Health state utilities among contemporary prostate cancer patients on active surveillance
Introduction
For localized (non-metastatic) prostate cancer, radical treatment, such as surgery and radiation therapy, is often curative but may cause significant side effects such as impotence and urinary problems (1). However, in the era of widespread PSA screening, overdiagnosis is a significant issue (2). Many prostate cancers have a low risk of progression in the absence of treatment and may be managed conservatively.
Conservative management spans a spectrum from watchful waiting (WW), which involves minimal testing and no curative intent, to active surveillance (AS), which involves serial follow-up testing to offer selective delayed treatment to those with increasing disease burden over time. Several comparative-effectiveness models have shown that conservative management is a safe alternative and may reduce initial costs (3-5).
Although upfront conservative management has the potential to delay or avoid the need for treatment and its potential side effects, early studies reported a significant decrement in utility potentially from disease-related anxiety (6). However, over the past decade new data has emerged from large prospective cohort studies showing the long-term safety of AS, with very low rates of metastasis and prostate cancer death (7,8). Correspondingly, the use of AS has rapidly increased in both the United States and internationally (9). The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) registry, which obtains data from urologic practices across the United States, reported that from 2010 to 2013 around 40% of low-risk prostate cancer patients were managed by AS or WW (10).
More recent data has shown a high quality of life among men in contemporary AS programs (11,12). Thus, we hypothesized that health state utilities (quality of life weights) may be different now than prior to the widespread use of AS. Our objective was to perform a systematic review of the published literature on utilities among contemporary AS patients. In addition, we directly examined utilities in an ethnically diverse group of AS patients using both a generic (EuroQol three level questionnaire, EQ-5D-3L) and prostate cancer-specific instrument (Patient ORiented Prostate Utility Scale, PORPUS). The EQ-5D-3L is a generic measure of health that has been validated in cancer patients (13). With only five questions, it has been deemed one of the shortest and least cognitively demanding utility assessment instruments (14). The EQ-5D covers mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The PORPUS was developed by Krahn et al., and validated by Ritvo et al., to create a specific utility measure for prostate cancer patients (15,16). The PORPUS consists of 10 domains related to key dimensions of prostate cancer; pain, energy, social support, communication with doctor, emotional well-being, urinary leakage, sexual function, sexual interest, and bowel problems (14).
Methods
To assess health state utilities in contemporary AS patients, we first performed a systematic search of PubMed, PMC, and Ovid for English-language publications on “utility AND active surveillance”, and “utilities AND active surveillance” from inception through April 2016. We also searched for articles specifically using the EQ-5D and PORPUS instruments in AS populations with the following searches: “PORPUS AND active surveillance”, and “EQ-5D AND active surveillance”. Finally, we searched for “PORPUS and prostate cancer”, and “EQ-5D and prostate cancer” to find any additional articles using these questionnaires that may have included a subset of patients on AS. This search yielded a total of 518 unique results. After excluding based on title (n=500), abstract (n=7) and full-text review (n=11), this search did not find any data using these instruments to measure utilities in a modern AS population.
We addressed this gap in the literature by distributing the EQ-5D-3L and PORPUS to prostate cancer patients on AS from two clinical settings, NYU Langone Medical Center and the Manhattan Veterans Affairs Hospital. These surveys were completed as part of a larger qualitative study on AS that aimed to parse out the educational and informational needs of men on AS. A total of 235 men on AS from both institutions were identified through a query of the electronic health record and mailed invitations to participate in focus groups. Patients were eligible if they met the following criteria: (I) male between 30–89 years old; (II) diagnosed with prostate cancer; (III) had not undergone treatment. We conducted seven focus groups with 37 men on AS from October 2015 to March 2016, until thematic saturation was reached, wherein no new themes emerged. All participants completed both questionnaires prior to the focus group discussion. Descriptive statistics were used to examine the distribution of EQ-5D-3L and PORPUS scores, and a Spearman correlation was calculated between these instruments. Chi-square and Moody’s test were used for statistical comparisons. All statistical analyses were performed using the statistical software package SAS (SAS Institute Inc., Cary, NC, USA). The study protocol was approved by the IRB at New York University School of Medicine and the VA New York Harbor Healthcare System.
Results
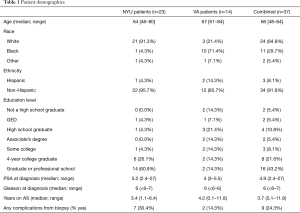
Among the 37 focus group participants, the median age was 66, and racial background was 65% white, 30% black and 5% were of other race/ethnicities (Table 1). Twenty-two percent of participants graduated from a four-year university and 43.2% completed graduate or professional school. The median PSA at prostate cancer diagnosis was 4.9 (range, 2.4–27) and the median Gleason score was 6 (range, ≤6–7). The median length of time on AS at the time of the study was 3.4 years (range, 0.1–11.8 years).
Full table
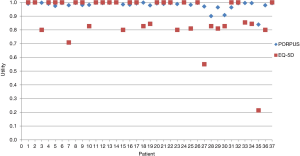
All 37 patients completed the EQ-5D-3L and 36 of the patients completed the PORPUS (Figure 1). The mean score was 0.90±0.16 on the EQ-5D-3L (median, 1.00; range, 0.21–1.00) and 0.98±0.03 on the PORPUS (median, 0.99; range, 0.84-1.00). The correlation between the EQ-5D-3L and PORPUS was 0.87 (P<0.0001), and 14 patients (38%) had a difference >0.1. There was no significant relationship between time on AS and utility scores, and no significant difference in scores between clinical settings. A bivariate analysis suggested no significant correlation between education level and utility score.
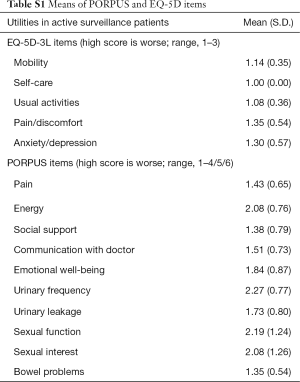
Evaluation of the individual items (Table S1) showed the highest (or most severe) item in the EQ-5D-3L was pain/discomfort (mean 1.35±0.54), followed by anxiety/depression (mean 1.30±0.57). None of the patients reported a decrement in the EQ-5D domain of self-care. In the PORPUS, the highest scores were for urinary frequency (mean 2.27±0.77) and sexual function (mean 2.19±0.80).
Full table
Discussion
Our results demonstrate a high overall correlation in the scores from EQ-5D and PORPUS in contemporary AS patients. However, there was a difference of more than 0.1 in 38% patients, and the most influential domains differed between instruments.
Precise utility estimates are very important for modeling studies of prostate cancer management, which are frequently used to guide clinical care and policy decisions. For example, a recent study by Roth et al. showed PSA screening is cost-effective when used in conjunction with conservative management of low-risk disease (17). In the main analysis, the authors used a utility decrement of 0.08 for “surveillance”, which was varied from 0.02 to 0.14. These utilities were drawn from a 2005 study including 162 men ages ≥60 (of whom 52% were diagnosed with prostate cancer) who were asked about three different watchful waiting states with a varying chance of cancer spreading (6). Although this is similar to the mean utility using the EQ-5D in our contemporary cohort, the PORPUS had a mean utility of 0.98 and only 2 patients had a decrement ≥0.1. In the Roth study, sensitivity analyses showed that model results were most sensitive to the health state utility for the conservative management state (17). These combined findings suggest that the instrument used to assess utilities for AS patients may have a substantial impact on prostate cancer model results.
The PORPUS has more items overall, so each specific item is not weighted as heavily as in the EQ-5D. For example, with all other domains perfect, a 3 for pain (middle category) brings the PORPUS to 0.99, and a 5 (maximum) results in a PORPUS score of 0.77. By contrast, with all other domains perfect, a pain score of 2 (middle score) brings the EQ-5D to 0.83, and a score of 3 (maximum) would result in a EQ-5D of 0.46. Although pain had the highest mean score on the EQ-5D in our patients, it is unclear whether this was related to prostate cancer or due to other comorbid issues. No patients reported a decrement in the self-care domain, suggesting that this item may have limited discriminatory utility in a contemporary AS population.
Meanwhile, PORPUS asks about several disease-specific domains that are not explicitly measured by the EQ-5D. Although the PORPUS also measures pain and anxiety/depression (worst scores in EQ-5D), the highest mean scores were instead for disease-specific urinary and sexual items. Although AS does delay or avoid the potential urinary and sexual side effects of radical treatment, it is important to recognize that it does not prevent the age-related progression of these issues. The prostate is a primary contributor to male lower urinary tract symptoms, and a long-term prospective cohort study of men undergoing radical prostatectomy found that men with significant urinary symptoms prior to surgery actually had an improvement in urinary quality of life postoperatively (18). Acar et al. analyzed quality of life after various forms of prostate cancer treatment, demonstrating an inverse relationship between age and sexual function scores (19). In the subset of men on AS, they also found an increase in the use of incontinence aids over time. Overall, it is important for men choosing AS to recognize that they may still experience declines in urinary and sexual function over time, even in the absence of prostate cancer treatment.
Limitations of our study are that despite a racially diverse population, the sample size was small and these results may not be generalizable to other settings. Also, these utilities were not measured at the time of prostate biopsy, which may have a transient impact on quality of life. Despite these limitations, our systematic review demonstrated there is scant data on validated utility measures among current AS patients and how they may differ based on the instrument that is used. Thus, these preliminary findings provide novel data on utilities among current active surveillance patients, and how they differ using validated generic and disease-specific instruments.
Acknowledgements
Funding: This work was supported by the Blank Family Foundation; the Laura & Isaac Perlmutter NYU Cancer Center (P30CA016087); the Louis Feil Charitable Lead Trust; and the National Cancer Institute at the National Institutes of Health (Award Number K07CA178258). And this work was supported by the COMET Center ONCOTYROL, which is funded by the Austrian Federal Ministries BMVIT/BMWFJ (via FFG) and the Tiroler Zukunftsstiftung/Standortagentur Tirol (SAT).
Footnote
Conflicts of Interest: SL received honoraria for lectures from Astellas, GenomeDx Biosciences, MDx Health and Boehringer Ingelheim, consulting fees from Lilly, and reimbursed travel to conferences from Minomic and Astellas (unrealted to current study).
Ethical Statement: The study protocol was approved by the IRB at New York University School of Medicine and the VA New York Harbor Healthcare System.
References
- Huang GJ, Sadetsky N, Penson DF. Health related quality of life for men treated for localized prostate cancer with long-term followup. J Urol 2010;183:2206-12. [Crossref] [PubMed]
- Loeb S, Bjurlin MA, Nicholson J, et al. Overdiagnosis and overtreatment of prostate cancer. Eur Urol 2014;65:1046-55. [Crossref] [PubMed]
- Hayes JH, Ollendorf DA, Pearson SD, et al. Active surveillance compared with initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA 2010;304:2373-80. [Crossref] [PubMed]
- Liu D, Lehmann HP, Frick KD, et al. Active surveillance versus surgery for low risk prostate cancer: a clinical decision analysis. J Urol 2012;187:1241-6. [Crossref] [PubMed]
- Kim S 2nd, Dall'Era MA, Evans CP. Economic analysis of active surveillance for localized prostate cancer. Curr Opin Urol 2012;22:247-53. [Crossref] [PubMed]
- Stewart ST, Lenert L, Bhatnagar V, et al. Utilities for prostate cancer health states in men aged 60 and older. Med Care 2005;43:347-55. [Crossref] [PubMed]
- Klotz L, Vesprini D, Sethukavalan P, et al. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J Clin Oncol 2015;33:272-7. [Crossref] [PubMed]
- Tosoian JJ, Mamawala M, Epstein JI, et al. Intermediate and Longer-Term Outcomes From a Prospective Active-Surveillance Program for Favorable-Risk Prostate Cancer. J Clin Oncol 2015;33:3379-85. [Crossref] [PubMed]
- Tosoian JJ, Carter HB, Lepor A, et al. Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol 2016;13:205-15. [Crossref] [PubMed]
- Cooperberg MR, Carroll PR. Trends in Management for Patients With Localized Prostate Cancer, 1990-2013. JAMA 2015;314:80-2. [Crossref] [PubMed]
- Bellardita L, Rancati T, Alvisi MF, et al. Predictors of health-related quality of life and adjustment to prostate cancer during active surveillance. Eur Urol 2013;64:30-6. [Crossref] [PubMed]
- Wilcox CB, Gilbourd D, Louie-Johnsun M. Anxiety and health-related quality of life (HRQL) in patients undergoing active surveillance of prostate cancer in an Australian centre. BJU Int 2014;113 Suppl 2:64-8. [Crossref] [PubMed]
- Pickard AS, De Leon MC, Kohlmann T, et al. Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Med Care 2007;45:259-63. [Crossref] [PubMed]
- Krahn M, Bremner KE, Tomlinson G, et al. Responsiveness of disease-specific and generic utility instruments in prostate cancer patients. Qual Life Res 2007;16:509-22. [Crossref] [PubMed]
- Krahn M, Ritvo P, Irvine J, et al. Construction of the Patient-Oriented Prostate Utility Scale (PORPUS): a multiattribute health state classification system for prostate cancer. J Clin Epidemiol 2000;53:920-30. [Crossref] [PubMed]
- Ritvo P, Irvine J, Naglie G, et al. Reliability and validity of the PORPUS, a combined psychometric and utility-based quality-of-life instrument for prostate cancer. J Clin Epidemiol 2005;58:466-74. [Crossref] [PubMed]
- Roth JA, Gulati R, Gore JL, et al. Economic Analysis of Prostate-Specific Antigen Screening and Selective Treatment Strategies. JAMA Oncol 2016;2:890-8. [Crossref] [PubMed]
- Prabhu V, Taksler GB, Sivarajan G, et al. Radical prostatectomy improves and prevents age dependent progression of lower urinary tract symptoms. J Urol 2014;191:412-7. [Crossref] [PubMed]
- Acar C, Schoffelmeer CC, Tillier C, et al. Quality of life in patients with low-risk prostate cancer. A comparative retrospective study: brachytherapy versus robot-assisted laparoscopic prostatectomy versus active surveillance. J Endourol 2014;28:117-24. [Crossref] [PubMed]