Penile fracture epidemiology, diagnosis and management in Iran: a narrative review
Introduction
Fracture of penis is a urological emergency resulting from a tear in the tunica albuginea of the penis often due to forceful manipulation, vigorous vaginal or anal intercourse or masturbation, gunshot wounds, or any other mechanical trauma that causes forcible bending of an erect penis. Less common etiologies include turning over in bed, a direct blow, forced bending, or hastily removing or applying clothing when the penis is erect (1). Most commonly, it involves one of the corpora cavernosa. It may also affect both corpora cavernous, corpus spongiosum or urethra (2). During erection, the thickness of the tunica albuginea decreases from 2 mm in the flaccid state to 0.25–0.5 mm. Therefore penis is more vulnerable to traumatic injury (3). The most common mechanism of injury is when the penis slips out of the vagina and strikes against the symphysis pubis or perineum. In some reports sixty per cent of cases occur during consensual intercourse (4), and is more likely when the partner is on top (5).
PF is commonly underreported in the published literature. In US, the reported incidence is 1 out of 175,000 male populations. The incidence of PF varies in different regions with divergent cultures. In some Eastern countries the incidence is higher and up to one case in a week may present to a busy emergency department (6). Some patients may not seek treatment because of embarrassment (2).
Here we review the epidemiology, diagnosis and management of PF in Iranian publications and also present our data from a recent questionnaire based survey study.
Definition
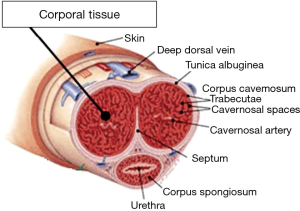
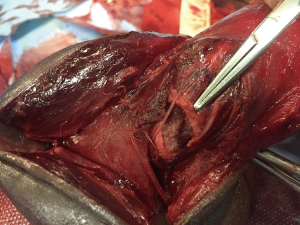
PF is defined as the traumatic rupture of the tunica albuginea of the corpora cavernosum (Figure 1) (7). Traumatic rupture of the penis is relatively uncommon and is considered a urologic emergency (8). The tunica albuginea is a bilaminar structure (inner circular, outer longitudinal) composed of collagen and elastin. The outer layer determines the strength and thickness of the tunica, which varies in different locations along the shaft and is thinnest ventrolaterally. The tensile strength of the tunica albuginea is remarkable, resisting rupture until intracavernous pressure increases to more than 1,500 mm Hg. When the erect penis bends abnormally, the abrupt increase in intracavernosal pressure exceeds the tensile strength of the tunica albuginea, and a transverse laceration of the proximal shaft usually results. Penile fracture may occur more frequently in “stressful situations” such as extramarital sex (1).
Epidemiology
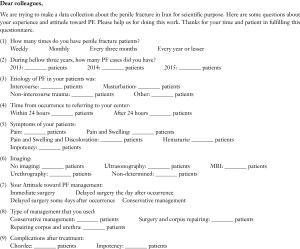
Trauma during sexual relations is responsible for approximately one third of all cases; the female-dominant position is most commonly reported. The mechanism of action may lead to embarrassment, causing patients to avoid seeking treatment and also contributing to late presentation and underreporting of the cases. As of 2001, 1,331 cases were reported in the literature. The incidence of concomitant urethral injury in reported cases is 10–58% (9). Incidence of PF in areas with distinct cultures is different (1). In reviewing Iranian literature we found data from four different geographical regions of Iran. Shafi et al. (6) reported 84 patients in 8 years from Northern Iran. Sixty six of these patients (79%) were singles and 46 (55%) were living in rural areas. Mean age of patients was 28.11 years old (ranging from 26 to 45). Asgari et al. reported 68 PF patients in 3 years from Tehran, Central Iran (10). Ahmadnia et al. mentioned in their study that during a 10-year period, they treated 116 patients with mean age of 32.78 (ranging from 16 to 62) (11). A study in Kermanshah, Western Iran, reported 18 years’ experience, with 373 patients (12). Moslemi investigated the PF in a 9-year period in Qom Province, Central Iran. He found 86 patients with the mean age of 36.74, (ranging from 17 to 62), 56 (65%) married and 30 (35%) singles. He also reported the seasonal variation of this disorder and indicated that 22 cases (25.5%) occurred in spring, 25 (29%) in summer, 17 (20%) in autumn, and 22 cases (25.5%) in winter with the lowest incidence in autumn that was statistically significant (13).Overall in four regions of Iran, the mean number of PF cases treated by urologists was reported as high as 15 case per year (1). To collect more comprehensive data and also to look for any recent change in incidence of PF we performed a questionnaire based study. Of 891 urologists in Iran, we were able to send a questionnaire (Figure S1) to 700 urologists in different parts of Iran. 97 urologists completed the questionnaire. The response rate was 14% which comparing to available literature seems acceptable. Table 1 show the results from our study. In Western Iran the mean frequency of PF patients treated by urologists was 1 every 2.31 months, Eastern Iran: 1 per 3 months, Southern Iran: 1 per 4.8, Northern Iran: 1 per 5.18, Capital of Iran (Tehran): 1 per 7.2 and Central of Iran (except Tehran): 1 per 10.5 months.
Full table
In this survey the number of reported cases within past three years in different areas of Iran was: North Iran: 96, Tehran: 307, South Iran: 118, East Iran: 27, Center: 25, West: 55. We should acknowledge that these data are limited to the centers that responded to the questionnaire. Based on this study the 97 urologists who responded to questionnaire (including urologists with no case to report), overall had 987 cases in 3 years which means 3.39 cases each year. We can calculate that our responding urologists from all different parts of Iran, on average have seen one PF patients every 3.5-month in the last 3 years.
The Worst and Best Analysis of our data was done to calculate the incidence of PF. In the best analysis of data we assumed that all PF cases which reported by respondent urologists are the whole cases which founded in the residence area of reporters and the non-respondents had no PF cases to report; so the denominator of annual incidence rate are equal to total at risk population (male population) during a report year and the nominator of incidence rate are equal to reported number of PF cases. In worst analysis we assumed that the data of no respondent urologists were missed and also we assumed an equal number of populations of catchment area of each urologist in each province and divided the population of each province between urologists practicing in that province equally. Therefore, after calculating the rate of PF for respondents we generalized it to other urologists of each province by direct adjustment method and determined the estimated incidence rates. Finally, the incidence rate in 100,000 and 175,000 at risk population were calculated by multiplication of calculated incidence rate to 100,000 and 175,000 respectively. Calculating the incidence in every 175,000 population was done to make it easier to compare with incidence in US which is one for every 175,000 males.
With lack of better and more reliable source of data, it is reasonable to assume that real number of cases is a number between worst and best estimates. Also, we can estimate that the real number is closer to lower end, since the urologists with higher number of cases probably had higher chance to respond to this questionnaire. This means incidence of PF in Iran can be estimated between 1.14 to 10.48 per 100,000 male populations (very possible closer to lower end). Also, the incidence is by no mean uniform and Province of Kermanshah has the highest rate, with low rates in many other parts.
Etiology
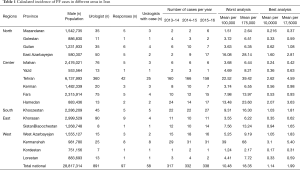
Common causes of PF are intercourse, masturbation, rolling over in bed, forced flexion to achieve detumescence and some other sporadic causes (14). ‘Woman on top” position poses the greatest risk to PF, although no systematic review has corroborated this (15). Patients sometimes report that they were having sexual relations on a desk (with the patient on top) and the penis slipped out, hitting the edge of the desk. It seems that there is geographical variation in its etiology distribution (16). Patients ‘kneading and snapping’ the erect penis to achieve rapid detumescence in unsuitable situations, is another cause in Middle East countries (7,17). This is called “Taqaandan”. a common practice in Province of Kermanshah in Western Iran. A report from Zargooshi et al. indicated that in 269 of 352 (76%) patients, “Taqnaadan” was the cause of PF (12). The common cause of PF in Iranian publications are: sexual intercourse (17.9–89%), masturbation (11–73.8%), and trauma (8.3–28.5%) (6,11,13,18). In our survey, the most common etiologies among all 620 reported cases with known etiologies in the last 3 years were: intercourse in 350 cases (56%), non-intercourse trauma in 146 (24%), masturbation in 108 (17%), and other causes in 16 (3%) cases.
Table 2 show complementary data on etiology of PF in Iran.
Full table
Clinical manifestations
The clinical presentation of PF is often fairly straightforward. Diagnosis is made based on history and physical examination findings (19). PF is characterized by sudden cracking or popping sound, pain and immediate detumescence. Local swelling and discoloration of the penile shaft occurs and may extend to the lower abdominal wall. The ruptured tunica may be palpable. Patients may report minimal to severe sharp pain, depending on the severity of injury. Upon physical examination, penile injury is self-evident (15). In a typical PF, the normal external penile appearance is completely obliterated because of significant penile deformity, swelling, and ecchymosis (the so-called “eggplant” deformity, Figure 2) (9).

Shafi et al. reported that the most common manifestations of PF are penile pain (35.7%), hematoma (29.8%) and edema (11.9%) (6). They also reported that the average time lag between fracture and arriving to the hospital was 5.9 hours. Fracture of corpus covernosum in their series of 76 patients was right sided in 59.5%, left sided in 29% and both sides in 11.5% (6). In a study in Western Iran, the author reported the site of injury was in the right corpus cavernosum in 65 (71.4%) and in the left corpus cavernosum in 26 (28.5%) cases (20). Ahmadnia et al. showed that the most common site of injury found with explorative surgery was the right side (55%) and lateral aspect (74%) of the corpus cavernosum (11). Moslemi reported that the time from injury to presenting to hospital was variable from 3 to 72 hours and all patients presented with the typical clinical picture of a characteristic “pop” sound at the time of injury, pain, detumescence and moderate to severe hematoma. Physical examination revealed penile swelling, ecchymosis and significant tenderness on palpation of the penile shaft. Penile deviation was evident in 82 cases (95.4%). The site of injury was in: right side in 48 cases (59%) and left side in 32 cases (39%), and in 2 cases (2%) rupture was bilateral (13).
In our study, 531 patients presented for treatment within the first 24 hours and 190 patients after 24 hours. In this study, patients’ clinical manifestations were pain, swelling and discoloration in 354 cases, pain and swelling in 183 cases, isolated pain in 184 cases, hematuria in 18 cases and impotency in 7 cases. The reported complications of PF were: chordee in 72 patients (10%), Peyronie’s plaque in 2 (0.2%) and impotence in 44 patients (6%).
Diagnosis
Amer et al. in a meta-analysis study mentioned that thirty-one authors used no imaging to diagnose PF, emphasizing that an accurate diagnosis is possible based on clinical assessment alone. Meanwhile, 22 authors used various imaging modalities to confirm the diagnosis including: ultrasonography study (USS) (21), cavernosography (22), retrograde urethrography (23) and Magnetic Resonance Imaging (MRI) (22). European Association of Urology (EAU) guidelines suggest that imaging (USS or MRI) may be useful in diagnosing PF (3). Moreno Sierra et al. (24) emphasized that complementary tests were helpful, but they were not definitive. In clinical examination, ecchymosis and swelling of penis and difficult voiding in patient suggest urethral rupture due to PF and in suspicious cases urethra should be evaluated by urethrography (25). The swollen, ecchymotic phallus often deviates to the side opposite the tunica tear because of hematoma and mass effect. The fracture line in the tunica albuginea may be palpable (1). Given that urethral injury occurs frequently, preoperative urethrography should be considered when urethral injury is suspected. However, because urethrography can be time-consuming and inaccurate, intraoperative flexible cystoscopy is now often performed routinely just before catheter placement at the time of penile exploration whenever urethral injury is suspected (1). The typical history and clinical presentation of PF usually makes adjunctive imaging studies unnecessary. However, when the history and physical examination are equivocal for PF, ultrasonography can establish the diagnosis (26). Ultrasonography has become the preferred imaging study to evaluate PF because it is rapid, readily available, noninvasive, inexpensive, and accurate. Penile ultrasound is most useful for ruling out fracture in patients with low clinical suspicion (27).
Shariat et al. in a case series report in Shiraz evaluated the role of ultrasound in diagnostic aid of PF. They concluded that ultrasound is a reliable modality to detect the presence and site of tear in the tunica albuginea and can also help with the correct diagnosis in difficult cases with atypical history or presentation (2).The penis is an ideal structure for imaging by ultrasonography. It does not contain bone or air, which impedes sound waves, and it is readily accessible. The sharp tissue interfaces between the corpora and tunica albuginea can be shown clearly with sonography. In ultrasound, the paired corpora cavernosa, the cavernosal arteries, the tunica albuginea and the corpus spongiosum are easily identified. The corpora cavernosa are of uniform hypoechoic reflectivity and the tunica can be seen as an echogenic envelope surrounding the corpora. Corpus spongiosum is of higher echogenicity. Ultrasound is able to detect the site of the tear as an interruption of the echogenic line of the tunica albuginea (28). In two studies in Western Iran, ultrasonography was not used for diagnosis. Diagnosis was made based on clinical presentations, suggesting that typical history and physical findings rarely warrant further radiographic studies, such as sonography, considering its false negative results and operator dependency. Magnetic resonance imaging is another diagnostic tool which is accurate but expensive (12,20). Ahmadnia et al. made their diagnosis by history and clinical examination. Urethral injury was detected by retrograde urethrography in 4 patients (3%) who had macroscopic hematuria and urethrorrhagia. They suggested that there is no need to perform retrograde urethrography unless the patients have gross hematuria or urethrorrhagia. They concluded that key to success in treatment of PF is to achieve a rapid diagnosis based on history and a physical examination, avoid unnecessary imaging tests and perform immediate surgery to reconstruct injury site (11). Moslemi also made diagnosis using history and physical examination in all patients (13).
Other options for diagnosis of PF and the extent of concomitant injury are MRI, cavernosography and urethrography which are not used in most of the patients because of being time consuming and difficulty in access to the operator for imaging and also because of the cost. In a study by Mydlo et al., the cavernosography findings were falsely negative in 28.5% of PF patients (29). In another study done in Qatar, ultrasound had a false negative result in two out of 12 patients with PF (17%) (30). Retrograde urethrography should be performed if urethral injury is suspected based on the presence of blood at the meatus, hematuria of any form, dysuria, or urinary retention. Ultrasound scan should be able to detect possible urethral injury, however in presence of clinical suspicion for urethral injury and a normal ultrasound scan, retrograde urethrography should still be performed (2). Cavernosography is discouraged in the evaluation of a suspected PF because it is time-consuming and unfamiliar to most urologists and radiologists (2). Although MRI has been reported to be a noninvasive and accurate option to detect disruption of the tunica albuginea (31) and can detect corpus cavernosum fracture depicted by the discontinuity of the low signal tunica albuginea (32), it has not been employed widely for the evaluation of patients with symptoms and physical findings suggestive of PF. In our unpublished study of 357 patients, ultrasonography was performed in 62 cases (17%), MRI in 22 (6%) cases and urethrography in 12 (3%) of the patients. Rest of the patients (74%) had no diagnostic study before the surgical procedure.
Management
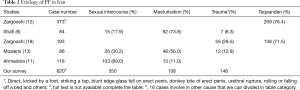
Majority of authors suggest urgent surgical treatment, to decrease the duration of hospitalization and surgical complications such as penile deformity and erectile dysfunction (Figure 3) (1). Multiple contemporary publications recommend that suspected PFs be promptly explored and surgically repaired (33).
The distal circumcising incision may be appropriate when the location of the fracture is uncertain because it provides exposure to all three penile compartments. Closure of the tunical defect with interrupted 2-0 or 3-0 absorbable sutures is recommended. Deep corporeal vascular ligation and excessive debridement of the delicate underlying erectile tissue should be avoided (1). European Urological Association (EAU) guidelines suggest that subcutaneous hematoma, without associated rupture of the cavernosal tunica albuginea does not require surgical intervention. Nonsteroidal analgesics and ice-packs are recommended. Intra-operative flexible cystoscopy is useful to diagnose urethral injury and to further localize urethral damage. Conservative management of penile fracture is not recommended (15). Ahmadnia performed surgery for his patients and rupture of tunica albuginea was sutured with non-absorbable (3/0 nylon) sutures and the knots were placed on the internal surface (continuous method). Several months follow up of his patients showed no complication (11). In a study in Western Iran, patients underwent immediate operation or surgery was delayed until the next morning. Surgical treatment consisted of a degloving circumferential incision of the penile skin, evacuation of the hematoma, control of hemorrhage, and debridement and closure of the defect in the tunica albuginea with a running or interrupted, inverted-knot 2 or 3-0 nylon suture. He showed that there were no significant intraoperative or immediate postoperative complications, and most patients were discharged home first day after surgery. He suggested that delay in surgery until the next morning did not result in any difficulty in surgical dissection or postoperative course (20). Similarly, other studies also suggested that, although surgery is better than conservative management, surgical delay of up to 7 days after the injury does not adversely affect the results of repair (27,34). Safarinjad et al. investigated the impact of immediate surgical repair and conservative treatment of PF on penile vascular indices in 146 surgically treated (group 1), and 56 conservatively treated patients (group 2). All participants underwent penile duplex Doppler ultrasonography, and Doppler parameters were measured. They concluded that current method of surgical treatment does not provide better outcome in terms of erectile function and penile vascular hemodynamics (35). In another study in Western Iran, Zargooshi evaluated the long-term outcome of PF. His patients operated upon using a degloving incision. Ten patients had venous injury and 352 had PF. In the follow up visits, in addition to answering the questionnaire, the patients completed the International Index of Erectile Function (IIEF), Erection Hardness Grading Scale (EHGS), and Global Self-Assessment of Potency (GSAP). He showed that postoperatively, almost all patients developed a permanent, inconsequential, fibrotic nodule and his time -tested approach provided excellent long term sexual function (12). Moslemi performed surgical repair in his all 86 cases, using 4/0 Prolene non-absorbable or 4/0 Vicryl absorbable continuous sutures, for closure of tunica albuginea in longitudinal direction and 4/0 chromic sutures, for closure of the skin in running fashion. He showed that almost all patients were able to achieve full erection with a straight penis. In two patients (2.3%), mild curvature and pain during erection was reported. He did not report early complications in patients for a median follow-up of 6 months (13). Asgari et al. conducted a study on 68 patients who underwent urgent surgical repair anywhere from 3 hours to 4 days after PF. He showed that of 32 patients who completed a questionnaire after surgery, functional results were excellent in all except 3 (9%), who developed penile curvature and pain during coitus. In all of these three patients surgery was done more than 48 hours after injury (10). In our survey from 59 responding urologists study, 42 (71%) urologists suggested emergency surgery for PF, 13 (22%) recommended delayed surgery in the next morning, and four (7%) suggested conservative management. In this series, 468 cases were treated by corporal repair, 22 cases needed both corporal and urethral repair and 26 cases were treated with conservative management.
Conclusions
We reviewed all the available literature on penile fracture in Iran. We also performed a questionnaire-based study with sending questionnaires by emails to 700 urologists throughout Iran to collect more accurate data about the epidemiology, etiology, diagnosis, complications, management and consequences of penile fracture in Iran. We found that the incidence of PF varies significantly in different parts of Iran. Western province of Kermanshah has a significantly higher rate of PF (3.1 to 39 cases per 100,000 male populations). The higher rate of PF in the Province of Kermanshah can be related to lack of sexual education and the practice of “Taqnaadan”, to hear a snap sound from erected penis, which made its incidence higher than other parts of country. Adding data from different regions of Iran, we calculated that incidence of PF in Iran can be estimated between 1.1 to 9.9 per100,000 male population (most probably closer to lower end). Urologists practicing in Iran on average may encounter a PF patient every 3.5 months.
To diagnose PF, majority of reviewed studies and also our responded urologists relied on history and physical examination did not recommend imaging, except for, in patients with possible urethral injuries. They also concluded that immediate surgical intervention can make good functional results with low morbidity and short hospital stay. Delayed surgical intervention and observational management approaches need large population studies with long term follow up.
Acknowledgements
We appreciate Dr. Abtin Heidarzadeh (Guilan University of Medical Science) who did statistical analysis, M.A. Hosseini (Qazvin University of Medical Sciences), M. Khorsand and P. Fazilat who cooperated to collect our study survey.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- McDougal WS, Wein AJ, Kavoussi LR, et al. Campbell-Walsh Urology 10th Edition Review: Elsevier Health Sciences; 2016.
- Shariat M, Sufian M. Role of Ultrasound in Diagnostic Aid of a Case of Penile Fracture. Shiraz E Medical Journal 2008;9:158-62.
- Lee SH, Bak CW, Choi MH, et al. Trauma to male genital organs: a 10-year review of 156 patients, including 118 treated by surgery. BJU Int 2008;101:211-5. [PubMed]
- Bryk DJ, Zhao LC. Guideline of guidelines: a review of urological trauma guidelines. BJU Int 2016;117:226-34. [Crossref] [PubMed]
- Haas CA, Brown SL, Spirnak JP. Penile fracture and testicular rupture. World J Urol 1999;17:101-6. [Crossref] [PubMed]
- Shafid H, Ramaji A, Kasaeian A, et al. Penile fracture In Babol Shaheed Beheshti Hospital during 1996-2004 Mazandaran Medical Science University Journal 2005;15:47-9. [In Persian].
- Ateyah A, Mostafa T, Nasser TA, et al. Penile fracture: surgical repair and late effects on erectile function. J Sex Med 2008;5:1496-502. [Crossref] [PubMed]
- Mahapatra RS, Kundu AK, Pal DK. Penile Fracture: Our Experience in a Tertiary Care Hospital. World J Mens Health 2015;33:95-102. [Crossref] [PubMed]
- Penile Fracture and Trauma Treatment & Management. Available online: http://emedicine.medscape.com/article/456305-treatment
- Asgari MA, Hosseini SY, Safarinejad MR, et al. Penile fractures: evaluation, therapeutic approaches and long-term results. J Urol 1996;155:148-9. [Crossref] [PubMed]
- Ahmadnia H, Younesi Rostami M, Kamalati A, et al. Penile fracture and its treatment: is retrograde urethrograghy necessary for management of penile fracture? Chin J Traumatol 2014;17:338-40. [PubMed]
- Zargooshi J. Sexual function and tunica albuginea wound healing following penile fracture: An 18-year follow-up study of 352 patients from Kermanshah, Iran. J Sex Med 2009;6:1141-50. [Crossref] [PubMed]
- Moslemi MK. Evaluation of epidemiology, concomitant urethral disruption and seasonal variation of penile fracture: A report of 86 cases. Can Urol Assoc J 2013;7:E572-5. [Crossref] [PubMed]
- Amer T, Wilson R, Chlosta P, et al. Penile Fracture: A Meta-Analysis. Urol Int 2016;96:315-29. [Crossref] [PubMed]
- Salonia A, Eardley I, Giuliano F, et al. European Association of Urology guidelines on priapism. Eur Urol 2014;65:480-9. [Crossref] [PubMed]
- Reis LO, Cartapatti M, Marmiroli R, et al. Mechanisms predisposing penile fracture and long-term outcomes on erectile and voiding functions. Adv Urol 2014;2014:768158. [Crossref] [PubMed]
- Jack GS, Garraway I, Reznichek R, et al. Current treatment options for penile fractures. Rev Urol 2004;6:114-20. [PubMed]
- Zargooshi J. Trauma as the cause of Peyronie's disease: penile fracture as a model of trauma. J Urol 2004;172:186-8. [Crossref] [PubMed]
- Agarwal MM, Singh SK, Sharma DK, et al. Fracture of the penis: a radiological or clinical diagnosis? A case series and literature review. Can J Urol 2009;16:4568-75. [PubMed]
- Zargooshi J. Penile fracture in Kermanshah, Iran: report of 172 cases. J Urol 2000;164:364-6. [Crossref] [PubMed]
- Rivas JG, Dorrego JM, Hernández MM, et al. Traumatic rupture of the corpus cavernosum: surgical management and clinical outcomes. A 30 years review. Cent European J Urol 2014;67:88-92. [PubMed]
- Thompson RF. Rupture (fracture) of the penis. J Urol 1954;71:226-9. [PubMed]
- Uygur MC, Gülerkaya B, Altuğ U, et al. 13 years' experience of penile fracture. Scand J Urol Nephrol 1997;31:265-6. [Crossref] [PubMed]
- Moreno Sierra J, Garde Garcia H, Fernandez Perez C, et al. Surgical repair and analysis of penile fracture complications. Urol Int 2011;86:439-43. [Crossref] [PubMed]
- Fergany AF, Angermeier KW, Montague DK. Review of Cleveland Clinic experience with penile fracture. Urology 1999;54:352-5. [Crossref] [PubMed]
- Koifman L, Barros R, Júnior RA, et al. Penile fracture: diagnosis, treatment and outcomes of 150 patients. Urology 2010;76:1488-92. [Crossref] [PubMed]
- El-Assmy A, El-Tholoth HS, Abou-El-Ghar ME, et al. False penile fracture: value of different diagnostic approaches and long-term outcome of conservative and surgical management. Urology 2010;75:1353-6. [Crossref] [PubMed]
- Dierks P, Hawkins H. Sonography and penile trauma. J Ultrasound Med 1983;2:417-9. [PubMed]
- Mydlo JH, Hayyeri M, Macchia RJ. Urethrography and cavernosography imaging in a small series of penile fractures: a comparison with surgical findings. Urology 1998;51:616-9. [Crossref] [PubMed]
- Shamsodini A, Prasad V K, Salman M, et al. Fracture Penis – The Qatar Experience. The Middle East Journal of Emergency Medicine 2003;3:39-42.
- Fedel M, Venz S, Andreessen R, et al. The value of magnetic resonance imaging in the diagnosis of suspected penile fracture with atypical clinical findings. J Urol 1996;155:1924-7. [Crossref] [PubMed]
- Uder M, Gohl D, Takahashi M, et al. MRI of penile fracture: diagnosis and therapeutic follow-up. Eur Radiol 2002;12:113-20. [Crossref] [PubMed]
- Mazaris EM, Livadas K, Chalikopoulos D, et al. Penile fractures: immediate surgical approach with a midline ventral incision. BJU Int 2009;104:520-3. [Crossref] [PubMed]
- Kozacioglu Z, Degirmenci T, Arslan M, et al. Long-term significance of the number of hours until surgical repair of penile fractures. Urol Int 2011;87:75-9. [Crossref] [PubMed]
- Safarinejad MR, Lashkari MH, Babaei A, et al. Penile vascular indices in surgically treated and conservatively treated penile fracture: does conventional immediate repair matter? Int Urol Nephrol 2012;44:1631-40. [Crossref] [PubMed]