Recurrent urinary tract infections in patients with incomplete bladder emptying: is there a role for intravesical therapy?
Background and etiology
Recurrent urinary tract infections, defined as 3 or greater urinary tract infections (UTIs) in one year, or 2 or more UTIs in six months, are a common and costly public health concern (1). Most of these infections are uncomplicated: they occur in a healthy host in the absence of urinary tract abnormalities. Recurrent uncomplicated UTIs can be addressed with a variety of interventions, such as behavioral modification, self-started antibiotic therapy or short-term suppressive antibiotics, and the majority of these patients can be managed without referral to a specialist (2). As urologists, however, we are often met with recurrent UTIs in patients with underlying structural and functional urologic abnormalities. Patients with incomplete or absent bladder emptying present a particular challenge, as both their pathologic processes and bladder management strategies may increase their susceptibility to infection. In this review, we will discuss the etiology of recurrent UTIs in individuals with impaired bladder emptying, evaluate existing studies regarding UTI prevention strategies in this population, and explore the published experiences with intravesical therapy for the prevention and treatment of recurrent UTIs in patients performing clean intermittent catheterization (CIC).
A variety of etiologies, from benign prostatic hypertrophy to urethral stricture disease, may result in a patient ultimately requiring catheterization for bladder emptying. Most of the published data regarding prolonged catheterization is drawn from patients with neurogenic bladder (NGB). Neurologic conditions leading to lower urinary tract dysfunction are diverse, with the most common being spinal cord injury (SCI), multiple sclerosis, cerebral vascular events and Parkinson’s disease (3). A recent observational study by Manack et al. of over 46,000 patients with a diagnosis of neurogenic bladder highlighted the burden that UTI in this population places on the health care system. In this study, between 29.2% and 36.4% of patients with NGB were diagnosed with lower urinary tract UTI annually. A quarter of patients required an ER visit and a third of patients were hospitalized, 21% of whom carried a diagnosis of UTI during admission. In another recent study, 81% of patients with SCI and NGB were diagnosed with a UTI over a 5-year period. Thirty-five percent of these patients met criteria for recurrent UTI, with 12% having 4 or more UTIs annually (4). Furthermore, sepsis from a urinary source accounts for 10% of mortality in patients with NGB (5). This number, while still high, actually represents a remarkable improvement in outcomes in the modern era: historically, renal failure and sepsis from a urinary source were the leading causes of death in patients following SCI (6).
The etiology of urinary tract infections in the setting of neurogenic bladder is manifold. There are likely alterations in the intrinsic defense mechanisms of the bladder in this setting. Altered vaginal and urethral flora have been noted, with an over-representation of uropathogens (7). A defective glycosaminoglycan layer has also been cited as a possible source for recurrent infections, which may be exacerbated by inflammation and bladder over-distention (8). Immunological impairment has also been postulated, with studies demonstrating deficient mucosal immunity, impaired NK cell, B and T cell function, and defective urothelium that may result in absent apoptosis in response to intercellular signaling (9-11). Bladder ischemia from either over-distension or poor compliance may result in increased risk of infection as adequate blood flow is necessary for host defense mechanisms to function (12). From a mechanical standpoint, impaired washout also increases the risk of UTI. Regular voiding has been shown to be a highly effective mechanism for eliminating bacteria, and multiple studies have shown a correlation between elevated post-void residuals (PVR) and an increased risk of UTI, although the definition of elevated PVR varies widely (13-16). The use of catheters increases the risk of UTI in several ways. Firstly, they negate the protective effect of urethral length on prevention of UTI, specifically in the male. Secondly, they produce chronic inflammation, which may contribute to alterations in defense mechanisms such as the GAG layer (12). Finally, bacterial biofilms may form even in the absence of indwelling catheters (17). Micro-organisms within a biofilm reproduce at a low rate, evading the bactericidal mechanisms of many antibiotic classes, and binding proteins on cell membranes, a common site of antibiotic activity, often have altered expression in this state. The protective extracellular matrix also resists penetration by both antibiotics and host immune mechanisms such as phagocytosis. In vitro studies have shown that bacteria in a biofilm can survive at antibiotic concentrations 1,000–1,500 times higher than planktonic bacteria (18).
Existing strategies for UTI prevention
While we know that altered bladder physiology increases the risk of UTI, demographic and modifiable risk factors for recurrent UTIs in this population are poorly understood. No definitive findings exist regarding correlation between UTIs and hygiene or level of spinal cord injury. There is conflicting evidence regarding gender, and no studies have examined a link between domicile and infection risk (19). CIC, first popularized in this population by Lapides, has been shown in multiple studies to decrease the risk of UTI when compared to indwelling catheters (19,20). Despite the benefits of CIC, bacteriuria still develops in 1–3% of patients per catheterization, and is present in the majority of patients by the third week of bladder management, with E Coli being the dominant species in most studies (21). Specific to the CIC population, low frequency of CIC (<4× daily) and high mean catheterization volumes correlates with increased risk of bacteriuria (22). A recent Cochrane review did not find any evidence that clean versus sterile catheterization, hydrophilic coated catheter versus traditional catheter, or catheterization by self versus other, incurred any benefit in preventing UTI in patients performing CIC (23). Proper self-catheterization technique is extremely important. Studies have demonstrated a reduction in UTIs with the introduction of nurse-led CIC teaching alone (24).
Prophylactic antibiotics and antimicrobial agents to prevent bacteriuria or symptomatic UTI while performing CIC have been met with variable success. Schlager et al. demonstrated half the incidence of symptomatic UTI in children taking nitrofurantoin prophylaxis over 11 months while performing CIC versus those who did not. The prevalence of bacteriuria remained high in both groups (74% of urine sample from placebo group versus 66% of prophylaxis group) (25). A reduction in symptomatic UTIs with nitrofurantoin prophylaxis in the pediatric neurogenic bladder population performing CIC was also noted in a larger study by Johnson (26). A Cochrane review published in 2012 evaluating urinary catheter policies for UTI noted that evidence for the use of prophylactic antibiotics in CIC was inconclusive. When compared to treatment with antibiotics when clinically indicated, only one of three studies analyzed showed a statistically significant difference favoring prophylaxis (27). The urinary antiseptic methenamine, which is used in combination with urinary acidification, was not shown to be beneficial in preventing symptomatic UTI in a recent randomized control trial of patients with neurogenic bladder (28). Similarly, the effectiveness of cranberry products in patients requiring either indwelling or intermittent catheterization have not been established (29).
The cornerstone of managing recurrent UTIs in patients who perform CIC is culture-specific antibiotics. At our institution, low dose antibiotic prophylaxis, such as trimethoprim, concentrated cranberry supplementation or methenamine are initiated on a patient to patient basis taking into account risk factors, species of bacteria cultures, and patient anxiety/motivation. All patients who have underlying urologic or neurologic pathologies and recurrent UTIs would also undergo imaging to rule-out upper tract abnormalities or urolithiasis and urodynamics to assess bladder safety. In particular, we have found that successful treatment of urodynamic abnormalities such as detrusor overactivity or poor compliance frequently causes UTI symptoms to improve or resolve. For individuals without targetable or treatable findings, a trial of single-use catheters is undertaken. In addition, it is important to obtain urine cultures during symptomatic episodes in order to guide antimicrobial therapy. Unfortunately, certain patients will continue to report frequent UTIs, and the repeated courses of antibiotics subject them to adverse events and to the development of resistant organisms. In such situations, intravesical antibiotics may be a useful alternative measure.
Historical and contemporary use of intravesical agents
Instillation of bactericidal solutions into the bladder following catheterization for prevention of UTI dates back to the early 1960s. Interest in this approach was likely generated by its theoretical advantages- bypassing systemic antibiotic side effects and limiting its impact to bladder flora. Paterson first reported using 0.02% chlorhexidine solution in women with urinary retention following gynecologic surgery. In his prospective study, the use of chlorhexidine reduced the risk of postoperative UTI in patients requiring catheterization from 70% to 13.5% (30). Initial reports were encouraging, and multiple studies demonstrated reduced rates of UTI using this method (31,32). Chlorhexidine also compared favorably to alternative bladder irrigation solutions. In a 1978 review, 0.02% chlorhexidine and 0.25% silver nitrate were both found to decrease bacterial counts in urine, while 0.25% acetic acid and normal saline did not substantially impact bacteriuria (33). Chlorhexidine irrigation was also shown to improve the incidence of bacteriuria after transurethral operations. Ball and colleagues demonstrated a statistically significant difference in bacteriuria between a group of patients who received chlorhexidine irrigation following transurethral surgery versus those who did not (12.8% vs. 36.7%) (34). While low serum levels of chlorhexidine were found in some patients, this did not meet the threshold of toxicity and no bladder damage was noted on cystoscopy. Unfortunately, further analysis showed an unacceptable rate of hematuria in patients with long-term use and examination of rat models exposed to intravesical chlorhexidine revealed erosive cystitis (31,35). Reducing the concentration of chlorhexidine prevented cystitis, but yielded insufficient bactericidal activity (36). The discovery of increased bactericidal effects of chlorhexidine with the addition of Ethylenediaminetetraacetic acid (EDTA) allowed for lower concentration to be used in the 1980s. In 1988, Pearman et al. performed a randomized control trial of 18 patients with SCI who used kanamycin/colistin instillations versus Trisdine, a stabilized form of 0.01% chlorhexidine plus EDTA. On statistical analysis Trisdine was found to be non-inferior to kanamycin, with 0.56% and 0.53% of catheterizations resulting in significant bacteriuria respectively (36). Despite its promise in preventing UTI postoperatively and in limited inpatient settings, chlorhexidine irrigation could not eliminate pre-existing symptomatic infection (34). Furthermore, none of these studies assessed long-term use for suppression of UTIs.
Aminoglycoside bladder instillations for prevention of bacteriuria after indwelling catheter placement were first described by Martin and Bookrajian in 1962. In their study, patients underwent continuous neomycin-polymyxin B irrigations while catheterized for an average of 2.7 days, and antibacterial solution did significantly delay the onset of bacteriuria (37). A similarly designed prospective study by Thornton and colleagues involving 33 inpatients who required indwelling catheterization also showed a benefit to neomycin-polymyxin B irrigation in preventing bacteriuria, although this effect was limited to patients with initially sterile urine who were catheterized for less than 10 days (38). However, neomycin-polymyxin B irrigations were not successful in preventing symptomatic UTI in catheterized patients (39). Haldorson reported the use of neomycin irrigation in the setting of intermittent catheterization. In a retrospective case-control study by his group in 1978, 108 adults with acute neurogenic bladder in an inpatient center were given an instillation of 0.1% neomycin after each catheterization. No significant difference in bacteriuria, the end point of the study, was noted between the treatment and non-treatment group (53% vs. 49%, respectively) (40). In 1979, Rhame and Perkash also found non-utility using a mixture of neomycin and polymyxin in the acute setting (41). In a randomized control trial of 33 patients published the following year by Anderson et al., neomycin and polymyxin instillations were shown to incur a significant reduction in bacteriuria, although this effect was only seen in patients performing CIC and instillation of antibiotics 6 times daily versus 3 (42). Serious concerns have been raised regarding the safety of intravesical neomycin, specifically in end-stage renal disease. A case report published in 1993 described the development of perception deafness in a pediatric patient with an augmented bladder and VUR following neomycin irrigations (43). In 1995, Gerharz and colleagues published a case series of three women with end stage renal disease (ESRD) (CrCl <15 mL/min) who developed complete perception deafness, confirmed on audiogram, after undergoing several months of intravesical neomycin irrigations for recurrent UTI. It is noteworthy, however, that at no time in their treatment did these women have serum levels of neomycin tested (44).
Evidence for kanamycin and colistin instillations are similarly limited. Pearman found that the incidence of significant bacteriuria was halved in 47 in-patients with NGB using intravesical instillations of 150 mg kanamycin plus 30 mg colistin after each catheterization versus controls in a prospective study in 1979 (45). Of note, bacteria cultured from patients who had used the antibiotic solution demonstrated significant resistance to both agents. More recently, a randomized trial of perioperative kanamycin instillation in non-infected patients undergoing renal transplant was performed (46). There was a decrease in post-operative UTIs in the treatment group, however it is difficult to generalize this finding to a broader patient population. From a safety standpoint, a study using rats demonstrated ulcerative cystitis and severe irritation with continuous kanamycin and colistin irrigations in 76% of animals intervened upon. This concern does not appear to have been clinically relevant in humans, as no macroscopic hematuria occurred in over 30,000 instillations performed by Pearman’s group (47).
Gentamicin sulfate (GS) is a bactericidal aminoglycoside that was first synthesized from Micromonospora purpurea in 1963 (48). Its mechanism of action is to inhibit protein synthesis at the 30s ribosomal subunit. It is primarily renally excreted and has a half-life of 2–3 hours with parenteral dosing. Common side effects include ototoxicity and nephrotoxicity (49). The use of intravesical gentamicin irrigations for prevention and treatment of recurrent UTIs was first reported by McGuire and Savastono in 1987. Four women with recurrent UTIs and elevated PVRs without a history of neurologic diseases were included in their case series. They initially used 4.8–7.2 mg of gentamicin following each catheterization for a maximum daily dose of 28.8 mg. All urine cultures remained sterile during an average of 42 months of treatment. To evaluate systemic absorption, they performed an animal study using a canine model, and did not show detectable levels of gentamicin even after surgical creation of vesicoureteral reflux (VUR). Lastly, they demonstrated the stability of gentamicin solution at room temperature for at least three weeks by demonstrating stable tube dilution sensitivities when compared with fresh gentamicin solutions (50). Wan et al. expanded upon these findings, specifically regarding the stability and safety of intravesical gentamicin sulfate irrigations. Their study design was tripartite. They first performed animal studies to evaluate absorption of gentamicin in the inflamed bladder. Using a previously designed fulgurated, infected rat bladder model, they showed that, while 43% of animals had detectable serum levels of gentamicin, they all were within a low, non-toxic range (4–12 ng/mL). Repeating this experiment in a canine model, no animals had detectable serum gentamicin levels or changes in creatinine. They subsequently described their findings in humans. In a sample of 10 pediatric patients with neurogenic bladder, three of which had VUR and 3 of which had reconstructions of their urinary tract using bowel, no detectable serum levels or changes in renal function were noted after intravesical use of 14.4–28.8 mg of GS. No resistant organisms were found after treatment, and all had negative cultures at two months. Lastly, in vitro evaluation of the stability and efficacy of gentamicin showed equivalent zones of inhibition of common uropathogens after two months of room temperature storage when compared to fresh solution (51). In 2006, Defoor and colleagues produced the largest prospective series to date. Their study included 80 neurogenic pediatric patients, who underwent intravesical gentamicin irrigations for either long-term suppression after failing oral antibiotics or acute treatment of UTI with an organism resistant to oral antibiotics. Half of these patients had prior urinary tract reconstruction with bowel. Their irrigation protocol was 14.4 mg gentamicin once or twice daily instilled into the bladder after catheterization. Twenty-six percent of their patients had breakthrough infections while on chronic suppression, 24% of whom grew organisms resistant to gentamicin. No breakthrough or persistent infections were seen in the acute UTI treatment group. In terms of safety, no serum gentamicin levels greater than 0.4 ng/mL were found, which is on par with normal trough values. Two patients were noted to have small increases in their creatinine, but both had pre-existing renal dysfunction and these values were thought to be progression of their underlying kidney disease. No electrolyte abnormalities or tinnitus were reported (49). Furthermore, as noted in this study, urine concentrations of 480 µg/mL were achievable with intravesical instillation, which is more than twice that achieved through parenteral administration (50–200 µg/mL) (49). There are few contemporary studies in the adult population. A case series of two women with urinary retention and recurrent UTIs by Van Nieuwkoop using a higher dose of intravesical gentamicin (80 mg daily), showed negative cultures during 8 and 9 months of treatment and no clinical side effects (52). Of note, gentamicin remains the only agent for which substantial series exist in which intravesical therapy was used for treatment of UTI, as all data regarding other antibiotics is limited to individual case reports (53-55).
There are several promising avenues for ongoing research in intravesical therapy for recurrent UTIs. A recent retrospective European trials showed a decrease in UTI recurrence in women undergoing intravesical instillation of hyaluronic acid and chondroitin sulfate (56). The proposed mechanism is restoration of the glycosaminoglycan layer which is disrupted by inflammation. This approach has the advantage of avoiding antibiotic use. The efficacy of this therapy in patients requiring CIC however has not been addressed. Bacterial interference, the introduction of non-virulent bacterial strains to prevent colonization by uropathogens, has also shown promising results. In patients with incomplete bladder emptying, inoculation with E. coli 83972 via catheter incurred both an increase in time to UTI and a decrease in number of UTIs over a 12-month period (57). A subsequent study specifically looking at the role of nonpathogenic E Coli inoculation in the spinal cord population also showed a decrease in UTIs per year (58). One can anticipate that the options for local therapy will expand as our understanding of the interplay between host defenses and the urinary microbiome continues to develop.
Suggested intravesical antibiotic strategy
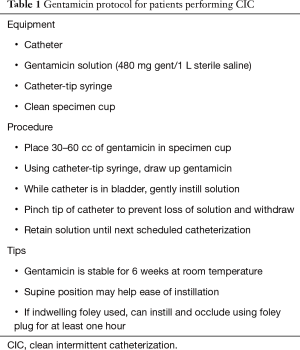
At our institution, intravesical gentamicin irrigation is commonly used in patients who already require CIC and are suffering from either recurrent UTIs or UTIs that are resistant to oral antibiotics. We use a compounded formulation of 480 mg diluted in 1 L normal saline. After the bladder has been drained, 30–60 mL (14.4–28.8 mg) of the solution is instilled in the bladder using gravity, generally at the last catheterization of the evening. The goal is to achieve at least one hour of dwell time. Patient and caregiver instruction regarding technique is led by urology clinic nurses from a standardized education protocol (Table 1). A retrospective review of our experience was recently performed. Twenty-two patients with recurrent UTIs who required CIC were included in our analysis. Each patient was started on a daily regimen of 14.4–28.8 mg of intravesical gentamicin. Prior to initiation of therapy, these patients had a mean of 4 UTIs and 3.5 courses of antibiotics in the preceding 6-month period. After starting gentamicin irrigations, this was reduced to one symptomatic UTI and one course of antibiotics over the same time period. No statistically significant difference in intravenous antibiotic administration, hospitalization or emergency department visits were noted due to low numbers of events, however, there was a decrease in telephone encounters for UTI concerns. Interestingly, multidrug resistant organisms in patients’ urine cultures actually declined overall while on intravesical gentamicin, and no increased resistance to gentamicin itself was seen (59).
Full table
This protocol is typically reserved for patients already performing CIC. Rarely, we will introduce this approach in neurologically intact patient with recurrent UTIs and normal bladder emptying who are willing to catheterize. Anecdotal evidence exists for use in patients with indwelling catheters using catheter plugs, however, the benefits must be weighed against the theoretical risk of sepsis with an occluded indwelling catheter. Twice daily instillation may be used for an acute UTI, and may provide an attractive option in the setting of a multi-drug resistant organisms that would otherwise require intravenous antibiotic use. However, evidence regarding this approach is sparse.
Conclusions
Recurrent UTIs in patients requiring long-term bladder management for incomplete emptying, specifically in those with neurogenic bladder, present a unique challenge to urologists. While many strategies to combat the high incidence of bacteriuria and symptomatic UTI in this population have been studied, the only conclusive data remains the importance of frequent, properly performed CIC. The evidence for use of prophylactic oral antibiotics and antimicrobial agents is conflicting. Series evaluating antibiotic and antiseptic instillations have historically been of poor quality, and concerns regarding safety have arisen. Gentamicin remains the best studied of these agents, and is the only intravesical treatment that has shown efficacy in both the prevention and treatment of urinary tract infections. No systemic side effects have been reported, the solution is stable at room temperature for several months, and development of antibiotic resistance has been minimal. At our institution, it remains a mainstay for combating this difficult problem.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Albert X, Huertas I, Pereiró II, et al. Antibiotics for preventing recurrent urinary tract infection in non-pregnant women. Cochrane database Syst Rev 2004.CD001209. [PubMed]
- Dason S, Dason JT, Kapoor A. Guidelines for the diagnosis and management of recurrent urinary tract infection in women. Can Urol Assoc J 2011;5:316-22. [Crossref] [PubMed]
- Manack A, Motsko SP, Haag-Molkenteller C, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn 2011;30:395-401. [Crossref] [PubMed]
- Biering-Sørensen F, Nielans HM, Dørflinger T, et al. Urological situation five years after spinal cord injury. Scand J Urol Nephrol 1999;33:157-61. [Crossref] [PubMed]
- García Leoni ME, De Ruz AE. Management of urinary tract infection in patients with spinal cord injuries. Clin Microbiol Infect 2003;9:780-5. [Crossref] [PubMed]
- Barber KE, Cross RR. The urinary tract as a cause of death in paraplegia. J Urol 1952;67:494-502. [Crossref] [PubMed]
- Taylor TA, Waites KB. A quantitative study of genital skin flora in male spinal cord-injured outpatients. Am J Phys Med Rehabil 1993;72:117-21. [Crossref] [PubMed]
- Perlow DL, Gikas PW, Horowitz EM. Effect of vesical overdistention on bladder mucin. Urology 1981;18:380-3. [Crossref] [PubMed]
- Vaidyanathan S, McDicken IW, Soni BM, et al. Secretory immunoglobulin A in the vesical urothelium of patients with neuropathic bladder--an immunohistochemical study. Spinal Cord 2000;38:378-81. [Crossref] [PubMed]
- Iversen PO, Hjeltnes N, Holm B, et al. Depressed immunity and impaired proliferation of hematopoietic progenitor cells in patients with complete spinal cord injury. Blood 2000;96:2081-3. [PubMed]
- Schlager TA, Grady R, Mills SE, et al. Bladder epithelium is abnormal in patients with neurogenic bladder due to myelomeningocele. Spinal Cord 2004;42:163-8. [Crossref] [PubMed]
- Vasudeva P, Madersbacher H. Factors implicated in pathogenesis of urinary tract infections in neurogenic bladders: some revered, few forgotten, others ignored. Neurourol Urodyn 2014;33:95-100. [Crossref] [PubMed]
- Cox CE, Hinman F. Experiments with induced bacteriuria, vesical emptying and bacterial growth on the mechanism of bladder defense to infection. J Urol 1961;86:739-48. [Crossref] [PubMed]
- Merritt JL. Residual urine volume: correlate of urinary tract infection in patients with spinal cord injury. Arch Phys Med Rehabil 1981;62:558-61. [PubMed]
- Bakke A, Digranes A, Høisaeter PA. Physical predictors of infection in patients treated with clean intermittent catheterization: a prospective 7-year study. Br J Urol 1997;79:85-90. [Crossref] [PubMed]
- Kim BR, Lim JH, Lee SA, et al. The Relation between Postvoid Residual and Occurrence of Urinary Tract Infection after Stroke in Rehabilitation Unit. Ann Rehabil Med 2012;36:248-53. [Crossref] [PubMed]
- Kai-Larsen Y, Lüthje P, Chromek M, et al. Uropathogenic Escherichia coli modulates immune responses and its curli fimbriae interact with the antimicrobial peptide LL-37. PLoS Pathog 2010;6:e1001010. [Crossref] [PubMed]
- Tenke P, Kovacs B, Jäckel M, et al. The role of biofilm infection in urology. World J Urol 2006;24:13-20. [Crossref] [PubMed]
- Shekelle PG, Morton SC, Clark KA, et al. Systematic review of risk factors for urinary tract infection in adults with spinal cord dysfunction. J Spinal Cord Med 1999;22:258-72. [Crossref] [PubMed]
- Lapides J, Diokno AC, Silber SJ, et al. Clean, intermittent self-catheterization in the treatment of urinary tract disease. J Urol 1972;107:458-61. [Crossref] [PubMed]
- Wyndaele JJ, Brauner A, Geerlings SE, et al. Clean intermittent catheterization and urinary tract infection: review and guide for future research. BJU Int 2012;110:E910-7. [Crossref] [PubMed]
- Bakke A, Vollset SE. Risk factors for bacteriuria and clinical urinary tract infection in patients treated with clean intermittent catheterization. J Urol 1993;149:527-31. [Crossref] [PubMed]
- Prieto JA, Murphy C, Moore KN, et al. Intermittent catheterisation for long-term bladder management (abridged cochrane review). Neurourol Urodyn 2015;34:648-53. [Crossref] [PubMed]
- Barber DB, Woodard FL, Rogers SJ, et al. The efficacy of nursing education as an intervention in the treatment of recurrent urinary tract infections in individuals with spinal cord injury. SCI Nurs 1999;16:54-6. [PubMed]
- Schlager TA, Anderson S, Trudell J, et al. Nitrofurantoin prophylaxis for bacteriuria and urinary tract infection in children with neurogenic bladder on intermittent catheterization. J Pediatr 1998;132:704-8. [Crossref] [PubMed]
- Johnson HW, Anderson JD, Chambers GK, et al. A short-term study of nitrofurantoin prophylaxis in children managed with clean intermittent catheterization. Pediatrics 1994;93:752-5. [PubMed]
- Niël-Weise BS, van den Broek PJ, da Silva EM, et al. Urinary catheter policies for long-term bladder drainage. Cochrane Database Syst Rev 2012.CD004201. [PubMed]
- Lee BB, Haran MJ, Hunt LM, et al. Spinal-injured neuropathic bladder antisepsis (SINBA) trial. Spinal cord Off J Int Med Soc Paraplegia 2007;45:542-50.
- Jepson RG, Williams G, Craig JC. Cranberries for preventing urinary tract infections. Cochrane database Syst Rev 2012.CD001321. [PubMed]
- Paterson ML, Barr W, Macdonald S. Urinary infection after colporrhaphy: its incidence, causation and prevention. J Obstet Gynaecol Br Emp 1960;67:394-401. [Crossref] [PubMed]
- McFadyen IR, Simmons SC. Prevention of urinary infection following major vaginal surgery. J Obstet Gynaecol Br Commonw 1968;75:871-5. [Crossref] [PubMed]
- Gillespie WA, Lennon GG, Linton KB, et al. Prevention Of Catheter Infection Of Urine In Female Patients. Br Med J 1962;2:13-6. [Crossref] [PubMed]
- Bruun JN, Digranes A. Bladder irrigation in patients with indwelling catheters. Scand J Infect Dis 1978;10:71-4. [Crossref] [PubMed]
- Ball AJ, Carr TW, Gillespie WA, et al. Bladder irrigation with chlorhexidine for the prevention of urinary infection after transurethral operations: a prospective controlled study. J Urol 1987;138:491-4. [Crossref] [PubMed]
- Harper WE, Matz LR. The Effect of Chlorhexidine Irrigation of the Bladder in the Rat. Br J Urol 1975;47:539-43. [Crossref] [PubMed]
- Pearman JW, Bailey M, Harper WE. Comparison of the efficacy of “Trisdine” and kanamycin-colistin bladder instillations in reducing bacteriuria during intermittent catheterisation of patients with acute spinal cord trauma. Br J Urol 1988;62:140-4. [Crossref] [PubMed]
- Martin CM, Bookrajian E. Bacteriuria Prevention after Indwelling Cateterization. Arch Intern Med 1962;110:703-11. [Crossref]
- Thornton GF, Lytton B, Andriole VT. Bacteriuria during indwelling catheter drainage. Effect of constant bladder rinse. JAMA 1966;195:179-83. [Crossref] [PubMed]
- Warren JW, Platt R, Thomas RJ, et al. Antibiotic irrigation and catheter-associated urinary-tract infections. N Engl J Med 1978;299:570-3. [Crossref] [PubMed]
- Haldorson AM, Keys TF, Maker MD, et al. Nonvalue of neomycin instillation after intermittent urinary catheterization. Antimicrob Agents Chemother 1978;14:368-70. [Crossref] [PubMed]
- Rhame FS, Perkash I. Urinary tract infections occurring in recent spinal cord injury patients on intermittent catheterization. J Urol 1979;122:669-73. [Crossref] [PubMed]
- Anderson RU. Prophylaxis of bacteriuria during intermittent catheterization of the acute neurogenic bladder. J Urol 1980;123:364-6. [Crossref] [PubMed]
- de Jong TP, Donckerwolcke RA, Boemers TM. Neomycin toxicity in bladder irrigation. J Urol 1993;150:1199. [Crossref] [PubMed]
- Gerharz EW, Weingartner K, Melekos MD, et al. Neomycin-induced perception deafness following bladder irrigation in patients with end-stage renal disease. Br J Urol 1995;76:479-81. [Crossref] [PubMed]
- Pearman JW. The value of kanamycin-colistin bladder instillations in reducing bacteriuria during intermittent catheterisation of patients with acute spinal cord injury. Br J Urol 1979;51:367-74. [Crossref] [PubMed]
- Salehipour M, Salahi H, Fathikalajahi A, et al. Is perioperative intravesically applied antibiotic solution effective in the prophylaxis of urinary tract infections after renal transplantation? Urol Int 2010;85:66-9. [Crossref] [PubMed]
- Harper WE, Matz LR. Further Studies on Effects of Irrigation Solutions on Rat Bladders. Br J Urol 1976;48:463-7. [Crossref] [PubMed]
- Weinstein MJ, Luedemann GM, Oden EM, et al. l. Gentamicin, a New Antibiotic Complex from Micromonospora. J Med Chem 1963;6:463-4. [Crossref] [PubMed]
- Defoor W, Ferguson D, Mashni S, et al. Safety of Gentamicin Bladder Irrigations in Complex Urological Cases. J Urol 2006;175:1861-4. [Crossref] [PubMed]
- McGuire EJ, Savastano JA. Treatment of intractable bacterial cystitis with intermittent catheterization and antimicrobial instillation: case report. J Urol 1987;137:495-6. [Crossref] [PubMed]
- Wan J, Kozminski M, Wang SC, et al. Intravesical instillation of gentamicin sulfate: In vitro, rat, canine, and human studies. Urology 1994;43:531-6. [Crossref] [PubMed]
- Van Nieuwkoop C, den Exter PL, Elzevier HW, et al. Intravesical gentamicin for recurrent urinary tract infection in patients with intermittent bladder catheterisation. Int J Antimicrob Agents 2010;36:485-90. [Crossref] [PubMed]
- Wood GC, Chapman JL, Boucher BA, et al. Tobramycin bladder irrigation for treating a urinary tract infection in a critically ill patient. Ann Pharmacother 2004;38:1318-9. [Crossref] [PubMed]
- Hill DM, Wood GC, Hickerson WL. Linezolid bladder irrigation as adjunctive treatment for a vancomycin-resistant Enterococcus faecium catheter-associated urinary tract infection. Ann Pharmacother 2015;49:250-3. [Crossref] [PubMed]
- Hajjar RR, Philpot C, Morley JE. Continuous bladder irrigation with vancomycin for the treatment of methicillin-resistant Staphylococcus aureus. J Am Geriatr Soc 1996;44:886-7. [Crossref] [PubMed]
- Cicione A, Cantiello F, Ucciero G, et al. Intravesical treatment with highly-concentrated hyaluronic acid and chondroitin sulphate in patients with recurrent urinary tract infections: Results from a multicentre survey. Can Urol Assoc J 2014;8:E721-7. [Crossref] [PubMed]
- Sundén F, Håkansson L, Ljunggren E, et al. Escherichia coli 83972 Bacteriuria Protects Against Recurrent Lower Urinary Tract Infections in Patients With Incomplete Bladder Emptying. J Urol 2010;184:179-85. [Crossref] [PubMed]
- Darouiche RO, Green BG, Donovan WH, et al. Multicenter randomized controlled trial of bacterial interference for prevention of urinary tract infection in patients with neurogenic bladder. Urology 2011;78:341-6. [Crossref] [PubMed]
- Cox L, Bevins J, Clemens JQ, et al. Gentamicin bladder instillations decrease symptomatic urinary tract infections and oral antibiotic use in patients on intermittent catheterization Conference Paper in Neurourology and Urodynamics. In 2015.


