A perspective on sperm DNA fragmentation
The paper on sperm DNA fragmentation by Ashok Agarwal et al. summarizes the currently available DNA fragmentation tests and discusses the role of sperm function tests in the intracytoplasmic sperm injection (ICSI) era (1). The authors have summarized the clinical utility of sperm DNA fragmentation test and have provided recommendations based on specific clinical practice scenarios.
We, however, have reservations regarding the precise clinical utility of these sperm function tests.
Semen analysis remains, even today in 2017, the single most important test in evaluating male infertility, despite its poor positive predictive value and even poorer negative predictive value. Nevertheless, numerous other tests, which have been introduced in the last 6 decades to complement, supplement, and replace semen analysis have proven to be even more inadequate.
Semen analysis, as a routine part of infertility evaluation, was first introduced only in the early 20th century (2). Normal or reference semen values have never been convincingly established. The WHO Laboratory Manual for the Examination and Processing of Human Semen (5th edition, 2010) was the first attempt to standardize semen variables based on evidence. This approach is patchy, inadequate, and not representative of the world population (3).
Much before the WHO 2010 manual, one of our PhD students, Dr. Kamaraj, worked to establish Nomo gram for fertility in South Indian men (4). The study conclusions were drastically different from WHO 1999-4th edition. There is no sperm concentration, motility, or morphology values, above which pregnancy is certain, nor below which pregnancy is impossible. The exceptions to this statement are absolute azoospermia, total asthenozoospermia, total teratozoospermia, or total necrozoospermia. Most of these are rare in occurrence. Even today, we do not know the sperm concentration or total sperm count necessary for in vivo conception. Donor insemination studies have clearly shown that in fertile women, conception is possible even with values as low as 2.5 million/mL of motile spermatozoa (5).
Fertility, after all, is a joint effort of two people—man and woman. Sub-fertility of either of the partner may be compensated by normal or super fertility of the other (6).
Sperm function tests—from one unknown to more unknown
As many andrologists felt that semen analysis is an inadequate indicator of male fertility, sperm function tests were introduced to evaluate the potential for male fertility (7). The sperm cervical mucus interaction test is one of the earliest tests to evaluate sperm function (8). The first few editions of the WHO manual carried details about sperm cervical mucus interaction tests, the slide test, capillary tube test etc. (8-11), as cover page features. However, the use of these tests seem to have died a natural death.
Post coital test
The post coital test is an unaesthetic test; it was introduced to study sperm cervical mucus interaction. This test is now sparingly used and remains unproven (12). Tests for anti-sperm antibodies, like MAR and immunobead tests, have been used in the investigation of the infertile male (13). Nancy Alexander raised an issue about this test in an opinion page (14). The use of this test seems to have gone out of fashion.
Hamster egg penetration test (15), Hemi zona assay (15), etc.
With the advent of IVF on a large scale, these tests were introduced claiming that they would predict pregnancy rates both in vivo and in vitro. After a decade of practising these tests, we woke up to realize that these tests would not predict pregnancy outcome both in vivo and in vitro fertilization.
Hypo osmotic swelling test (HOST)
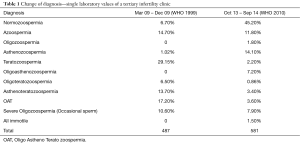
Jeyendran et al. introduced HOST as a test for fertility (16). However, the test remains today only as a useful test for sperm viability, particularly in total asthenozoospermia. Semen analysis is a number’s game (17). Today, we are not even sure about the definition of oligozoospermia (18), asthenozoospermia and teratozoospermia (Table 1). Everything in a semen sample is variable from time to time (11).
Full table
Sperm DNA fragmentation test
The advent of molecular biology and genomics made a quantum change in the management of many medical conditions. Their precise role in infertility, however, remains ill-defined. Genetic analysis is a very useful diagnostic tool in certain conditions (19) (i.e., cystic fibrosis, non-obstructive azoospermia). Its therapeutic and diagnostic roles in other conditions are still under evaluation. A DNA fragmentation test indicates the percentage of spermatozoa in the ejaculate with fragmented DNA. Since DNA is the most crucial component of the cell or spermatozoa, the DNA fragmentation test was believed to indicate the fertility potential of a given semen sample. But unfortunately, we do not know the minimum number of non-fragmented spermatozoa required for in vivo conception. Even in patients with more than 50% spermatozoa carrying DNA fragmentation, the remaining Spermatozoa with non-fragmented DNA would be adequate to effect normal conception (20). After all, only a single normal spermatozoon is required for natural conception (21).
DNA fragmentation occurs as a physiological process in cells undergoing apoptosis (22). With such a huge number of spermatozoa, a certain proportion, say 15%, 30%, 50%, are bound to undergo apoptosis. Therefore, 50% of DNA fragmentation may in fact indicate apoptosis, which is physiological rather than any pathological derangement in the sample. Unless the sample has 100% DNA fragmentation, it may be impossible to call the sample sterile (20).
Tests for DNA fragmentation
There are numerous tests available for evaluating sperm DNA fragmentation (20). The article by Ashok Agarwal et al. gives an excellent summary of all the available DNA fragmentation tests (1). All of them have their own limitations and some of them are quite expensive. It would be naïve for us to introduce these tests into routine clinical practice before we have solid data clearly incriminating sperm DNA fragmentation as a cause for infertility, miscarriages, or IUI, IVF, or ICSI failures. The paper (1) recommends sperm DNA fragmentation testing for specific clinical scenarios, which themselves are debatable.
In a recent article, Erma Z. Drobnis stated that “It (DNA-F testing) remains impossible to recommend its routine use” (23).
Management of sperm DNA fragmentation
Several causative factors have been implicated in producing sperm DNA fragmentation (20). These include varicocoele, smoking, obesity, etc. Varicoceles remain an unproven cause of infertility (24). Smoking needs to be stopped for several reasons besides infertility. Obesity is the Mother of all diseases, and patients should be encouraged to reach their optimum weight, irrespective of their fertility status. Reactive oxygen species (ROS), due to any of other factors or due to inflammation, has been implicated as the cause for sperm DNA fragmentation. ROS is produced in all metabolically active cells and is often a physiological component of the metabolic process. ROS is a physiological cue for apoptosis. Attempts have been made to quench the free radicals by administering antioxidants. Numerous nutraceuticals have been advocated for improving sperm DNA fragmentation, all of which remain unproven in clinical practice (25). It is possible that some of them may even worsen prognosis in some cancer patients (26).
American Society of Reproductive Medicine states that there is insufficient evidence to recommend the routine use of sperm DNA integrity tests in the evaluation and treatment of infertile couples (27). The only usefulness of DNA fragmentation test in infertility would be if we can identify a normal spermatozoon by a non-invasive DNA fragmentation test and thereafter proceed with ICSI procedure using the same spermatozoon. Until then, the current tests remain very useful research tools only. Nothing more, nothing less.
Sperm DNA test and ICSI
With the advent of ICSI, doing the sperm DNA test may turn out to be counterproductive. With a semen analysis report of 50% DNA fragmentation and with no knowledge of which spermatozoon has DNA fragmentation, it is possible that the embryologists may be injecting an abnormal spermatozoon into every other oocyte. In vitro fertilisation would be a better option as it would leave it to the oocyte to choose the right spermatozoon and to repair the minor errors when present. Major genetic errors would end in failed fertilization and hence this may not lead to a pregnancy
Conclusions
Semen analysis is at a crossroads. Andrologists, quite unsatisfied with routine semen analysis, have been trying to introduce newer methods of evaluating a semen sample; this trend has occurred in every decade. With an abundance of spermatozoa in the ejaculate, any test to evaluate a semen sample would remain meaningless, as this only evaluates a portion of the ejaculate. The advent of ICSI has certainly brought about a paradigm change in the management of male infertility and these tests would remain only historical tests until proven otherwise in the years to come. As a medical community, we have been logically illogical several times in the past, with examples such as using immunotherapy for recurrent implantation failure, recurrent pregnancy loss, and hormone replacement therapy in natural menopause. We hope we do not repeat the same mistake with the DNA fragmentation test. Automation gives a sense of false accuracy but not reliability. As Edward E. Wallach once said, “It is easy to fall prey to accepting an unproven therapy as dogma, while overlooking the basic principles responsible for infertility, especially when the overall climate encourages aggressiveness in the use of high-tech measures” (28).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Agarwal A, Majzoub A, Esteves SC, et al. Clinical utility of sperm DNA fragmentation testing: practice recommendations based on clinical scenarios. Transl Androl Urol 2016;5:935-50. [Crossref] [PubMed]
- WHO Laboratory manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction. 1st edition, 1980.
- WHO laboratory manual for the Examination and processing of human semen. Fifth Edition, 2010.
- Kamaraj Thesis on “Establishing a nomogram for semen analysis in South Indian fertile men”. The Tamil Nadu Dr MGR Medical University, Chennai, India.
- Ombelet W. Evidence-based recommendations for IUI in daily practice. Middle East Fertility Society Journal 2013;18:74-7. [Crossref]
- te Velde ER, Bonde JP. Misconceptions about falling sperm counts and fertility in Europe. Asian J Androl 2013;15:195-8. [Crossref] [PubMed]
- Vasan SS. Semen analysis and sperm function tests: How much to test? Indian J Urol 2011;27:41-8. [Crossref] [PubMed]
- Kremer J, Jager S. The sperm-cervical mucus contact test: a preliminary report. Fertil Steril 1976;27:335-40. [Crossref] [PubMed]
- WHO Laboratory manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction. 2nd edition, 1987.
- WHO Laboratory manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction. 3rd edition, 1992.
- WHO Laboratory manual for the Examination of Human Semen and Sperm Cervical Mucus Interaction. 4th edition, 1999. Available online: http://catdir.loc.gov/catdir/samples/cam032/98046890.pdf
- NICE Guidance. Fertility problems assessment and treatment (CG156). Available online: https://www.nice.org.uk/guidance/cg156
- Ford WC, Williams KM, McLaughlin EA, et al. The indirect immunobead test for seminal antisperm antibodies and fertilization rates at in-vitro fertilization. Hum Reprod 1996;11:1418-22. [Crossref] [PubMed]
- Alexander NJ. Treatment for antisperm antibodies: voodoo or victory? Fertil Steril 1990;53:602-3. [Crossref] [PubMed]
- Franken DR, Oehninger S. Semen analysis and sperm function testing. Asian J Androl 2012;14:6-13. [Crossref] [PubMed]
- Jeyendran RS, Van der Ven HH, Perez-Pelaez M, et al. Development of an assay to assess the functional integrity of the human sperm membrane and its relationship to other semen characteristics. J Reprod Fertil 1984;70:219-28. [Crossref] [PubMed]
- Pandiyan N. Semen Analysis—A Numbers Game Chettinad Health City Medical Journal 2012;1:2-3.
- Prathima T, Pandiyan N. Definition of Oligozoospermia—A Commentary. Chettinad Health City Medical Journal 2013;2:108-9.
- World Health Organisation. Classification of cystic fibrosis and related disorders. J Cyst Fibros 2002;1:5-8. [PubMed]
- Smit M, Wissenburg OG, Romijn JC, et al. Increased sperm DNA fragmentation in patients with vasectomy reversal has no prognostic value for pregnancy rate. J Urol 2010;183:662-5. [Crossref] [PubMed]
- Barratt CL, Kay V, Oxenham SK. The human spermatozoon - a stripped down but refined machine. J Biol 2009;8:63. [Crossref] [PubMed]
- Gandini L, Lombardo F, Paoli D, et al. Study of apoptotic DNA fragmentation in human spermatozoa. Hum Reprod 2000;15:830-9. [Crossref] [PubMed]
- Drobnis EZ, Johnson M. The question of sperm DNA fragmentation testing in the male infertility work-up: a response to Professor Lewis’ commentary. Reprod Biomed Online 2015;31:138-9. [Crossref] [PubMed]
- Pandiyan N. Whither varicocelectomy? Chettinad Health City Medical Journal 2014;3:2-3.
- Ranjani S, Benziger A, Pandiyan N. Nutraceuticals in Sperm Abnormalities. Chettinad Health City Medical Journal 2013;2:133-6.
- Chandel NS, Tuveson DA. The promise and perils of antioxidants for cancer patients. N Engl J Med 2014;371:177-8. [Crossref] [PubMed]
- Practice Committee of the American Society for Reproductive Medicine. The clinical utility of sperm DNA integrity testing: a guideline. Fertil Steril 2013;99:673-7. [Crossref] [PubMed]
- Wallach EE. Gonadotropin treatment for the ovulatory patient--the pros and cons of empiric therapy for infertility. Fertil Steril 1991;55:478-80. [Crossref] [PubMed]


