Beyond chemotherapy for advanced disease—the role of EGFR and PD-1 inhibitors
Introduction
Penile cancer is a rare neoplasm in developed nations of Western Europe and the USA, where it represents approximately 0.4–0.6% of all malignancies in men (1). However, the prevalence of penile cancer in developing areas of Africa, Asia and South America is ranging from 6–20 per 100,000 men (2). General socioeconomic status, Human papillomavirus status (HPV), cigarette smoking, access to health care contribute to the discrepancies in this incidence (3). The dominant pathology is squamous cell carcinoma, accounting for 95% of cases. Other malignant tumor types described in published work include basaloid, warty, warty-basaloid, papillary, verrucous, sarcomatoid, adenosquamous and mixed (4).
Most early stage penile cancer will present with lesions affecting the glans and prepuce. Penile preserving surgical techniques are now widely used and result in good functional and cosmetic results (5). However, up to 14% of cases may present as advanced penile cancer in association with extensive inguinal lymph node invasion and 2% patients present with metastasis due to aggressive histological subtype (6). With such advanced disease, surgical treatment may not be effective due to the presence of skin, subcutaneous tissue and vessels invasion by extra nodal disease. There may be little option but to commence palliative systemic treatment as the prognosis is generally very poor. Due to the rarity of penile carcinoma, the peer reviewed scientific literature on the value of systemic treatment is fragmented and the optimal therapy is yet to be determined as studies are generally limited to small single institution retrospective studies. Triplet chemotherapy regimens by adding taxane to cisplatin-based therapy have demonstrated better efficacy in patients with locally advanced or metastatic penile cancer, as indicated by positive findings seen in patients with advanced head and neck squamous cell carcinoma (HNSCC). In a study of 26 patients with advanced penile SCC, the efficacy of a regimen consisting of docetaxel, cisplatin-5-fluorouracil (TPF) was studied. Ten of 26 cases (38.5%) had responded, and 2 patients with locally advanced disease exhibited complete remission. Similarly, another study of 30 cases with advanced penile SCC, patients received neoadjuvant treatment with 4 cycles of paclitaxel, ifosfamide, and cisplatin (TIP). Half of the patients (15/30,50%) had an objective response. Three patients (10%) had a complete pathologic response. The median time to progression (TTP) was 8.1 months, and the median overall survival was 17.1 months. However, the major limitation of this triplet regimen is the extremely high treatment-related toxicity with 65–70% patients experiencing grade 3 or 4 adverse events (7,8). With the development of new strategies including novel targeted therapy and immunotherapy, current treatment paradigms may shift to emphasize the implementation of epidermal growth receptor (EGFR) inhibitors and program death receptor 1 (PD-1) inhibitors in the treatment of advanced or metastatic penile SCC.
Novel targeted therapy: epidermal growth factor receptor inhibitors
The overexpression of EGFR is frequently observed in a variety of epithelial cancers, such as non-small cell lung cancer (NSCLC), HNSCC, colorectal cancer (CRC), and breast cancer (9-11). The expression of EGFR is often assessed by immunohistochemistry (IHC), and the overexpressing is prevalent in patients with penile SCC. In a study of 17 invasive cases, the overexpression of EGFR was examined in all samples, with most showing 3+ overexpression (12). Chaux and colleges assessed the expression of EGFR in 112 patients with the high expression rate was 44%, but the expression was not associated with grade, histologic subtype, or HPV status (13). In a study of 148 penile cancers, Stankiewicz and colleagues investigated the epidermal growth factor receptor (HER) family receptors and in HPV-positive and negative penile SCC and its impact on Akt activation. Differently from EGFR, they found the expression of phosphate-EGFR (p-EGFR) was present in only 25% of penile SCC, and the p-EGFR in tumor with HPV-negative significantly more expressed than HPV-positive cancers (14). The expression of EGFR appeared to be predictive of poor prognosis in a number of malignancies, including non-small-cell lung cancer, oropharyngeal cancer as well as penile cancer. In a study of 30 cases with penile SCC, EGFR expressed was noted in all patients, and positivity for cytosolic p-EGFR were predictive for recurrence and poor survival (15). A recent study from Brazil found EGFR expression in half of the samples which correlated with recurrence. FISH analysis, as determined by signals of the EGFR gene and chromosome 7, revealed the alteration (polysomy and amplification) as an independent risk factor for poor survival (16). Thus, expression of EGFR detected by IHC has been frequently observed in penile SCC, but expression may not correlate well with response.
EGFR mutation is known as an actionable driver mutations in patients with NSCLC, and sensitizing the EGFR mutations play an important role, because of the high prevalence of approximately 10% in Caucasian patients and up to 50% in Asian patients (17-19). EGFR exons 18 to 21 encode a portion of the EGFR kinase domain. It is reported that up of 80% to 90% of patients with EGFR-mutated NSCLC will have either an exon 19 deletion or an L858R point mutation in exon 21 (20-22). It is noted that most mutations involving exons 18, 19, and 21 are considered predictive of sensitivity to EGFR tyrosine kinase inhibitors (TKIs), whereas mutations in exon 20 are typically resistant to these agents (23-25). In penile carcinoma, multiple studies have identified that overexpression of EGFR is not associated with gene amplification, or gene copy number gain. In a study of a series of 20 cases with penile SCC, targeted next-generation sequencing showed EGFR amplification was seen in about 4/20 (20%) patients (26). A recent study performed targeted next-generation sequencing to identify somatic genomic alterations in a cohort of 60 samples from 43 patients and the results showed EGFR expression by IHC does not appear to be correlated with EGFR copy number. The EGFR gains/amplifications accounts for approximately 10% of penile SCC cases, with significant heterogeneity between paired primary tumors and lymph node metastases (27). Moreover, we failed to detect any driver mutations in the tyrosine kinase domain of EGFR, which is known as a predictor of responsiveness in lung cancer (28).
The EGFR-RAS-RAF signaling pathway plays an important role in regulation of tumor cell survival and proliferation, especially in squamous cell carcinoma. The KRAS gene, as a member of the RAS proto-oncogene family, is an important component of the EGFR signaling pathway. KRAS mutations are mostly found in codons 12 and 13, which harbor in exon2. KRAS gene mutation has been recognized as a negative predictor for responsiveness of CRC to cetuximab. However, KRAS mutation has no effect on the overall survival of patients with CRC (29). KRAS mutations were reported to be rare in penile SCC. In a small sample size of 28 cases, Andersson and colleges found 1 mutations in KRAS gene (30). In an analysis of 107 samples from Brazil, only 1 sample presented a mutation in exon 12/13 of KRAS (16). Recently, Gou and colleges analyzed 94 tumor tissues of penile SCC, only 1 case of KRAS mutations at codon 12 was found. Moreover, the RAS-association domain family 1, acted as a tumor suppressor gene through RAS-mediated apoptosis, positively expressed in only 5/150 patients (3.33%) (31). Similarly, KRAS gene mutation was also rare in HNSCCs and was estimated to occur in <3% (32). BRAF is another important component of the EGFR-RAS-RAF signal transduction pathway, which mediates cell growth, differentiation, apoptosis, and malignant transformation. Mutations of BRAF were found in several tumors, such as pilocytic astrocytoma, melanoma, colorectal, thyroid and ovarian cancers (33). The presence of BRAF mutations also very rare in penile SCC. In an analysis of 83 tumors, Gao and colleges found no BRAF V600E point mutation (31).
To date, several EGFR-targeted therapies have been developed and these drugs have been shown in efficacy in several solid tumors, including lung, head and neck and colon. The commercial EGFR-targeted therapies included monoclonal antibodies such as cetuximab, and EGFR tyrosine kinase inhibitors such as erlotinib, and gefitinib. These drugs have been reported to have promising efficacy in some small subset of patients with advanced or metastatic penile squamous cell carcinomas (Table 1).
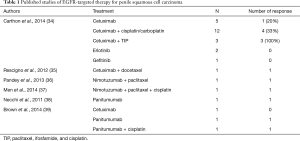
Full table
A retrospective study by Carthon and colleges evaluated the safety and efficacy of EGFR-targeted agents in 24 patients with advanced penile SCC. Eight patients had received an EGFR-targeted drug alone, 13 had received cetuximab plus a platinum or carboplatin, and three patients had received TIP plus cetuximab. The patients with cetuximab with chemotherapy had overall response rate of 30%. Partial responses were seen in 1/5 patients (20%) who had received cetuximab alone, in 3/12 patients (25%) who had received cetuximab plus cisplatin, and in 2/3 patients (66%) who had received cetuximab and TIP. There were no objective responses to the small-molecule inhibitors gefitinib or erlotinib. The overall median TTP was 11.3 weeks, and the median overall survival was 29.6 weeks. The toxicity of EGFR-targeted therapy has been well tolerated, and only 4 cases had the grade 3 or 4 adverse events (34). Similarly, several case reports have also demonstrated the efficacy of other anti-EGFR drugs in addition of cetuximab in the treatment of advanced penile SCC. In a case report, a partial response was seen with the anti-EGFR monoclonal antibody, nimotuzumab, in combination of cisplatin-based chemotherapy (37). In a case report with 3 cases, Brown and colleges reported 2 of the 3 patients had clinical benefit who received cetuximab or panitumumab in the platinum-refractory settings (37). Necchi and colleges reported an experience of using single-agent panitumumab to treat a penile SCC with extensive cutaneous and subcutaneous metastatic nodules. Significant clinical response and rapid recovery of disease related symptoms were observed 2 weeks after the administration (39). Another study summarized cases retrieved from the published studies on using anti-EGFR monoclonal antibodies. Lorenzo and colleges presented a cohort of 28 advanced penile SCC who treated with cetuximab, panitumumab and nimotuzumab. About half patients received the EGFR agent as secondline therapy. Cetuximab was the most commonly used drug, which was administrated in 24/28 patients (85.7%). In the patients who received EGFR-targeted inhibitors plus chemotherapy, over a half of them showed a response to treatment, with a median TTP of 3.2 months. In contrast, patients who received EGFR-targeted inhibitors alone had a response rate of 28.6% and the median TTP of 2.1 months (40).
A number of commercial anti-EGFR agents have been used in patients with penile SCC outside the context of a clinical trial, and these agents seem to have promising efficacy as a salvage treatment after failure of first-line chemotherapy. The current data indicate that patients with penile SCC who received anti-EGFR monoclonal antibodies appear to have better response rate and longer TTP, whereas available anti-EGFR TKIs such erlotinib and gefitinib seem to have no activity, which is likely to be related to the lack of EGFR mutating activation.
Although the vascular endothelial growth factor (VEGF) receptor is overexpressed in approximately 50% of penile SCC cases (41), few studies use these agents in patients with advanced penile SCC. In penile cancers, Stankiewicz and a study of 6 cases, Zhu and colleagues described the experience with VEGF-TKIs after receiving at least 2 prior chemotherapy regimens. One partial response was observed, and 4 patients showed stable disease. Three patients showed pain response and had an improvement in quality of life (42).
Immune checkpoint inhibitors: a new approach to trial design and potential treatment of penile squamous cell carcinoma
Immune checkpoint inhibition with PD-1 and PD-ligand 1 (PD-L1) emerged to play an important role in cancer immunotherapy for a number of cancer phenotypes. The success of immunotherapeutics was previously reported in squamous cell carcinomas of the lung, which led to significant interest in testing similar therapeutic strategies in penile squamous cell carcinoma (43,44).
Recent studies using immunochemical assay to exploit the PD-1/PD-L1 pathway in penile squamous cell carcinoma. The expression of PD-L1 in penile squamous cell carcinoma was reported in three studies (Table 2). The first study reported by Udager found 23 of 37 primary tumors (62.2%) were positive for the PD-L1 expression. Furthermore, the PD-L1 expression of primary tumors was strong positively correlation with usual type histology, regional lymph node metastasis and decreased cancer-specific survival (45). Another study evaluated PD-L1 expression in 200 tumor specimens from a European cohort. At a 1% cut-off level, PD-L1 expressed in 96 primary penile carcinomas (48%) and associated with negative high-risk HPV status. Multivariable analysis revealed PD-L1 expression was independently associated with negative lymph node status and with poor survival. The results were more prominent in men with negative HPV status (46,48). A study access the PD-L1 expression in a North American cohort. Twenty-one (40%) of 53 penile squamous cell carcinomas had positive PD-L1 expression, which was expressed by a significant proportion of advanced penile cancer (47). Thus, 40–60% cases of primary penile SCC express PD-L1, which is associated with negative HPV status, high-risk clinicopathologic features, and poor clinical outcome. Although the sample size of these studies is relatively small, these findings provide a strong rational for the use of checkpoint inhibitors as therapeutic options in penile SCC.
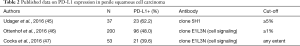
Full table
The FDA approval of the immune checkpoint inhibitors, Ipilimumab, Pembrolizumab and Nivolumab, in metastatic melanoma has led to significant interest in rapid development of clinical trials in penile SCC. Ipilimumab, as a humanized IgG1 monoclonal antibody against cytotoxic T lymphocyte antigen (CTLA-4), has yielded a significant improvement in overall survival in metastatic melanoma. The other two immune checkpoint inhibitors, Pembrolizumab and Nivolumab, are humanized monoclonal antibodies against PD-1, and are approved for use in metastatic melanoma. Several clinical trials were designed to use these immune checkpoint inhibitors to treat penile SCC, and the results of these clinical trials would provide valuable insight to treatment of the aggressive disease. The ongoing clinical trials are phase 2 trial of Pembrolizumab for advanced penile SCC (NCT02837042), and the phase 2 trial for the evaluation of efficacy of Pembrolizumab in rare tumors (NCT02721732). The other two are going to open for recruiting patients, which are phase 2 trial for investigating the efficacy and safety of Nivolumab (NCT03012581) and phase 2 trials of evaluating efficacy of Ipilimuab and Nivolumab for selected rare cancer types (NCT02834013).
Summary
Penile SCC is a rare and lethal disease. In advanced disease, the results, even after aggressive surgical approaches in combination with conventional systemic chemotherapeutic agents, have been disappointing with high recurrence rates and poor survival. High expression of EGFR and the rarity of KRAS mutation make the rational in the use of anti-EGFR inhibitors in advanced penile SCC promising. Anti-EGFR monoclonal antibodies could be used in the neoadjuvant setting to increase radiological responses and in the adjuvant setting to decrease recurrence probability, as well as in the first-line setting in combination with chemotherapy or in more advanced lines of therapy as a single agent. Furthermore, immune checkpoint PD-1 inhibitors have changed the treatment paradigm in a variety of solid tumors. The overexpression of PD-L1 in advanced penile SCC lay biological rational in the potential efficacy of PD-1 inhibitors in this frequently chemo-refractory disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Parkin DM, Muir CS. Cancer Incidence in Five Continents. Comparability and quality of data. IARC Sci Publ 1992.45-173. [PubMed]
- Madsen BS, van den Brule AJ, Jensen HL, et al. Risk factors for squamous cell carcinoma of the penis--population-based case-control study in Denmark. Cancer Epidemiol Biomarkers Prev 2008;17:2683-91. [Crossref] [PubMed]
- Downes MR. Review of in situ and invasive penile squamous cell carcinoma and associated non-neoplastic dermatological conditions. J Clin Pathol 2015;68:333-40. [Crossref] [PubMed]
- Pietrzak P, Corbishley C, Watkin N. Organ-sparing surgery for invasive penile cancer: early follow-up data. BJU Int 2004;94:1253-7. [Crossref] [PubMed]
- Kirrander P, Sherif A, Friedrich B, et al. Swedish National Penile Cancer Register: incidence, tumour characteristics, management and survival. BJU Int 2016;117:287-92. [Crossref] [PubMed]
- Nicholson S, Hall E, Harland SJ, et al. Phase II trial of docetaxel, cisplatin and 5FU chemotherapy in locally advanced and metastatic penis cancer (CRUK/09/001). Br J Cancer 2013;109:2554-9. [Crossref] [PubMed]
- Pagliaro LC, Williams DL, Daliani D, et al. Neoadjuvant paclitaxel, ifosfamide, and cisplatin chemotherapy for metastatic penile cancer: a phase II study. J Clin Oncol 2010;28:3851-7. [Crossref] [PubMed]
- Cassell A, Grandis JR. Investigational EGFR-targeted therapy in head and neck squamous cell carcinoma. Expert Opin Investig Drugs 2010;19:709-22. [Crossref] [PubMed]
- Hirsch FR, Varella-Garcia M, Cappuzzo F. Predictive value of EGFR and HER2 overexpression in advanced non-small-cell lung cancer. Oncogene 2009;28 Suppl 1:S32-7. [Crossref] [PubMed]
- Khelwatty S, Essapen S, Bagwan I, et al. The impact of co-expression of wild-type EGFR and its ligands determined by immunohistochemistry for response to treatment with cetuximab in patients with metastatic colorectal cancer. Oncotarget 2017;8:7666-77. [PubMed]
- Lavens N, Gupta R, Wood LA. EGFR overexpression in squamous cell carcinoma of the penis. Curr Oncol 2010;17:4-6. [PubMed]
- Chaux A, Munari E, Katz B, et al. The epidermal growth factor receptor is frequently overexpressed in penile squamous cell carcinomas: a tissue microarray and digital image analysis study of 112 cases. Hum Pathol 2013;44:2690-5. [Crossref] [PubMed]
- Stankiewicz E, Prowse DM, Ng M, et al. Alternative HER/PTEN/Akt pathway activation in HPV positive and negative penile carcinomas. PLoS One 2011;6:e17517. [Crossref] [PubMed]
- Di Lorenzo G, Perdona S, Buonerba C, et al. Cytosolic phosphorylated EGFR is predictive of recurrence in early stage penile cancer patients: a retropective study. J Transl Med 2013;11:161. [Crossref] [PubMed]
- Silva Amancio AM, Cunha IW, Neves JI, et al. Epidermal growth factor receptor as an adverse survival predictor in squamous cell carcinoma of the penis. Hum Pathol 2017;61:97-104. [Crossref] [PubMed]
- Castellanos E, Feld E, Horn L. Driven by Mutations: The Predictive Value of Mutation Subtype in EGFR-Mutated Non-Small Cell Lung Cancer. J Thorac Oncol 2017;12:612-23. [Crossref] [PubMed]
- Skov BG, Hogdall E, Clementsen P, et al. The prevalence of EGFR mutations in non-small cell lung cancer in an unselected Caucasian population. APMIS 2015;123:108-15. [Crossref] [PubMed]
- Shi Y, Li J, Zhang S, et al. Molecular Epidemiology of EGFR Mutations in Asian Patients with Advanced Non-Small-Cell Lung Cancer of Adenocarcinoma Histology - Mainland China Subset Analysis of the PIONEER study. PLoS One 2015;10:e0143515. [Crossref] [PubMed]
- Maemondo M, Inoue A, Kobayashi K, et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N Engl J Med 2010;362:2380-8. [Crossref] [PubMed]
- Sequist LV, Yang JC, Yamamoto N, et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J Clin Oncol 2013;31:3327-34. [Crossref] [PubMed]
- Wu YL, Zhou C, Hu CP, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol 2014;15:213-22. [Crossref] [PubMed]
- Chiu CH, Yang CT, Shih JY, et al. Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Treatment Response in Advanced Lung Adenocarcinomas with G719X/L861Q/S768I Mutations. J Thorac Oncol 2015;10:793-9. [Crossref] [PubMed]
- Wu JY, Wu SG, Yang CH, et al. Lung cancer with epidermal growth factor receptor exon 20 mutations is associated with poor gefitinib treatment response. Clin Cancer Res 2008;14:4877-82. [Crossref] [PubMed]
- Beau-Faller M, Prim N, Ruppert AM, et al. Rare EGFR exon 18 and exon 20 mutations in non-small-cell lung cancer on 10 117 patients: a multicentre observational study by the French ERMETIC-IFCT network. Ann Oncol 2014;25:126-31. [Crossref] [PubMed]
- Ali SM, Pal SK, Wang K, et al. Comprehensive Genomic Profiling of Advanced Penile Carcinoma Suggests a High Frequency of Clinically Relevant Genomic Alterations. Oncologist 2016;21:33-9. [Crossref] [PubMed]
- McDaniel AS, Hovelson DH, Cani AK, et al. Genomic Profiling of Penile Squamous Cell Carcinoma Reveals New Opportunities for Targeted Therapy. Cancer Res 2015;75:5219-27. [Crossref] [PubMed]
- Di Lorenzo G, Buonerba C, Gaudioso G, et al. EGFR mutational status in penile cancer. Expert Opin Ther Targets 2013;17:501-5. [Crossref] [PubMed]
- Karapetis CS, Khambata-Ford S, Jonker DJ, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med 2008;359:1757-65. [Crossref] [PubMed]
- Andersson P, Kolaric A, Windahl T, et al. PIK3CA, HRAS and KRAS gene mutations in human penile cancer. J Urol 2008;179:2030-4. [Crossref] [PubMed]
- Gou HF, Li X, Qiu M, et al. Epidermal growth factor receptor (EGFR)-RAS signaling pathway in penile squamous cell carcinoma. PLoS One 2013;8:e62175. [Crossref] [PubMed]
- Fujii S, Uryu H, Akashi K, et al. Clinical significance of KRAS gene mutation and epidermal growth factor receptor expression in Japanese patients with squamous cell carcinoma of the larynx, oropharynx and hypopharynx. Int J Clin Oncol 2013;18:454-63. [Crossref] [PubMed]
- Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature 2002;417:949-54. [Crossref] [PubMed]
- Carthon BC, Ng CS, Pettaway CA, et al. Epidermal growth factor receptor-targeted therapy in locally advanced or metastatic squamous cell carcinoma of the penis. BJU Int 2014;113:871-7. [Crossref] [PubMed]
- Rescigno P, Matano E, Raimondo L, et al. Combination of docetaxel and cetuximab for penile cancer: a case report and literature review. Anticancer Drugs 2012;23:573-7. [Crossref] [PubMed]
- Pandey A, Noronha V, Joshi A, et al. Resistant metastatic penile carcinoma and response to biochemotherapy with paclitaxel and epidermal growth factor receptor monoclonal antibody, nimotuzumab. Indian J Med Paediatr Oncol 2013;34:24-7. [Crossref] [PubMed]
- Men HT, Gou HF, Qiu M, et al. A case of penile squamous cell carcinoma treated with a combination of antiepidermal growth factor receptor antibody and chemotherapy. Anticancer Drugs 2014;25:123-5. [Crossref] [PubMed]
- Necchi A, Nicolai N, Colecchia M, et al. Proof of activity of anti-epidermal growth factor receptor-targeted therapy for relapsed squamous cell carcinoma of the penis. J Clin Oncol 2011;29:e650-2. [Crossref] [PubMed]
- Brown A, Ma Y, Danenberg K, et al. Epidermal growth factor receptor-targeted therapy in squamous cell carcinoma of the penis: a report of 3 cases. Urology 2014;83:159-65. [Crossref] [PubMed]
- Di Lorenzo G, Buonerba C, Ferro M, et al. The epidermal growth factor receptors as biological targets in penile cancer. Expert Opin Biol Ther 2015;15:473-6. [Crossref] [PubMed]
- Li D, Han Z, Liu J, et al. Upregulation of nucleus HDGF predicts poor prognostic outcome in patients with penile squamous cell carcinoma bypass VEGF-A and Ki-67. Med Oncol 2013;30:702. [Crossref] [PubMed]
- Zhu Y, Li H, Yao XD, et al. Feasibility and activity of sorafenib and sunitinib in advanced penile cancer: a preliminary report. Urol Int 2010;85:334-40. [Crossref] [PubMed]
- Borghaei H, Paz-Ares L, Horn L, et al. Nivolumab versus Docetaxel in Advanced Nonsquamous Non-Small-Cell Lung Cancer. N Engl J Med 2015;373:1627-39. [Crossref] [PubMed]
- Weber JS, D'Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol 2015;16:375-84. [Crossref] [PubMed]
- Udager AM, Liu TY, Skala SL, et al. Frequent PD-L1 expression in primary and metastatic penile squamous cell carcinoma: potential opportunities for immunotherapeutic approaches. Ann Oncol 2016;27:1706-12. [Crossref] [PubMed]
- Ottenhof SR, Djajadiningrat RS, de Jong J, et al. Expression of Programmed Death Ligand 1 in Penile Cancer Is of Prognostic Value and Associated with HPV Status. J Urol 2017;197:690-7. [Crossref] [PubMed]
- Cocks M, Taheri D, Ball MW, et al. Immune-checkpoint status in penile squamous cell carcinoma: a North American cohort. Hum Pathol 2017;59:55-61. [Crossref] [PubMed]
- Thoma C. Penile cancer: Prognostic value of PD-L1 status. Nat Rev Urol 2016;13:694. [PubMed]


