BPH impose a substantial burden on elderly men, significantly diminishing their quality of life, while advanced PCa poses a more fatal threat to patients. However, uneven distribution of medical resources in underdeveloped regions remains a vexing issue, encompassing inadequate diagnosis and treatment as well as an imbalance ratio of urologists to patients. In this study, we have separately examined the global burden of BPH and PCa, providing evidence to inform targeted healthcare policy formulation and medical resource allocation in the future.
Our results showed that the incidence of BPH remained much higher than those of PCa, and the ASIR showed a relatively stable trend over past 32 years. The global population aging and increased life expectancy may be reasons for the rising absolute disease burden of BPH (4). Compared to 1990, despite the increase in the absolute burden of BPH (incidence and DALYs) in 2021, the relative burden (ASIR and ASDR) has decreased. This likely reflects the impact of population growth and aging globally, while also indicating that improvements in healthcare have effectively reduced the burden of BPH across all age groups. Overall, the decreasing trends in ASDR, and ASMR of PCa (EPAC =−0.96; −1.05) over the past 32 years suggested significant impacts from advances in medical imaging technologies, screening criteria, radiation and endocrine therapy methods, as well as increased public health awareness in reducing the relative burden of PCa (16-18). We found that from 1990 to 2021, regions with high SDI (such as high-income North America and Australasia) consistently had markedly higher annual ASIRs for PCa compared to other regions. This is likely due to the expanded prostate-specific antigen (PSA) screening initiatives that started in developed countries in the 1990s (19). Despite the extensive use of PSA screening, the current method for detecting PCa has led to overdiagnosis, overtreatment of low-risk cases, and the underdiagnosis of clinically significant cases (20). Therefore, high-precision and non-invasive monitoring and early detection methods for PCa, including artificial intelligence (AI) diagnostic models, are becoming increasingly popular research topics (21).
Overall, the broader and superior healthcare systems and medical resources in high-income regions, along with a higher level of health consciousness among their citizens who regularly undergo health checks, have resulted in relatively lower ASDR and ASMR for PCa (5), as well as lower ASDR for BPH, compared to other regions. For BPH, North Africa and Middle East recorded the most significant increase in cases, while Eastern Europe had the highest ASIR and ASDR. High-income North America had the highest EAPC of ASIR for BPH, while Southern Latin America (one of middle-SDI regions) had the highest EAPC of ASDR. In some low-SDI regions, the ASIR is relatively low, possibly due to a significant number of potential BPH and PCa patients not seeking timely medical care due to economic constraints. Additionally, the higher ASDR and ASMR in underdeveloped areas indicate that the healthcare systems in these regions are less advanced, with many patients unable to receive adequate treatment and support (8,15). Thus, developing AI-assisted medical systems and online clinic services, along with collaborating with international medical institutions and non-governmental organizations to introduce advanced medical technologies and expertise, are effective measures to provide underdeveloped regions with direct access to external medical resources, promoting universal health coverage.
Notably, although South Korea’s ASIR for PCa in 2021 is not among the highest compared to most other countries, its EAPC of ASIR is the highest among 204 countries and territories, at 4.35. Additionally, the increase in incident cases in 2021 compared to 1990 was the second highest globally, with a 1,620.90% increase. This indicates a rapidly rising trend in PCa incidence in South Korea, suggesting that the country may face a significant increase in the burden of PCa in the near future. Facing the projected increase in PCa cases and the strain it may impose on South Korea’s healthcare infrastructure, augmenting screening and prevention strategies is a vital step towards mitigation. An epidemiological study from 2007 to 2013 also supported our aforementioned conclusion, suggesting that the increasing incidence of PCa in South Korea may be attributed to population aging and the westernization of dietary habits (22).
The GBD methodology employs rigorous data validation and estimation techniques to minimize reporting inconsistencies across years and countries. However, national estimates may still be influenced by changes in healthcare policies, screening practices, or reporting systems. Despite the extreme increases or decreases in ASIR observed in some countries, their overall trends remained within the range of their respective geographic regions. This suggests that regional patterns continue to provide a robust framework for understanding the burden of prostate diseases.
In both 1990 and 2021, the incidence rates and DALY rates of PCa across all age groups showed a downward trend globally. This trend may be attributed to improvements in healthcare and increased public awareness of the disease, leading to earlier detection and treatment of PCa. The clinical prevalence of BPH in men over 50 years old ranges from 50% to 75%, and this figure increases with age, exceeding 80% in men over 70 years old (23). In line with previous studies, we observed that the DALYs rate for BPH rose with age but declined in patients over 80 (8). This suggested that most BPH patients may underwent medical or surgical treatment in the early stages, leading to improved or controlled LUTS symptoms, thereby reducing the DALYs in the over-80 age group compared to those under 80 years.
For BPH, a significant positive correlation was observed between the HDI in 2021 and the EAPCs for ASIR and ASDR, indicating that countries with higher HDI experienced a faster increase in the ASRs of BPH. We inferred that this was due to these countries having more advanced medical detection and reporting systems, which could more effectively diagnose and record a greater number of cases. Besides, our results exhibited that in countries with higher HDI, although the rate of increase in the ASIR of PCa did not show significant change, the rate of increase in ASDR was lower. This might reflect advancements in the treatment and management of PCa in these countries, which could lead to an improved quality of life. Previous reports also supported our conclusion (24). Therefore, countries with varying levels of HDI, particularly underdeveloped and developing nations, need to develop tailored PCa prevention and management strategies that align with their available healthcare infrastructure.
Consistent with previous studies, smoking has been identified as a major risk factor for PCa (15,25). Over the past 32 years, global efforts to control tobacco use have resulted in a decline in both PCa-related deaths and DALYs, particularly in high-SDI regions such as Australasia, high-income North America, and Western Europe. We also observed that smoking has a greater impact on older PCa patients. As age increases, smoking leads to higher DALYs and mortality rates, possibly due to older patients experiencing more or more severe comorbidities such as chronic obstructive pulmonary disease resulting from long-term smoking (26). While we acknowledge that modifying lifestyle habits such as smoking and secondhand smoke exposure can be challenging for some patients, it is crucial to recognize their potential influence on PCa advancement. A review indicated that modifying factors like diet and lifestyle after PCa diagnosis are associated with rates of recurrence, progression, and mortality (27). The study highlighted increased risks of PCa recurrence and death linked to smoking and consumption of whole-fat milk/high-fat dairy products. In contrast, regular physical exercise and consuming half to one glass of red wine per day were linked with reduced PCa-specific mortality and risks of recurrence. Therefore, there is still a long way to go in reducing tobacco consumption and preventing malignant tumor. Countries should implement more tobacco control policies and smoking cessation education, especially for the potential youth smokers, as cigarette use continues to prevail among this demographic across many countries (15). Racial and ethnic differences have been widely recognized as important factors in prostate cancer risk, with individuals of African ancestry exhibiting a higher incidence (28,29). However, the GBD database does not provide race-specific data, as its estimates rely on national and regional disease burden models rather than individual-level racial classifications (13). While geographical trends may partly reflect racial disparities in prostate cancer burden, direct conclusions regarding racial influences cannot be drawn from GBD estimates. Future studies incorporating race-specific data could offer a more comprehensive understanding of the interplay between genetic and environmental risk factors in prostate cancer epidemiology.
During a pandemic, such as the challenging coronavirus disease 2019 (COVID-19) outbreak, there can be changes in the delivery of clinical services, particularly in the screening, diagnosis, and intervention of malignant tumors, potentially leading to missed opportunities for timely detection and optimal treatment (30). In England alone, this epidemic resulted in approximately 20,000 missed cases of PCa. Throughout the entire pandemic period, the incidence of PCa remained lower than anticipated (31). A study indicated that patients with PCa are more sensitive to COVID-19-related pathogenesis, leading to higher hospitalization and mortality rates. Compared to COVID-19 patients with other genitourinary cancers, those with PCa experienced higher rates of hospitalization and mortality (32). This suggested that mortality rates and DALYs for PCa patients during 2020–2021 might have been overestimated.
Despite using the most updated epidemiological data and comprehensively analyzing the burden of BPH and PCa across diverse regions and countries worldwide, there are several limitations in this study. Firstly, the GBD data sources are constrained and do not encompass all geographic regions or populations, therefore they only offer a broad overview for certain locations. Secondly, inconsistencies in diagnostic criteria, detection techniques, and oversight frameworks across regions with varying degrees of development lead to uneven data quality. Furthermore, the risk factors for PCa considered in the GBD 2021 are restricted and do not fully capture the entire spectrum of disease etiologies. While the GBD database provides a reliable estimation of BPH and PCa incidence, it is important to note that there could be potential underreporting or discrepancies in regions with limited health infrastructure or where cancer registration systems are less established. Additionally, the model adjustments used to estimate missing data may introduce some level of uncertainty.
Conclusions
BPH and PCa remain significant global health issues due to their increasing absolute burden, despite BPH’s stable relative burden and the declining trend in PCa. Strategic allocation of medical resources across regions and countries, considering epidemiological features and geographical distributions, remains imperative. Additionally, enhancing access to effective treatments and increasing the number of trained healthcare professionals in developing and underdeveloped regions could be the next significant milestones.
Acknowledgments
The authors appreciate the works by the Global Burden of Disease Study 2021 collaborators.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-2025-12/rc
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-2025-12/prf
Funding: This study was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-2025-12/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tang X, Liu Z, Ren J, et al. Comparative RNA-sequencing analysis of the prostate in a mouse model of benign prostatic hyperplasia with bladder outlet obstruction. Mol Cell Biochem 2023;478:2721-37. [Crossref] [PubMed]
- Lee SWH, Chan EMC, Lai YK. The global burden of lower urinary tract symptoms suggestive of benign prostatic hyperplasia: A systematic review and meta-analysis. Sci Rep 2017;7:7984. [Crossref] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- The global, regional, and national burden of benign prostatic hyperplasia in 204 countries and territories from 2000 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Healthy Longev 2022;3:e754-76. [Crossref] [PubMed]
- Culp MB, Soerjomataram I, Efstathiou JA, et al. Recent Global Patterns in Prostate Cancer Incidence and Mortality Rates. Eur Urol 2020;77:38-52. [Crossref] [PubMed]
- Launer BM, McVary KT, Ricke WA, et al. The rising worldwide impact of benign prostatic hyperplasia. BJU Int 2021;127:722-8. [Crossref] [PubMed]
- Abbasi-Kangevari M, Saeedi Moghaddam S, Ghamari SH, et al. The burden of prostate cancer in North Africa and Middle East, 1990-2019: Findings from the global burden of disease study. Front Oncol 2022;12:961086. [Crossref] [PubMed]
- Zhu C, Wang DQ, Zi H, et al. Epidemiological trends of urinary tract infections, urolithiasis and benign prostatic hyperplasia in 203 countries and territories from 1990 to 2019. Mil Med Res 2021;8:64. [Crossref] [PubMed]
- Liu D, Li C, Li Y, et al. Benign prostatic hyperplasia burden comparison between China and United States based on the Global Burden of Disease Study 2019. World J Urol 2023;41:3629-34. [Crossref] [PubMed]
- Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020;396:1204-22. [Crossref] [PubMed]
- Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024;403:2133-61. [Crossref] [PubMed]
- Li S, Huang X, Liu J, et al. Trends in the Incidence and DALYs of Urolithiasis From 1990 to 2019: Results From the Global Burden of Disease Study 2019. Front Public Health 2022;10:825541. [Crossref] [PubMed]
- Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet 2024;403:2162-203. [Crossref] [PubMed]
- Khazaei Z, Goodarzi E, Borhaninejad V, et al. The association between incidence and mortality of brain cancer and human development index (HDI): an ecological study. BMC Public Health 2020;20:1696. [Crossref] [PubMed]
- Tian YQ, Yang JC, Hu JJ, et al. Trends and risk factors of global incidence, mortality, and disability of genitourinary cancers from 1990 to 2019: Systematic analysis for the Global Burden of Disease Study 2019. Front Public Health 2023;11:1119374. [Crossref] [PubMed]
- Van Poppel H, Albreht T, Basu P, et al. Serum PSA-based early detection of prostate cancer in Europe and globally: past, present and future. Nat Rev Urol 2022;19:562-72. [Crossref] [PubMed]
- Aboagye EO, Barwick TD, Haberkorn U. Radiotheranostics in oncology: Making precision medicine possible. CA Cancer J Clin 2023;73:255-74. [Crossref] [PubMed]
- Parker CC, Kynaston H, Cook AD, et al. Duration of androgen deprivation therapy with postoperative radiotherapy for prostate cancer: a comparison of long-course versus short-course androgen deprivation therapy in the RADICALS-HD randomised trial. Lancet 2024;403:2416-25. [Crossref] [PubMed]
- de Vos II, Luiting HB, Roobol MJ. Active Surveillance for Prostate Cancer: Past, Current, and Future Trends. J Pers Med 2023;13:629. [Crossref] [PubMed]
- Vaccarella S, Li M, Bray F, et al. Prostate cancer incidence and mortality in Europe and implications for screening activities: population based study. BMJ 2024;386:e077738. [Crossref] [PubMed]
- Zhang H, Ji J, Liu Z, et al. Artificial intelligence for the diagnosis of clinically significant prostate cancer based on multimodal data: a multicenter study. BMC Med 2023;21:270. [Crossref] [PubMed]
- Han HH, Park JW, Na JC, et al. Epidemiology of prostate cancer in South Korea. Prostate Int 2015;3:99-102. [Crossref] [PubMed]
- Egan KB. The Epidemiology of Benign Prostatic Hyperplasia Associated with Lower Urinary Tract Symptoms: Prevalence and Incident Rates. Urol Clin North Am 2016;43:289-97. [Crossref] [PubMed]
- Zhang H, Huang D, Zhang Y, et al. Global burden of prostate cancer attributable to smoking among males in 204 countries and territories, 1990-2019. BMC Cancer 2023;23:92. [Crossref] [PubMed]
- Zi H, He SH, Leng XY, et al. Global, regional, and national burden of kidney, bladder, and prostate cancers and their attributable risk factors, 1990-2019. Mil Med Res 2021;8:60. [Crossref] [PubMed]
- Safitri W, Martini S, Artanti KD, et al. Smoking from a Younger Age Is the Dominant Factor in the Incidence of Chronic Obstructive Pulmonary Disease: Case-Control Study. Int J Environ Res Public Health 2021;18:6047. [Crossref] [PubMed]
- Langlais CS, Graff RE, Van Blarigan EL, et al. Post-Diagnostic Dietary and Lifestyle Factors and Prostate Cancer Recurrence, Progression, and Mortality. Curr Oncol Rep 2021;23:37. [Crossref] [PubMed]
- Marais B, Klopper G, John J. Prostate cancer perspective: Africa versus the world. S Afr Med J 2024;114:e1950. [Crossref] [PubMed]
- Schafer EJ, Laversanne M, Sung H, et al. Recent Patterns and Trends in Global Prostate Cancer Incidence and Mortality: An Update. Eur Urol 2025;87:302-13. [Crossref] [PubMed]
- Hamilton AC, Donnelly DW, Loughrey MB, et al. Inequalities in the decline and recovery of pathological cancer diagnoses during the first six months of the COVID-19 pandemic: a population-based study. Br J Cancer 2021;125:798-805. [Crossref] [PubMed]
- Lemanska A, Andrews C, Fisher L, et al. During the COVID-19 pandemic 20 000 prostate cancer diagnoses were missed in England. BJU Int 2024;133:587-95. [Crossref] [PubMed]
- Chakravarty D, Ratnani P, Sobotka S, et al. Increased Hospitalization and Mortality from COVID-19 in Prostate Cancer Patients. Cancers (Basel) 2021;13:1630. [Crossref] [PubMed]


