An objective measurement of urinary continence recovery with pelvic floor physiotherapy following robotic assisted radical prostatectomy
Introduction
Although robotic-assisted laparoscopic radical prostatectomy (RALP) is an overall excellent procedure from an oncological aspect, urinary incontinence (UI) remains a potentially bothersome side effect of the procedure. Historically, post-prostatectomy incontinence has been reported to be as high as 87% at 12 months (1). Surgical technique has however evolved since the previous study to performing nerve-sparing prostatectomies where possible and thus more recently, a large Swedish study reported an incontinence rate of 21.3% following RALP at the same time point (2,3). While the incidence of UI has pleasingly decreased over time, it still has a significant impact on the quality of life following surgery, which partly explains the preference to manage patients on active surveillance where suitable (4). Abraham and colleagues reported that worsening urinary function negatively impacts patient satisfaction post-radical prostatectomy (RP) (5).
The anatomical and physiological mechanisms that are involved in maintaining continence in the male are not entirely understood and hence there are a number of different hypotheses as to how surgery impacts these components. A comprehensive review of the literature and urodynamic results concluded that the male urethral sphincter has two parts and is composed of an inner smooth muscle layer that is more pronounced proximally at the bladder neck and an outer skeletal muscle layer which is more distinct distally at the membranous urethra (6). It is thought that prostatectomy can potentially damage both the smooth muscle sphincter mechanism and the skeletal muscle component. It should be noted that this alone is not responsible for all post-RP UI and other factors such as detrusor overactivity and damage to nerves have a role.
Accordingly, a number of factors have been shown to act as predictors for post-operative continence recovery including pre-operative pelvic floor therapy (7). As a result, pelvic floor physiotherapy has become an important element of post-prostatectomy rehabilitation. A large Italian study demonstrated that early pelvic floor muscle training following RP both significantly improved time to continence recovery with 94.6% of the men who participated in pelvic floor re-training being continent at 6 months following surgery compared to 65% in the control group (8). Interestingly increasing age may delay recovery but overall results are similar (9). Finally laparoscopic versus open or robotic approach may ultimately also be similar although more data are required to demonstrate a superiority related to technique (10).
Whereas the literature in general utilizes subjective measures to assess UI, which are prone to considerable bias, this study aimed to objectively characterize the impact of pelvic floor physiotherapy on recovery of urinary continence following RALP.
Methods
Patient population
A retrospective database was created for consecutive men who underwent a RALP under the care of two senior surgeons between January 2013 and July 2016 and then engaged in a physiotherapist-led pelvic floor rehabilitation program.
Program and data collection
The program commenced pre-operatively and concluded post-op when men were continent. The program involved an initial visit (2–3 weeks pre-surgery) with a pelvic floor physiotherapist (at least 5 years’ experience in the treatment of post RALP incontinence). The initial visit involved education about anatomy, use of ultrasound to demonstrate the pelvic floor musculature and if required a digital rectal exam to assess adequacy of pelvic floor contracture. Patients were then encouraged to practice pelvic floor exercises (PFE) prior to surgery, and to recommence it upon removal of the catheter post-op.
Post-operative visits consisted of counseling, refinement of PFE programs, use of ultrasound to document muscle movement and re-education if required. Patients were instructed to only start measuring their pad weights at week 4 post-op.
Men documented their daily urinary leakage in a diary by recording the weight of their wet pad over a 24-hour period, and subtracting the dry pad weight to determine urine weight. Patients were required to maintain at least two separate 24-hour total urine leakage per week to determine an average for the week. Participants who did not comply with this were excluded from the study.
The average 24-hour urine leakage from each individual’s first week of data collection (week 4 post-op), was considered to be his baseline volume of leakage. Improvement in urinary continence was determined by comparing subsequent weeks’ 24-hour pad weight average to the measurement in that baseline week. Continence is defined in this study as strictly having no leakage, that is, 0 mL on the 24 hours pad-weight test.
Data was also collected regarding medications taken by the patients that may impact bladder function and patients were also monitored for the development of bladder neck contracture.
Statistical analysis
Statistical analysis was carried out using IBM SPSS Statistics (Statistical Package for the Social Science, version 22.0, SPSS Inc., Chicago, Illinois, USA). Difference between groups was calculated using ANOVA. Statistical significance was defined by a P value <0.05.
Results
Forty-five patients with a median age of 63.7 years old met the inclusion criteria for the study and were followed up for a mean of 11.3 weeks post-operatively.
The overall continence rate at 12 weeks post-RP was 38%. Amongst those patients who met the continence definition (n=17), the mean time to continence was 10.5 weeks following surgery.
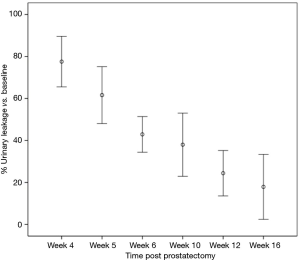
The mean baseline leakage in the cohort was 408.0 mL which then decreased to 324.3, 252.5, 205.8, 157.0 and 110.1 mL at post-operative weeks 4, 5, 6, 10 and 12 respectively. This corresponded to a significant 22.4% (95% CI, 16.5% to 28.3%), 38.4% (95% CI, 31.7% to 45.0%), 57.1% (95% CI, 52.9% to 61.3%) and 75.6% (95% CI, 72.3% to 78.8%) improvement in urinary leakage at the same respective time points (Figure 1).
Three patients were utilizing anticholinergic medication prior to surgery. A single patient from this sub-group ceased their anticholinergic therapy post-RALP but the remaining two continued treatment but at a lower dose. No patients newly commenced anticholinergic treatment post-operatively. No patients in our cohort developed a bladder neck contracture during their follow-up.
Discussion
Our study demonstrates the recovery of urinary continence over time with a 75.6% improvement in leakage 3 months post-RALP with the assistance of a structured pelvic floor physiotherapy program. This is the first study in the literature to tract 24-hour pad weight tests over multiple days and an extended period to assess the recovery of continence in an objective manner. A previous study by Patel et al., has used a single 24-hour pad weight test at 6 weeks and 3 months post-open radical retropubic prostatectomy to assess the impact of pelvic floor physiotherapy on the early recovery of continence (11). They reported that the group who underwent a pre-operative physiotherapist-led program experienced significantly lower leakage at 6 weeks than those who only received verbal instructions by the surgeon. However, there was no difference evident at 3 months suggesting that pelvic floor physiotherapy accelerates the recovery time rather than improving the overall long-term rate.
The absolute pad weights in the aforementioned study is lower than that seen in our study however it should be noted that Patel and colleagues utilized a single measure at the 2 time points. Despite the 24-hour test being the gold standard, it is still subject to variability depending on daily activity levels (12). In contrast, by measuring the mean leakage over the week, we intended to account for variations in daily activity levels and obtain a more accurate measure of leakage over time. Further research could determine which of these is the more valid method of evaluating stress incontinence.
The main strength of this study lies in the objective measure of UI. The quality of research in this field has been affected by the tendency to report numbers of pads as the outcome measure. This has been shown to be a poor measure that is subject to recall bias and has poor correlation to the degree of incontinence. A group from Duke University, USA suggested that self-reported pads per day only accounts for 38% of the variation of UI volume and that the 24-hour pad weight test would be a more reliable measure (13). Furthermore, rather than a 24-hour test which is logistically challenging to perform, other studies have performed a 1-hour test as a compromise. These too have been shown to have a low negative predictive value and require retrograde filling of the bladder to be reproducible (14,15). Our study relied on natural bladder filling, which represents highly objective data of post-prostatectomy UI.
The 38% continence rate seen in our study is comparatively low compared with reports in the literature at the same time point post-RP. However, this is likely a reflection of the strict continence definition in our study where men had to have no leakage to be classified as being continent. In contrast, a large systematic review reported a 65% pooled continence rate at 3 months following RALP (16). It should be noted that the pooled studies had varying definitions of continence and collected data utilizing a questionnaire that is susceptible to bias. Moreover, Malik et al. reported that a single pad corresponded to approximately 72.1 g of measured urinary leakage (17). Therefore, if we included the use of a single pad in our definition of continence as many previous studies have and considered all patients who reported a daily leakage less than 72.1 g as being continent then our continence rate would be substantially greater. A Californian study did however question the classification of a security pad or 0 to 1 pad as being “continent” as there is a significant decrease in the quality of life amongst those who use no pads compared to men who use 0 to 1 pad (18).
In addition, Kadono and colleagues performed a 24-hour pad test prior to RALP and reported a mean of 1.1 g (19). Therefore, since we did not have data on pre-operative urinary leakage, we did not account for men who may have had a small degree of leakage pre-operatively and thus would not be expected to be fully continent post-RALP hence potentially over-estimating our incontinence rate.
Additionally, the importance of a qualified physiotherapist has been highlighted by Patel et al. where the group of men whose pelvic floor rehabilitation was guided by a physiotherapist pre-operatively had superior urinary continence outcomes in regards to duration and severity of UI compared to the control group who was only instructed by the surgeon (11). In contrast, a Dutch group reported that there was no significant recovery of UI between men whose pelvic floor muscle exercises were guided by a physiotherapist compared to those who only received guidance from an instruction folder (15). It should be noted that the aforementioned study was underpowered due to inadequate recruitment and that there was a small favourable absolute difference in continence recovery at 6 months amongst men whom were led by a physiotherapist.
A final point is one of psychology and positive reinforcement. Just as someone who is attempting weight loss may benefit from weighing daily or even weekly with “real-time” achievements able to be processed and help them remain on a plan (20), so too many more intense measuring have a role in men recovering from RALP. Furthermore, the relationships of the patient and even their partners with the physiotherapist and urology nurse specialist has taken on greater importance in recent years and may also aid in the psychological and physical recovery of men (21). Greater study is needed in this area from a psychometric perspective of patient’s recovery profiles.
We acknowledge that our study has a number of limitations including the lack of a control arm to assess the impact of pelvic floor physiotherapy. Furthermore, our results are based on a short follow-up and a relatively small sample size, which is partly explained by the logistical challenge of performing multiple 24-hour pad weight tests over a prolonged time period.
This study continues to highlight the differences in pathways men have after surgery. A lack of consensus guidelines on management serves to remind us of the gaps in the literature to provide high-level evidence on the best pathways to follow (22). This study demonstrates that urinary leakage following RALP considerably improves in the short-term with the aid of pelvic floor physiotherapy. The usefulness of a daily pad weight may assist recovery via positive feedback. However, further research with a control group is required to gauge its true utility.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The article was deemed exempt from ethical review as per Australian NHMRC guidelines.
References
- Jønler M, Madsen FA, Rhodes PR, et al. A prospective study of quantification of urinary incontinence and quality of life in patients undergoing radical retropubic prostatectomy. Urology 1996;48:433-40. [Crossref] [PubMed]
- Haglind E, Carlsson S, Stranne J, et al. Urinary Incontinence and Erectile Dysfunction After Robotic Versus Open Radical Prostatectomy: A Prospective, Controlled, Nonrandomised Trial. Eur Urol 2015;68:216-25. [Crossref] [PubMed]
- Suardi N, Moschini M, Gallina A, et al. Nerve-sparing approach during radical prostatectomy is strongly associated with the rate of postoperative urinary continence recovery. BJU Int 2013;111:717-22. [Crossref] [PubMed]
- Wong LM, Tang V, Peters J, et al. Feasibility for active surveillance in biopsy Gleason 3 + 4 prostate cancer: an Australian radical prostatectomy cohort. BJU Int 2016;117 Suppl 4:82-7. [Crossref] [PubMed]
- Abraham NE, Makarov DV, Laze J, et al. Patient centered outcomes in prostate cancer treatment: predictors of satisfaction up to 2 years after open radical retropubic prostatectomy. J Urol 2010;184:1977-81. [Crossref] [PubMed]
- Koraitim MM. The male urethral sphincter complex revisited: an anatomical concept and its physiological correlate. J Urol 2008;179:1683-9. [Crossref] [PubMed]
- Song C, Doo CK, Hong JH, et al. Relationship between the integrity of the pelvic floor muscles and early recovery of continence after radical prostatectomy. J Urol 2007;178:208-11. [Crossref] [PubMed]
- Filocamo MT, Li Marzi V, Del Popolo G, et al. Effectiveness of early pelvic floor rehabilitation treatment for post-prostatectomy incontinence. Eur Urol 2005;48:734-8. [Crossref] [PubMed]
- Basto MY, Vidyasagar C, Te Marvelde L, et al. Early urinary continence recovery after robot-assisted radical prostatectomy in older Australian men. BJU Int 2014;114:29-33. [Crossref] [PubMed]
- Louie-Johnsun MW, Handmer MM, Calopedos RJ, et al. The Australian laparoscopic non robotic radical prostatectomy experience – analysis of 2943 cases (USANZ supplement). BJU Int 2016;118:43-8. [Crossref] [PubMed]
- Patel MI, Yao J, Hirschhorn AD, et al. Preoperative pelvic floor physiotherapy improves continence after radical retropubic prostatectomy. Int J Urol 2013;20:986-92. [PubMed]
- Rasmussen A, Mouritsen L, Dalgaard A, et al. Twenty-four hour pad weighing test: reproducibility and dependency of activity level and fluid intake. Neurourol Urodyn 1994;13:261-5. [Crossref] [PubMed]
- Dylewski DA, Jamison MG, Borawski KM, et al. A statistical comparison of pad numbers versus pad weights in the quantification of urinary incontinence. Neurourol Urodyn 2007;26:3-7. [Crossref] [PubMed]
- Siltberg H, Victor A, Larsson G. Pad weighing tests: the best way to quantify urine loss in patients with incontinence. Acta Obstet Gynecol Scand Suppl 1997;166:28-32. [PubMed]
- Dubbelman Y, Groen J, Wildhagen M, et al. The recovery of urinary continence after radical retropubic prostatectomy: a randomized trial comparing the effect of physiotherapist-guided pelvic floor muscle exercises with guidance by an instruction folder only. BJU Int 2010;106:515-22. [Crossref] [PubMed]
- Ficarra V, Novara G, Rosen RC, et al. Systematic review and meta-analysis of studies reporting urinary continence recovery after robot-assisted radical prostatectomy. Eur Urol 2012;62:405-17. [Crossref] [PubMed]
- Malik RD, Cohn JA, Fedunok PA, et al. Assessing variability of the 24-hour pad weight test in men with post-prostatectomy incontinence. Int Braz J Urol 2016;42:327-33. [Crossref] [PubMed]
- Liss MA, Osann K, Canvasser N, et al. Continence definition after radical prostatectomy using urinary quality of life: evaluation of patient reported validated questionnaires. J Urol 2010;183:1464-8. [Crossref] [PubMed]
- Kadono Y, Nohara T, Kadomoto S, et al. Investigating Urinary Conditions Prior to Robot-assisted Radical Prostatectomy in Search of a Desirable Method for Evaluating Post-prostatectomy Incontinence. Anticancer Res 2016;36:4293-8. [PubMed]
- McCarthy M. Loss of potential reward is best motivator in workers’ wellness programme, study finds. BMJ 2016;352:i932. [Crossref] [PubMed]
- Couper J, Collins A, Bloch S, et al. Cognitive existential couple therapy (CECT) in men and partners facing localised prostate cancer: a randomised controlled trial. BJU Int 2015;115:35-45. [Crossref] [PubMed]
- Brown B, Young J, Kneebone AB, et al. Knowledge, attitudes and beliefs towards management of men with locally advanced prostate cancer following radical prostatectomy: an Australian survey of urologists. BJU Int 2016;117:35-44. [Crossref] [PubMed]


