
A prospective study to determine the safety and feasibility of opioid-free discharge after percutaneous nephrolithotomy
Highlight box
Key findings
• We found that opioid-free discharge after percutaneous nephrolithotomy (PCNL) is safe and feasible in a limited prospective study utilizing a nonopioid protocol.
What is known and what is new?
• Routine opioid prescriptions after surgical procedures have contributed to the American opioid epidemic. The feasibility of nonopioid protocols after endourologic procedures such as ureteroscopy has been shown both retrospectively and prospectively, however, the feasibility and safety of opioid-free discharge after PCNL have not been fully evaluated.
• This study demonstrates our experience with a nonopioid protocol for postoperative pain and its effect on participant symptoms and outpatient healthcare resource utilization after PCNL.
What is the implication, and what should change now?
• Urologists should consider an opioid-free discharge following uncomplicated PCNL with stent placement. Further randomized studies are necessary to confirm our findings.
Introduction
The impact of the opioid epidemic in the United States is well-established, and research in the urologic community continues to focus on the reduction of opioid prescriptions for postoperative pain to minimize exposure risk to patients and communities (1). Within the gamut of urologic diseases, patients with kidney stones may have a higher risk for long-term opioid use than non-stone formers (2), indicating the importance of minimizing unnecessary opioid exposure and further emphasizing the need for research into opioid reduction after kidney stone surgery. The risk of opioid tolerance and addiction due to this exposure has been documented: Kang et al. demonstrated that 1-in-8 stone formers who undergo ureteroscopy and laser lithotripsy (URSLL) require additional opiate prescriptions within 30 days (3). Additionally, Tam et al. showed that nearly 1 in 16 (6.2%) opioid-naïve patients developed new persistent opioid use after URSLL demonstrated by continued filling of opioid prescriptions 6 months after surgery (4). Efforts to reduce opioids after endourologic procedures have begun at the provider level to develop national consensus guidelines regarding the prescription of pain control medications (5).
Opioid-sparing pathways for URSLL have been developed and studied both retrospectively and prospectively, with a significant reduction in the routine prescription of opioids seen with these multimodal protocols (6-9). Most pathways studied have utilized nonsteroidal anti-inflammatory drugs (NSAIDs) as a substitute for opioid medications, such as oxycodone or hydromorphone. The SKOPE trial (Study of Ketorolac vs Opioid for Pain after Endoscopy: A Double-Blinded Randomized Control Trial in Patients Undergoing Ureteroscopy) prospectively demonstrated noninferiority of oral ketorolac to oxycodone for post-ureteroscopy pain management (8). Other adjunctive medications such as alpha-blockers, anticholinergics, and phenazopyridine have been used for stent specific symptoms, such as renal colic and irritative lower urinary tract symptoms (LUTS) related to the indwelling stent with efficacy for some time (10-12). Additionally, opioid-sparing protocols do not seem to negatively impact outpatient resource utilization, such as telephone calls to the clinic or emergency department (ED) visits (13), and in some studies have been shown to be associated with reduced outpatient resource utilization (7,14). Despite this evidence in support of nonopioid alternatives for postoperative pain management, there remains significant variation in prescribing patterns for opioids after urologic surgery (15,16).
Only recently, however, has experience gained from nonopioid URSLL been applied to percutaneous nephrolithotomy (PCNL). A meta-analysis by Cabo et al. in 2024 revealed only two opioid-sparing enhanced recovery after surgery (ERAS) pathways studied in the setting of PCNL (17). PCNL is a more invasive stone treatment modality than URSLL, and pain after PCNL is likely multifactorial in etiology secondary to interoperative factors such as the incision, tract dilation, torque on the kidney, intrarenal pressure, possible dilation of the ureter and nephrostomy tube, or ureteral stent placement. Complications such as hematoma or urinoma formation, or persistent hydronephrosis due to obstruction, can cause significant postoperative pain and may increase narcotic use (18). Wu et al. retrospectively studied 331 patients who underwent PCNL at a single institution and found that nearly 67% of patients described moderate-to-severe (4-10) pain on the visual analog scale (VAS) postoperatively (19). The TOWER research collaborative studied postoperative pain after PCNL compared URSLL by administering the Patient-Reported Outcomes Measurement Information System (PROMIS) postoperatively at postoperative day (POD) 1, 7 and 14. URSLL patients were found to have below-baseline pain intensity and interference on POD 14, but PCNL patients reported pain intensity and interference above baseline for at least 14 days (20). While URSLL and PCNL share many endourologic aspects, the more invasive nature of PCNL may require more pain control than the current nonopioid pathways implemented for ureteroscopy can safely offer.
Given the limited inquiry into the safety and feasibility of opioid-free discharge after PCNL, we aimed to evaluate the feasibility of a nonopioid protocol consisting of enhanced preoperative counseling, standardized multimodal nonopioid analgesics, and detailed postoperative instructions for discharge after PCNL without opioid prescriptions. We present this article in accordance with the TREND reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-2024-692/rc).
Methods
This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the institutional review board of The Miriam Hospital, Lifespan (#212920). The study was supported by the National Institute of General Medical Sciences of the National Institutes of Health (No. P20GM125507) and was prospectively registered (clinicaltrials.gov: NCT04597619). It was designed as a pragmatic pre/post pilot study where eligible patients were offered unblinded participation prospectively. Following completion of accrual for the pre-intervention arm, the nonopioid protocol was implemented and patients meeting inclusion criteria were offered participation in the intervention arm.
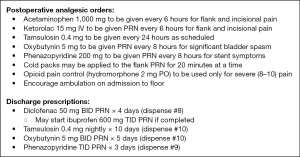
The nonopioid protocol was developed from prior research and experience for pain management following URSLL (6) and consisted of preoperative, intraoperative, and postoperative elements. Enhanced preoperative counseling was conducted during outpatient surgical consultation after enrollment and in the preoperative area and consisted of verbal review of all expected potential stent symptoms. Intraoperative and postoperative components were developed with multidisciplinary support from anesthesiology, perioperative nursing, and floor nursing teams and consisted of a standardized medication order set for inpatient and outpatient administration (Figure 1), instructions for nursing and urology house staff (Appendix 1) and detailed postoperative discharge instructions for patients (Appendix 2). Scheduled and as necessary postoperative medications for stent discomfort, consisting of acetaminophen, tamsulosin, diclofenac, phenazopyridine, oxybutynin, were standardized. Nursing staff were educated on the protocol via group presentations, and implemented order sets and discharge instructions were reviewed with house-staff and nursing.
The primary outcome was discharge from the hospital without prescription for opioid pain medication after PCNL utilizing the nonopioid protocol. Secondary outcomes investigated were adherence to the protocol, postoperative inpatient intravenous and oral opioid utilization [morphine mEq/kg/day (MEDD)], length of stay, duration of indwelling stent, Ureteral Stent Symptom Questionnaire (USSQ) (21) scores at time of stent removal, adverse events (AEs) while inpatient and following discharge, and outpatient healthcare resource utilization measured by calls to clinic for pain/discomfort, requests for refills of opioid prescriptions, new prescriptions for opioids written by other providers found in the state prescription drug monitoring program (PDMP) and ED visits for genitourinary (GU) concerns or pain within thirty days after stent removal in the office.
Statistical analysis
All analyses were performed using R Statistical Software (v4.2.2; R Core Team 2022). Primary outcome analysis utilized Fisher’s exact test. Secondary outcomes were evaluated using Fisher’s exact test for categorical variables and Wilcoxon rank sum test for continuous variables. The data was not normal, and therefore medians were reported for descriptive statistics.
Study procedures
Adult participants (>18 years old) who underwent outpatient consultation for PCNL at the Minimally Invasive Urology Institute (The Miriam Hospital, Providence, RI, USA) were screened for eligibility to participate. Patients were excluded if taking opioids for chronic pain, were planned to have a concurrent non-PCNL procedure, second-look PCNL, or presented with chronic kidney disease (CKD) stage >3 or estimated glomerular filtration rate (eGFR) <50 mL/min/1.73 m2 at time of surgery. Patients with a documented allergy to NSAIDs or with a history of NSAID-related gastrointestinal bleeding or ulcers were excluded. Individuals with an existing indwelling ureteral stent or percutaneous nephrostomy tube were also excluded. Written informed consent was obtained from all individual participants at the time of screening and eligibility review during outpatient surgical consultation.
All enrolled participants underwent PCNL at a single institution by a single endourology fellowship-trained surgeon in the prone split-leg position utilizing a single 30 French access tract. Fluoroscopic-guided renal access was obtained by the urologist at a time of surgery. A 6 or 7 French double J ureteral stent and urethral Foley catheter were placed at the conclusion of the case. The caliber and length of the stent were at the discretion of the surgeon. No nephrostomy tubes were placed. No local anesthetic was administered peri-procedurally. Pre-intervention group participants received standard of care anesthetic medications at the discretion of the anesthesiologist, while intervention arm participants additionally received Ketorolac 15 mg intravenously administered at the end of the procedure. Standard-of-care adjunctive and analgesic medications were administered at the anesthesiologist’s discretion in the post-anesthesia care unit (PACU) postoperatively. Intravenous and oral opioid medications were not restricted in the immediate postoperative period (2–4 hours prior to transfer to the floor) in PACU and were administered per nursing protocol and anesthesiologist standard-of-care. All participants were admitted to the floor following surgery for observation. Pain was assessed using the numeric rating scale (NRS) every 4 hours. Participants in the pre-intervention group received postoperative orders and medications at the discretion of the ordering urology house staff.
Following pre-intervention group accrual, the nonopioid protocol was implemented institutionally and eligible patients were enrolled in the intervention group. Participants underwent the protocol starting in the preoperative setting with review of all expected potential stent symptoms and adjunctive medications and interventions for symptom relief at a time of surgical consultation, as well as the preoperative holding area prior to surgery. Following surgery, they received nonopioid medications via the standardized order set in the postoperative setting (Figure 1). At the time of discharge, intervention arm participants were queried to confirm that they felt comfortable going home without a prescription for opioids. If they were not comfortable, they were given a prescription for five (5) tablets of oxycodone 5 mg. Participants received detailed discharge instructions regarding expectations for pain and stent symptoms (Appendix 2). All participants were seen in the office 7–10 days following discharge for cystoscopic stent removal, and during this visit, the Ureteral Stent Symptom Questionnaire (USSQ) was administered (8). Follow-up and review of outcomes through study activities were standardized in the two groups to minimize reporting bias. Participant outcomes were prospectively followed for thirty days after stent removal. The state PDMP was queried at the conclusion of study activities to assess for any additional opioid prescriptions made by other providers during the study. AEs were monitored weekly and as necessary throughout the study activity per IRB protocol.
Results
Participant demographics are described in Table 1, and the surgical characteristics of both groups are depicted in Table 2. Seventy-eight patients were screened for eligibility during the study period. Participant recruitment for the pre-intervention group began in December 2020 and ended August 2021. Twenty patients consented to undergo the pre-intervention standard-of-care treatment. Following enrollment, six patients were excluded from participating in the study: One patient failed screening labs (eGFR <50 mL/min/1.73 m2) after consent, one patient was stented due to pain prior to PCNL, and 4 patients underwent alternate or additional procedures (one patient underwent staged URSLL, two patients underwent PCNL and contralateral URSLL, and one patient had an aborted PCNL due to inability to access the kidney).
Table 1
| Characteristics | Pre-intervention group (N=14) | Intervention group (N=6) | P value |
|---|---|---|---|
| Age (years) | 59.5 [13.0] | 52.0 [20.0] | 0.23 |
| Sex | 0.61 | ||
| Female | 10 (71.4) | 3 (50.0) | |
| Male | 4 (28.6) | 3 (50.0) | |
| BMI (kg/m2) | 34.3 [10.9] | 27.8 [9.50] | >0.99 |
| ASA score | 2.00 [0.750] | 2.00 [0] | 0.58 |
| HTN | 0.63 | ||
| No | 6 (42.9) | 4 (66.7) | |
| Yes | 8 (57.1) | 2 (33.3) | |
| CAD | >0.99 | ||
| No | 13 (92.9) | 6 (100.0) | |
| Yes | 1 (7.1) | 0 (0) | |
| DM | 0.61 | ||
| No | 9 (64.3) | 5 (83.3) | |
| Yes | 5 (35.7) | 1 (16.7) | |
| Preoperative creatinine (mg/dL) | 0.800 [0.250] | 0.900 [0.225] | >0.99 |
| Previous nephrolithiasis requiring surgical intervention | >0.99 | ||
| No | 10 (71.4) | 5 (83.3) | |
| Yes | 4 (28.6) | 1 (16.7) | |
| Total stone size (mm) on CT | 23.0 [23.3] | 25.5 [7.00] | 0.71 |
| Side of stone | 0.35 | ||
| Right | 6 (42.9) | 1 (16.7) | |
| Left | 8 (57.1) | 5 (83.3) |
Data are presented as n (%) or median [interquartile range]. ASA, American Society of Anesthesiologists; BMI, body mass index; CAD, coronary artery disease; CT, computed tomography; DM, diabetes mellitus; HTN, hypertension.
Table 2
| Characteristic | Pre-intervention group (N=14) | Intervention group (N=6) | P value |
|---|---|---|---|
| Location of access | >0.99 | ||
| Upper pole calyx | 3 (21.4) | 1 (16.7) | |
| Interpolar calyx | 3 (21.4) | 2 (33.3) | |
| Lower pole calyx | 8 (57.1) | 3 (50.0) | |
| Ribspace | >0.99 | ||
| Subcostal (below 12th rib) | 10 (71.4) | 4 (66.7) | |
| Supracostal (above 12th rib) | 4 (28.6) | 2 (33.3) | |
| Number of percutaneous attempts | >0.99 | ||
| One | 10 (71.4) | 5 (83.3) | |
| Two to three | 4 (28.6) | 1 (16.7) | |
| Greater than 3 | 0 | 0 | |
| Procedure length (min) | 89.0 [23.3] | 85.0 [26.0] | 0.46 |
| Procedure EBL (cc) | 17.5 [17.5] | 12.5 [6.50] | 0.14 |
| Stent circumference (Fr) | 6.00 [0.750] | 7.00 [0] | 0.03 |
| Complication during procedure | >0.99 | ||
| No complications encountered | 14 (100.0) | 6 (100.0) | |
| Complications encountered | 0 | 0 |
Data are presented as n (%) or median [interquartile range]. EBL, estimated blood loss.
Participant recruitment for the intervention group began in September 2021 and ended in March 2022. Ten patients consented to participate in the intervention arm of the study. Three patients (30%) withdrew from the study following consent but prior to surgery due to anxiety about the potential for increased discomfort. One patient failed screening labs (eGFR <50 mL/min/1.73 m2) and was excluded from participation. Six participants underwent intervention and received the entire perioperative protocol consisting of enhanced preoperative counseling, multimodal nonopioid analgesics, specific nursing teaching, and detailed postoperative instructions. Table 3 describes postoperative details regarding pain control, discharge medications, and outpatient postoperative course in the two groups.
Table 3
| Outcome | Pre-intervention group (N=14) | Intervention group (N=6) | P value |
|---|---|---|---|
| Length of stay (days) | 1.00 [0] | 1.00 [0] | 0.59 |
| Stent duration (days) | 8.00 [1.75] | 8.00 [0] | 0.50 |
| PRN opioid received on floor | 0.16 | ||
| No | 4 (28.6) | 4 (66.7) | |
| Yes | 10 (71.4) | 2 (33.3) | |
| Scheduled inpatient acetaminophen ordered | 0.02 | ||
| No | 0 | 3 (50.0) | |
| Yes | 14 (100.0) | 3 (50.0) | |
| Inpatient intravenous MEDD (mEq/kg/day) | 4.00 [2.00] | 0 [0] | 0.21 |
| Inpatient oral MEDD (mEq/kg/day) | 7.50 [2.50] | 16.0 [8.00] | 0.20 |
| Scheduled NSAID ordered | 0.051 | ||
| No | 7 (50.0) | 0 (0) | |
| Yes | 7 (50.0) | 6 (100.0) | |
| Most severe pain score during inpatient stay (NRS) | 7.00 [3.50] | 6.00 [2.75] | >0.99 |
| Pain score at time of discharge (NRS) | 2.00 [3.75] | 2.50 [3.25] | 0.59 |
| No new opioid prescription at time of discharge | 0.01 | ||
| No | 10 (71.4) | 0 | |
| Yes | 4 (28.6) | 6 (100.0) | |
| Outpatient MEDD (mEq/kg/day) | 20.0 [30.0] | 0 [0] | 0.01 |
| Phenazopyridine prescribed at discharge | 0.052 | ||
| No | 7 (50.0) | 0 | |
| Yes | 7 (50.0) | 6 (100.0) | |
| Tamsulosin prescribed at discharge | 0.26 | ||
| No | 5 (35.7) | 0 | |
| Yes | 9 (64.3) | 6 (100.0) | |
| Oxybutynin prescribed at discharge | 0.26 | ||
| No | 5 (35.7) | 0 | |
| Yes | 9 (64.3) | 6 (100.0) | |
| NSAID prescribed at discharge | 0.01 | ||
| No | 9 (64.3) | 0 | |
| Yes | 5 (35.7) | 6 (100.0) | |
| ED visit within 30 days | >0.99 | ||
| No | 12 (85.7) | 6 (100.0) | |
| Yes | 2 (14.3) | 0 | |
| Telephone call to office for pain, GU complaint within 30 days | 0.52 | ||
| No | 13 (92.9) | 5 (83.3) | |
| Yes | 1 (7.1) | 1 (16.7) | |
| Operative reintervention for same nephrolithiasis | 0.52 | ||
| No | 13 (92.9) | 5 (83.3) | |
| Yes | 1 (7.1) | 1 (16.7) | |
| Secondary nonoperative procedure within 30 days | >0.99 | ||
| No | 14 (100.0) | 6 (100.0) | |
| Yes | 0 | 0 | |
| Request for refill opioid pain medication | >0.99 | ||
| No | 14 (100.0) | 6 (100.0) | |
| Yes | 0 | 0 | |
| Patient was prescribed a separate opioid within 30 days | >0.99 | ||
| No | 12 (85.7) | 6 (100.0) | |
| Yes | 2 (14.3) | 0 | |
Data are presented as n (%) or median [interquartile range]. ED, emergency department; GU, genitourinary; MEDD, morphine equivalent daily dose; NRS, Numeric Rating Scale; NSAID, non-steroidal anti-inflammatory drug; PRN, as necessary.
Primary outcome
Ten of the fourteen participants enrolled in the pre-intervention group (71%) who completed study activities were discharged with opioid prescriptions (8 participants received oxycodone 5 mg tablets and 2 received tramadol 50 mg tablets), and 4 participants (29%) were discharged without opioids. All six participants (100%) in the intervention group were able to be discharged without a prescription for opioids.
Secondary outcomes
All intervention group participants (100% protocol adherence) received the entire perioperative protocol consisting of enhanced preoperative counseling, multimodal nonopioid analgesics, specific nursing teaching and detailed postoperative instructions. All received the prescriptions for the nonopioid adjunctive protocol medications on discharge. Postoperative inpatient intravenous opioid utilization (MEDD) was lower in the intervention group {median 0 [interquartile range (IQR), 0] vs. 4.00 (IQR, 2.00) mEq/kg/day in the pre-intervention group}, however, oral opioid utilization was higher in the intervention group [median 16.0 (IQR, 8.00) vs. 7.50 (IQR, 2.50) mEq/kg/day] than the pre-intervention group. Length of stay was the same between the pre-intervention and the intervention groups [median 1.00 (IQR, 0.0) day]. There were no inpatient protocol deviations in the intervention group.
After discharge and prior to stent removal, 2 participants (14%) in the pre-intervention group presented to the ED for pain concerns, and both were discharged home with a new prescription for opioids in addition to their discharge opioid prescription. No participants in the intervention group presented to the ED for GU concerns or pain before or after stent removal. One participant (7%) in the pre-intervention group called the office for parosmia and dysgeusia and was provided reassurance over the phone. One participant (17%) in the intervention group called the office for stent discomfort and was provided reassurance over the phone. No new prescriptions for opioids were written within 30 days after surgery for intervention group participants. No outpatient prescription refills for opioids were ordered by the urology clinic for any participants. There were no inpatient or outpatient AEs in either arm related to or unrelated to the protocol.
Indwelling ureteral stents were removed on a median of 7 (IQR, 2.0) days after surgery in the pre-intervention group and a median of 7 (IQR, 0.0) days in the intervention arm. The administered USSQ responses at the time of stent removal are summarized in Table 4. The averaged pain across all body locations on the VAS was similar between the two groups [median 6.00 (IQR, 3.84) in the pre-intervention group and 5.67 (IQR, 3.33) in the intervention group]. Symptoms from the stent lasted a median of 1.5 (IQR, 2.25) days for pre-intervention group participants and 0.5 (IQR, 1.0) days for the intervention group participants.
Table 4
| Question | Pre-intervention group (N=14) | Intervention group (N=6) | P value |
|---|---|---|---|
| Overall, how much of a problem are your urinary symptoms to you? | 0.12 | ||
| Not at all | 2 (14.3) | 0 | |
| A little bit | 3 (21.4) | 4 (66.7) | |
| Moderate | 7 (50.0) | 1 (16.7) | |
| Quite a bit | 2 (14.3) | 0 | |
| Extreme | 0 | 1 (16.7) | |
| If you were to spend the rest of your life with your current urinary symptoms, how would you feel? | 0.77 | ||
| Delighted | 0 | 0 | |
| Pleased | 0 | 0 | |
| Mostly satisfied | 0 | 0 | |
| Mixed feelings | 4 (28.6) | 2 (33.3) | |
| Mostly dissatisfied | 3 (21.4) | 0 | |
| Unhappy | 3 (21.4) | 2 (33.3) | |
| Terrible | 4 (28.6) | 2 (33.3) | |
| Do you experience body pain or discomfort, which you associate with the stent? | >0.99 | ||
| Yes | 11 (78.6) | 5 (83.3) | |
| No | 3 (21.4) | 1 (16.7) | |
| Averaged pain reported across all body locations (VAS) | 6.00 [3.84] | 5.67 [3.33] | 0.38 |
| For those who experience body pain or discomfort in association with the stent, how frequently have you required painkillers to control the pain or discomfort associated? | (N=11) | (N=5) | 0.65 |
| Never | 3 (27.3) | 1 (20.0) | |
| Occasionally | 3 (27.3) | 2 (40.0) | |
| Sometimes | 3 (27.3) | 0 | |
| Most of the time | 1 (9.1) | 2 (40.0) | |
| All of the time | 1 (9.1) | 0 | |
| Following the insertion of the stent, how many days did the symptoms associated with the stent last? | 1.50 [2.25] | 0.500 [1.00] | 0.52 |
| In the future, if you were advised to have another stent inserted, how would you feel? | 0.24 | ||
| Delighted | 1 (7.1) | 0 | |
| Pleased | 0 | 0 | |
| Mostly satisfied | 3 (21.4) | 0 | |
| Mixed feelings | 4 (28.6) | 4 (66.7) | |
| Mostly dissatisfied | 2 (14.3) | 0 | |
| Unhappy | 3 (21.4) | 0 | |
| Terrible | 1 (7.1) | 2 (33.3) |
Data are presented as n (%) or median [interquartile range] unless otherwise indicated. VAS, visual analog scale.
Discussion
We present a prospective study demonstrating the safety and feasibility of a nonopioid protocol for standard PCNL with stent placement. There have been far fewer studies evaluating pain management and opioid sparing pathways after PCNL than URSLL (17). Girgiss et al. demonstrated reduced opioid prescription and higher quality-of-life (QOL) scores on validated questionnaires following PCNL with a standardized ERAS protocol (22). This protocol included preoperative medications such as tamsulosin daily for 7 days prior to surgery and preoperative gabapentin and intraoperative rectal belladonna/opium suppositories, which may have a role in improved postoperative pain control but are distinct from other ureteroscopy-based pain control pathways previously described. Additionally, the ERAS group was compared against an age-matched historical cohort from a time period prior to implementation of the protocol for assessment of opioid reduction, however, QOL metrics were not directly compared between these two groups.
Specifically utilizing NSAIDs for postoperative pain control after PCNL, Li and colleagues published the results of their prospective randomized trial for participants undergoing 18 Fr PCNL with nephrostomy tube placement randomized to ERAS pathway utilizing intramuscular parecoxib 40 mg or flurbiprofen 50 mg intravenous administration versus intramuscular diclofenac. They found that complications were similar and subjective pain scores in the ERAS group were significantly lower on the VAS 4 hours after surgery. Some practice patterns, such as the control group undergoing absolute bed rest for 3–4 days after surgery, limit comparisons to other institutional experiences and enhanced recovery protocols studied (23).
Demasi and colleagues published their experience with non-opioids after ureteroscopy and PCNL prospectively with randomization to ketorolac (44 patients) or oxycodone-acetaminophen (49 patients) (24). While the groups were mixed with both completely endoscopic and percutaneous stone treatment, with only 28/90 (31%) patients receiving PCNL, pain was statistically significantly lower in the group receiving non-opioids [average pain scores were 3.20±1.94 (SD) with those receiving ketorolac and 4.17±1.84 in those receiving oxycodone-acetaminophen, P=0.02]. A subgroup analysis of those patients undergoing PCNL was not included, limiting interpretation. Additionally, the patient population was mixed regarding stent placement during the procedure.
Most recently, Khargi and colleagues published their single-center retrospective experience reviewing their quality improvement initiative to reduce opioid prescriptions following PCNL (25). In their institution, oxycodone-acetaminophen was replaced with 12 tablets of ketorolac following ambulatory PCNL and pre- and post-intervention groups were evaluated for pain-related encounters. Both those patients receiving ketorolac and oxycodone-acetaminophen were found to have similarly low levels of unplanned pain-related encounters (8/70, 11.4% vs. 10/70, 14.3%, respectively, P=0.614). With 140 consecutive patients, this represents the largest retrospective data supporting the use of NSAIDs for post-PCNL pain control. Some acknowledged limitations were included a large timespan of cases reviewed in which surgical technique changed, as fewer stents were left in the ketorolac group. Still, this data supports the safe and feasible use of NSAIDs instead of opioids after PCNL.
Our preliminary study demonstrates that opioid-free discharge is feasible after 30fr PCNL and ureteral stent placement using our nonopioid protocol that includes preoperative counseling, a standardized multimodal nonopioid order set, and PCNL-specific discharge instructions. The primary outcome of discharge without a prescription for opioid pain medication was attainable in all intervention group participants. All participants in the intervention group were given the standardized medication regimen while inpatient and discharged with the protocol nonopioid prescriptions, indicating high adherence to the protocol by nursing staff and urology house staff. In addition to being discharged without an opioid prescription, fewer participants undergoing intervention received opioids while inpatient (33% vs. 71% of pre-intervention group participants) and the median most severe pain while in the hospital was similar between the two groups [6.0 (IQR, 2.75) vs. 7.0 (IQR, 3.75)]. Median pain scores at time of discharge were low in both groups [median 2.5 (IQR, 3.25) vs. 2.0 (IQR, 3.75) in the pre-intervention group]. Length of stay was similar, indicating that inpatient recovery after PCNL was not impacted by the nonopioid protocol.
Additionally, the protocol did not appear to negatively impact outpatient pain control. The averaged pain across all body locations reported on the USSQ at time of stent removal was similar between the two groups, indicating that the outpatient regimen of standardized adjunctive nonopioid medications (acetaminophen, tamsulosin, phenazopyridine, oxybutynin) and the absence of an opioid medication did not significantly change postoperative pain at the time of survey completion.
Importantly, this nonopioid protocol did not increase the utilization of outpatient resources required to manage pain concerns: no participants in the intervention arm presented to the ED, requested refills of analgesic medications or underwent early stent removal due to intolerance, similar to findings seen by the Michigan Urologic Surgery Improvement Collaborative (MUSIC) and others after URSLL (6,7,13,14). It should be noted that a subset of the control group (four participants) was also discharged without a prescription for opioid analgesics at the discretion of the urology house staff or advanced practice provider (APP) performing the discharge. This suggests that a paradigm shift toward postoperative opioid reduction in general has begun and that provider awareness and patient expectations may play a role in this shift (26).
Our study has several limitations. The small cohort size and nonrandomized groups limit wide applicability. The study was designed to evaluate feasibility and safety rather than a comparison of the protocol to standard-of-care for non-inferiority. Accrual was severely attenuated during and immediately after the coronavirus disease 2019 (COVID-19) pandemic, as many patients with large stone burdens underwent stent or nephrostomy tube placement as a temporizing measure, which made them ineligible for participation in the study. Pre-stented patients and patients with nephrostomy tubes were specifically excluded from participation due to the potential confounding that an existing indwelling tube or stent may have on postoperative outcomes studied. Three of the ten participants who consented to participation in the intervention arm withdrew from the study prior to surgery due to concern and anxiety about postoperative pain, indicating the real and perceived patient concerns regarding postoperative recovery without opioids. Additionally, patients with underlying renal insufficiency (CKD stage >3 or eGFR <50 mL/min/1.73 m2) were excluded from participating given the protocol’s use of NSAIDs for pain control. While it was not measured in our study, there remain patients for whom opioid medications for postoperative pain after PCNL are likely necessary. Based on previous studies, opioids may be necessary for those with CKD, chronic opioid tolerance or existing use, and history of chronic pain, post-traumatic stress disorder (PTSD) or depression (7,16). Surgical technique was limited to standard 30 Fr PCNL with ureteral stent placement, which may limit applicability to other techniques for PCNL, such as totally-tubeless PCNL and mini PCNL. Adjunctive medications used in the protocol were included to address symptoms related to stent discomfort, which may not be necessary if stents are not utilized. Pill counts were not performed and opioid use after discharge was not discretely measured in the pre-intervention group, however, opioid prescriptions written represent overall potential opioid exposure to the participant, family and community. Despite these limitations, we feel this study contributes to the increasing body of literature supporting nonopioid protocols after PCNL.
Conclusions
This preliminary evaluation of a nonopioid protocol consisting of enhanced preoperative counseling, multimodal nonopioid analgesics and detailed postoperative instructions for patients undergoing standard PCNL with stent placement demonstrates initial safety and feasibility. Patients discharged without opioids had low levels of postoperative pain with minimal impact on outpatient healthcare resources. Further evaluation of this protocol and other efforts at reducing opioid exposure after PCNL are necessary and ongoing.
Acknowledgments
Data from this manuscript has been previously presented at the 92nd Annual Meeting of the New England Section of the American Urological Association (NEAUA) on September 7, 2023, Bretton Woods, NH, USA.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-2024-692/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-2024-692/dss
Peer Review File: Available at https://tau.amegroups.com/article/view/10.21037/tau-2024-692/prf
Funding: This work was supported by
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-2024-692/coif). D.S. reports that this research was supported by the NIH Grant P20GM125507. D.S. is a consultant for Olympus Corporation and Boston Scientific Corporation and recipient of a Boston Scientific Investigator Sponsored Research grant unrelated to this research. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study was conducted in accordance with the Declaration of Helsinki and its subsequent amendments. The study was approved by the institutional review board of The Miriam Hospital, Lifespan (#212920) and informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kiechle JE, Gonzalez CM. The Opioid Crisis and Urology. Urology 2018;112:27-8. [Crossref] [PubMed]
- Shoag JE, Patel N, Posada L, et al. Kidney Stones and Risk of Narcotic Use. J Urol 2019;202:114-8. [Crossref] [PubMed]
- Kang C, Shu X, Herrell SD, et al. Opiate Exposure and Predictors of Increased Opiate Use After Ureteroscopy. J Endourol 2019;33:480-5. [Crossref] [PubMed]
- Tam CA, Dauw CA, Ghani KR, et al. New Persistent Opioid Use After Outpatient Ureteroscopy for Upper Tract Stone Treatment. Urology 2019;134:103-8. [Crossref] [PubMed]
- Koo K, Winoker JS, Patel HD, et al. Evidence-Based Recommendations for Opioid Prescribing After Endourological and Minimally Invasive Urological Surgery. J Endourol 2021;35:1838-43. [Crossref] [PubMed]
- Large T, Heiman J, Ross A, et al. Initial Experience with Narcotic-Free Ureteroscopy: A Feasibility Analysis. J Endourol 2018;32:907-11. [Crossref] [PubMed]
- Sobel DW, Cisu T, Barclay T, et al. A Retrospective Review Demonstrating the Feasibility of Discharging Patients Without Opioids After Ureteroscopy and Ureteral Stent Placement. J Endourol 2018;32:1044-9. [Crossref] [PubMed]
- Fedrigon D, Faris A, Kachroo N, et al. SKOPE-Study of Ketorolac vs Opioid for Pain after Endoscopy: A Double-Blinded Randomized Control Trial in Patients Undergoing Ureteroscopy. J Urol 2021;206:373-81. [Crossref] [PubMed]
- Gridley C, Robles J, Calvert J, et al. Enhanced Recovery After Surgery Protocol for Patients Undergoing Ureteroscopy: Prospective Evaluation of an Opioid-Free Protocol. J Endourol 2020;34:647-53. [Crossref] [PubMed]
- Damiano R, Autorino R, De Sio M, et al. Effect of tamsulosin in preventing ureteral stent-related morbidity: a prospective study. J Endourol 2008;22:651-6. [Crossref] [PubMed]
- Beddingfield R, Pedro RN, Hinck B, et al. Alfuzosin to relieve ureteral stent discomfort: a prospective, randomized, placebo controlled study. J Urol 2009;181:170-6. [Crossref] [PubMed]
- Zhou L, Cai X, Li H, et al. Effects of α-Blockers, Antimuscarinics, or Combination Therapy in Relieving Ureteral Stent-Related Symptoms: A Meta-Analysis. J Endourol 2015;29:650-6. [Crossref] [PubMed]
- Bevill MD, Schubbe ME, Flynn KJ, et al. Prospective Comparison of Opioid vs Nonopioid Pain Regimen After Ureteroscopy. J Endourol 2022;36:734-9. [Crossref] [PubMed]
- Johnson BA, Akhtar A, Crivelli J, et al. Impact of an Enhanced Recovery After Surgery Protocol on Unplanned Patient Encounters in the Early Postoperative Period After Ureteroscopy. J Endourol 2022;36:298-302. [Crossref] [PubMed]
- Berger I, Strother M, Talwar R, et al. National Variation in Opioid Prescription Fills and Long-Term Use in Opioid Naïve Patients after Urological Surgery. J Urol 2019;202:1036-43. [Crossref] [PubMed]
- Leapman MS, DeRycke E, Skanderson M, et al. Variation in National Opioid Prescribing Patterns Following Surgery for Kidney Stones. Pain Med 2018;19:S12-8. [Crossref] [PubMed]
- Cabo JJS, Miller NL. Nonopioid Pain Management Pathways for Stone Disease. J Endourol 2024;38:108-120. [Crossref] [PubMed]
- Khater N, Keheila M, Lightfoot M, et al. Predictors of narcotic use after percutaneous nephrolithotomy. Can J Urol 2017;24:8634-40. [PubMed]
- Wu H, Ding T, Yan S, et al. Risk factors for moderate-to-severe postoperative pain after percutaneous nephrolithotomy: a retrospective cohort study. Sci Rep 2022;12:8366. [Crossref] [PubMed]
- Jones A, Lin G, Stambakio H, et al. Post-operative pain and recovery in patients with nephrolithiasis: results from the endourological society tower research collaborative. J Urol 2022;206:e238. [Crossref]
- Joshi HB, Newns N, Stainthorpe A, et al. Ureteral stent symptom questionnaire: development and validation of a multidimensional quality of life measure. J Urol 2003;169:1060-4. [Crossref] [PubMed]
- Girgiss CBL, Berger JH, Chen TT, et al. Standardizing Perioperative Medications to Be Used in an Enhanced Recovery After Surgery Program Is Feasible in Percutaneous Nephrolithotomy Patients. J Endourol 2022;36:1265-70. [Crossref] [PubMed]
- Li Q, Wan L, Liu S, et al. Clinical efficacy of enhanced recovery after surgery in percutaneous nephrolithotripsy: a randomized controlled trial. BMC Urol 2020;20:162. [Crossref] [PubMed]
- Demasi M, Segall M, Mengotto A, et al. Optimizing pain management following kidney stone surgery: can we avoid narcotics? World J Urol 2022;40:3061-6. [Crossref] [PubMed]
- Khargi R, Yaghoubian AJ, Blake RM, et al. Opioid-free percutaneous nephrolithotomy: an initial experience. World J Urol 2023;41:3113-9. [Crossref] [PubMed]
- Robles J, Abraham N, Brummett C, et al. Rationale and Strategies for Reducing Urologic Post-Operative Opioid Prescribing. American Urological Association Quality Improvement Clinical Consensus Statement and Quality Improvement Issue Brief (CCS & QIIB); 2021.


