Peyronie’s graft surgery—tips and tricks from the masters in andrologic surgery
IntroductionOther Section
Peyronie’s disease (PD) is an acquired benign process which affects the tunica albuginea of the penis leading to fibrous plaques. With an estimated prevalence of 3–9% of adult men, PD is not a rare disease. PD mainly affects males between 40 and 70 years. However, the disease also occurs in the younger population under 40 years old (1-3). PD can lead to the following symptoms: penile plaques, penile curvature, penile deformities like hourglass deformity, shortening of the penis, painful erections, erectile dysfunction (ED), and depression (4-9). The most characteristic and most bothersome symptom in affected patients is penile curvature, that may lead to inability to engage in penetrative sexual intercourse (1,8,10). Surgical therapy is considered the gold standard to correct penile deviation. Indications for surgical therapy include disease duration >12 months, stable phase of PD >6 months, and inability of the patient to perform sexual intercourse due to the extent of penile deformity including curvature and/or hinge effect. Surgical therapy of PD is subdivided into three main procedures: (I) plication techniques; (II) grafting techniques with partial plaque excision or incision followed by defect closure of the tunica albuginea with various grafts; and (III) correction of deformity with simultaneous penile prosthesis implantation in patients with ED not responding to medical therapy (5,11). Grafting techniques to correct penile deformity are applied when curvature exceeds 60°, as these procedures may preserve penile length by elongating the concave side of curvature (12,13). Besides a curvature of >60°, grafting techniques are also indicated when patients experience a shortened penis, to avoid further shortening after plication. Moreover, the presence of an hourglass deformity with associated hinge effect represents another indication for a grafting technique.
The aim of this report is to provide a step-by-step tutorial on grafting techniques for the surgical management of PD. These techniques can be challenging, especially in inexperienced hands. As such, this paper also provides tips and tricks from experienced surgeons in the field, who share their experience and expertise with young colleagues and beginners in penile reconstructive surgery. The tips and tricks provided by this study will also lead to shortening of the learning curve. The senior surgeons of this study (GH, LAL) have learned from multiple repetition of grafting techniques, and from possible complications/problems that occurred with each modification of their technique. As such, the reported experience will help other colleagues to avoid making the same mistakes in the future. This study also provides information and recommendations for proper patient selection and patient counselling before planning a grafting technique, as well as current recommendations on penile rehabilitation following grafting techniques. The ultimate goal will be improvement of patient care and patient safety, which will lead to increased patient satisfaction rates.
MethodsOther Section
This report provides recommendations regarding pre- and postoperative considerations from two experienced surgeons in PD reconstructive surgery (GH, LAL). Special attention is paid to patient counselling and patient selection for grafting techniques in PD. Moreover, this report includes recommendations against performing a grafting technique in patients not meeting the correct indications.
This report describes personal experience from two high-volume surgeons in PD graft surgery (GH, LAL), who share their experience and expertise. One major focus is to provide a detailed step-by-step surgical tutorial for PD grafting techniques, as performed on a daily basis by the authors. This includes recommendations on preferred sutures, grafts, dressings, and catheter placement. Each surgeon will detail his surgical approach as each has his own special technique and graft used [GH—Sealing technique with collagen fleece, LAL—partial plaque excision and grafting (PEG) with pericardium]. Preparation and handling of each individual graft is a major step during grafting surgery in PD. Moreover, this study provides particular remarks about pitfalls during surgery and in the postoperative period, and how to avoid them. Each surgeon will focus on this issue independently as both surgeons (GH, LAL) use a different technique and graft type. We also include surgical figures of the major steps during the Sealing technique with collagen fleece (GH) and partial PEG with pericardium (LAL) to illustrate the anatomical structures and important surgical steps.
ResultsOther Section
Preoperative considerations
The most important concern before planning a grafting technique for men with PD is making sure to have the correct indication. One major requirement is the compromised ability or inability of the patient to participate in penetrative sexual intercourse due to the extent of penile deformity. Other indications for a grafting technique include a curvature of >60°, a shortened penis, or the presence of an hourglass deformity with hinge effect. However, patients scheduled for a grafting technique should have strong preoperative erectile rigidity as these techniques may lead to worsening of erectile function (1). This is best assessed preoperatively by penile duplex Doppler ultrasound study using a vasoactive agent (e.g., Tri-Mix or Prostaglandine). If the resulting erection is measured as a grade 3 or 4 erection on the Erection Hardness Score (EHS), this is regarded sufficient for a grafting technique.
Patients suffering from PD should be counseled that all therapeutic options available today are symptomatic treatments, i.e., they can relieve symptoms associated with the disease. However, due to the lack of pathophysiological knowledge, there is no cure for PD. This aspect should be discussed with the patient prior to surgery, as there is risk of recurrent deformity in 10–33% of cases (1,14). Surgical treatment of PD should only be performed in the stable phase of the disease in order to minimize the risk of recurrence.
Patient selection
Selecting the ideal patient for grafting surgery in PD is a key to success. The patient should meet all of the rigorous inclusion criteria, as described above. Importantly, the patient should have sufficient and documented erectile rigidity preoperatively. Otherwise the patient should be recommended to undergo penile prosthesis implantation in order to restore erectile function and to correct penile deformity simultaneously (if needed by additional maneuvers, e.g., modeling or incision with or without grafting) (15,16). Realistic expectations must be set, as it is crucial that the PD patient understands that there are surgical limitations, such as penile length restoration. Surgery should be refused in patients with unrealistic expectations, e.g., patients who expect their penis to look like it was before the onset of PD (length, shape, rigidity). The same applies for aggressive or very demanding patients. In this regard it is noteworthy to mention that PD is not a life-threatening condition. Thus, it is justified to refuse patients who do not meet all of the inclusion/exclusion criteria.
Patient counseling
Preoperative counseling with a fully documented, signed consent by patients who are willing to undergo surgical therapy for PD is imperative. Patients have to be informed preoperatively in detail about possible complications and negative outcomes associated with the specific surgical approach. Furthermore, patients have to be informed about the estimated surgical outcome and realistic expectations have to be set. It is important that the patient understands that surgery has its limitations and, more important, that it is not possible by means of any surgical intervention, to achieve the original state of the penis (length, shape, rigidity) that is similar to the one before the onset of the disease. The extent of penile curvature (>60°) appears to be the main limiting factors in a man’s ability to perform coitus. Penile deformities, such as an hourglass deformity with hinge effects, seem to interfere on occasion as well (17). One important risk associated with surgical therapy for PD is penile shortening, which may occur with any surgical technique, though the risk of shortening is less with grafting techniques (18). This is an important detail, as almost all patients have already experienced penile shortening associated with their PD (8). In this context, persistent curvature may also be present after surgery. However, when the postoperative curvature is <20°, most patients are “functionally straight” and typically satisfied. The risk of postoperative ED can be as high as 67% (19). This is particularly important, as up to 58% of patients with PD already experience ED concomitantly with their disease (8). Change or decrease of penile sensation (penile hypoesthesia, glans numbness) is a complication that has been reported in 3–31% of cases (11,20,21), and can lead to orgasmic dysfunction in some patients. In most cases, however, sexual sensation will recover with time. In summary, when the patient is informed in detail about the scheduled surgical approach and knows about possible results and complications, this may lead to higher patient satisfaction rates.
Surgical technique
In the following section, each senior surgeon (GH, LAL) will describe his grafting technique in detail, providing a step-by-step tutorial (22,23).
Sealing technique with collagen fleece (GH)
Antibiotic prophylaxis is used only during surgery by means of Ampicillin/Sulbactam (Unasyn®, Pfizer, New York City, NY, USA). A trans-urethral catheter is not necessary during surgery. However, at the end of surgery placing a catheter together with a light compression dressing is important to keep the penis in a stretch position. First, a circumcising skin incision and penile degloving is performed. The skin incision has to be deep enough, from the beginning, to reach Buck’s fascia. Once an avascular layer is reached one has to stop as a deeper incision may injure the underlying nerves within the neurovascular bundle. If the correct layer is unclear, one can also start from the ventral aspect of the penis after skin incision, and go directly down to the urethra. Once the urethra is reached a further circular incision on the lateral and dorsal aspect can be executed. After this step, penile degloving has to be carried out down to the base of the penis in order to provide exposure of the entire penile shaft. Penile degloving is best done by using a ray-tec sponge to slide the full-thickness skin of the penile shaft, beginning distally towards to the proximal part of the penis. Providing that Buck’s fascia has been reached correctly after the skin incision, penile degloving will be very easy. Remember that Buck’s fascia is an avascular layer.
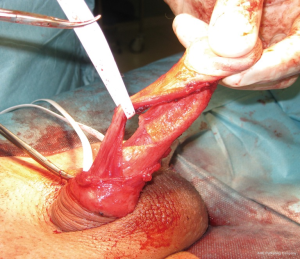
Then, beginning next to the urethra, Buck’s fascia is opened on both sides. This is done by electrocautery in the longitudinal direction parallel to the urethra, paying attention not to damage the underlying tunica albuginea. Once the tunica albuginea is reached careful lateral dissection and mobilization of the neurovascular bundle is performed with a fine scissors, from both sides of the urethra. In order to avoid damage to the nerves within the neurovascular bundle, it is important not to use bipolar or electrocautery during this step. The edge of the neurovascular bundle is grasped with a ray-tec sponge (better than a forceps) to avoid damage to the nerves. Then the bundle is hold on moderate stretch and dissected off the tunica albuginea. During this step it is important to stay right on the tunica to avoid injury to the neurovascular bundle.
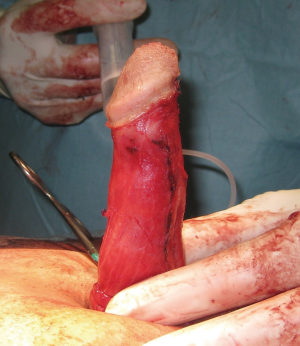
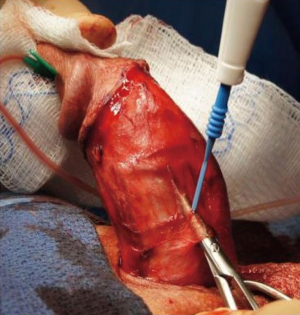
Once the dorsal aspect of the tunica is reached a vessel loop is pulled through to help elevate the neurovascular bundle, which makes further preparation of the bundle easier. The bundle is usually prepared and elevated at a longitudinal distance of approximately 6 cm (Figure 1). To clearly identify the point of maximum curvature, an artificial erection is achieved by injecting saline into the corporal bodies after placement of a tourniquet at the base of the penis (5.0 mm Silicone-loop, Serag Wiessner, Naila, Germany). The penis is then assessed for both curvature, using a goniometer, as well as any buckling, narrowing, hinge effect, or hourglass deformity. Subsequently, a partial plaque excision is performed at the point of maximum curvature on the concave (dorsal) side of curvature. Partial plaque excision is executed by excising an ellipsoid part of the tunica albuginea at the point of maximum curvature, measuring 2.0 cm × 0.5cm (transverse and longitudinal direction, respectively), with the resulting defect then extended laterally (Figure 2) (11,24). The final resulting defect then looks nearly diamond-shaped. During this step, it is crucial not to damage the underlying erectile tissue, as this may result in postoperative ED. The resulting defect of the tunica albuginea is then sealed by the self-adhesive collagen fleece (TachoSil®, Baxter Healthcare Corporation, CA, USA) without any sutures needed (Figure 3). The collagen fleece with an original size of 4.8 cm × 4.8 cm is moistened with physiological saline for 3 s and then put on the defect. It is important that the fleece overlaps the defect at each side of at least 5 mm, the more the better. Importantly, the yellow side of the collagen fleece is put down to the tunica and the defect. Then it is manually molded over the defect and the tunica for 3 minutes until it sticks on the defect and the tunica. As this step is crucial for the Sealing technique, it is important to take some time for it. Importantly, exact adjustment and sewing in the defect, as performed with other grafts, can be omitted. The fleece has a stretching capability; therefore the risk for contraction is minimal. The costs of the collagen fleece are approximately 170.00–190.00 Euros, which represents a cost-effective option. After 3 minutes a watertight closure of the tunical defect is achieved. The penis is held under moderate stretch throughout this step. An artificial erection is then again performed to confirm the watertight closure of the tunica albuginea and the result of correction (Figure 4). However, it is important not to overfill the penis during this artificial erection test, as the collagen fleece has its limitations during this initial phase (80% of maximum erection is sufficient). If residual curvature >20° or lateral deviation is present, additional tunical plication can be performed, which is very rarely needed. Finally, Buck’s fascia is closed on both sides by a running Monocryl® 4-0 suture (Ethicon, Somerville, NJ, USA). This means the edge of the neurovascular bundle is resewn to the periurethral tissue in the longitudinal direction. Then, the tourniquet is removed and the penile skin is attached with interrupted Monocryl® 4-0 sutures. A ring block is performed at the base of the penis using 20 mL of 0.5% pure ropivacaine for postoperative pain control. A light compression dressing is applied and left for 3 days.

Plaque excision and pericardial grafting procedure (PEG) (LAL)
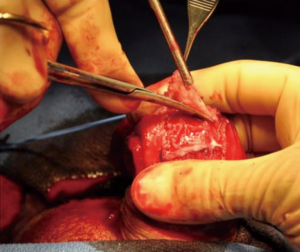
For the plaque excision and PEG, we recommend perioperative antimicrobial prophylaxis with cefazolin as per the AUA best practice policy statement (25). The penis is measured on stretch dorsally from the pubis to the corona with the penis positioned perpendicular to the body. A 21-gauge butterfly needle is placed through the glans into the corpus cavernosum. The needle should not be placed into the corpora through the shaft as infiltration of saline can compromise degloving the penis and dissecting the neurovascular bundle. An artificial erection is created with a vasodilating agent such as Alprostadil 20 mcg and supplemented with injectable saline. Thus, it is not required to place a tourniquet. The penis is then assessed for both curvature, using a goniometer, as well as any buckling, narrowing, hinge effect, or hourglass deformity. A circumcising incision is then made approximately 1.5–2.0 cm proximal to the corona and the penis degloved. Degloving is best achieved when the circumcising incision is carried down to Buck’s fascia and then a sponge is used to gently separate the shaft tissue from Buck’s fascia. Hemostasis is obtained using bipolar electrocautery. We recommend against the use of monopolar electrocautery due to risk of injury to the neurovascular bundle. Once the penis is degloved Buck’s fascia is elevated off the distal 2/3 of the penis unless the patient’s curve involves the proximal third. A pair of longitudinal incisions are made 1 cm lateral to the urethral ridge leaving tissue to reapproximate Buck’s fascia at the end of the procedure (Figure 5). This plane is carried dorso-laterally. In order to prevent tears in the fascia, grasp it using your fingers rather than a forcep. As the Peyronie’s plaque is most often on the dorsal aspect of the penis, separating the bundle from the underlying tunica can be challenging particularly if there has been previous intralesional injection therapy. In this case, a combination of sharp dissection using a Devine-Horton scissors (Snowden-Pencer, Tucker, Georgia) and bipolar cautery can be used to elevate the neurovascular bundle off the tunica albuginea. Keep in mind perforating vessels running from the neurovascular bundle through the tunica albuginea, which most often are located near the urethra. The neurovascular bundle is then secured using a vessel loop. An artificial erection is induced and the area of most severe disease is noted. Historically, the goal was to “cut out the disease”, but we recommend against this as it leads to unnecessarily large grafts with a reported higher risk of ED (26,27). The area of maximum deformity is excised, but not necessarily the entire plaque (Figure 6). This is particularly important in areas of severe indentation. Failure to excise the area of maximum indentation can lead to correction of the curvature but leaves the patient with persistent narrowing or a hinge effect. A rectangular piece of tunica is typically excised. If indentation continues under the urethra, the lateral border of the defect should be just lateral to the urethral ridge. Do not resect tunica under the urethra. If, on the other hand, indentation does not involve the contralateral side, carry the tunical excision through the entire septum to release its tethering effect but not all the way to the urethral ridge. Thus, the excision should always involve the septum, but in the instance of unilateral indentation, it need not be taken further than the septum on the contralateral side. This approach limits the need for extensive, unnecessary, dissection, while also minimizing the size of the produced defect.
The plaque tissue must be elevated with great care to minimize injury to the cavernosal tissue. Once the Peyronie’s plaque is excised the corners of the tunical defect are darted radially using a small scissors. This is done by placing the scissors at a 45° angle to the lateral and transverse edge and making a small cut outward approximately 3–4 mm. This maneuver helps to correct narrowing without creating an needlessly large defect. A 4-0 PDS (Ethicon, Somerville, New Jersey) suture is placed through the darted 4 corners as well as the midpoints transversely both proximally and distally. Place a small clamp on these tags; do not tie this suture. All needles are left on the field. The penis is measured on stretch and the defect is measured on stretch on all four sides (Figure 7). To measure the transverse segments place the segment from one corner to the midline stay suture on tension and measure. Repeat this procedure on the other side of the midline stay suture and add these measurements together. Repeat this process for both the proximal and distal transverse segments. The proximal and distal transverse measurements may differ (the distal measurement is frequently shorter), but the lateral sides should be the same length. If they are not equal, the radial incisions can be extended slightly in order to achieve symmetry (28). The pericardial graft (Tutoplast®, Coloplast, Humlebæk, Denmark) is then prepared on the back table. It should be rehydrated in a bacitracin solution prior to manipulation. The graft is tailored to be 2–3 mm longer than the measured defect. If the proximal and distal transverse aspects are different lengths, the graft is cut into a trapezoid to accommodate this discrepancy. At this point, orientation of the graft can be easily lost. To counter this, the graft should be marked with an arrow directed at what will become the distal border of the graft.
The previously placed stay sutures are then placed through the corresponding points on the graft and tied. Leave a 3–4 cm tail and place a clamp on it. The tails will be used to provide tension along the future suture line and facilitate the running closure. The needles are left in place on the 4 corners. The needles from the transverse midpoint stay sutures are removed. The assistant places gentle tension on the suture by holding two of the clamps in the direction of the suture line. The previously tied 4-0 PDS sutures are then run along each aspect of the graft and tied at the corners (Figure 8). Once the graft is secured, 2 to 3 4-0 PDS midline sutures are placed through the graft incorporating the septal fibers. This helps prevent postoperative hematoma formation deep to the graft. An artificial erection is induced and curvature (as well as indentation) is reassessed. Any areas which are not water tight are reinforced with 4-0 PDS suture. If residual curve exists outside of the grafted area, additional straightening maneuvers can be undertaken; the authors use 3-0 PDS plication sutures placed in a Lembert fashion if necessary. Once adequate straightening in accomplished, the field is washed with antibiotic solution and hemostasis obtained with bipolar cautery. Buck’s fascia is reapproximated using a 4-0 chromic suture. The shaft and subcoronal tissue are then reapproximated in 2 layers. The dartos is first closed with interrupted 4-0 Monocryl, and the skin is reapproximated with 4-0 chromic using an interrupted horizontal mattress technique. A ring block is performed at the base of the penis using 20 mL of 0.5% ropivacaine without epinephrine for postoperative pain control. With the penis on full stretch, a Xeroform gauze (3M, St. Paul, MN) is placed around the circumcising incision and then a Coban (3M, St. Paul, MN) dressing wrapped from distal to proximal to provide light compression. It is imperative that all patients void prior to discharge from the post anesthesia recovery area. A fluffy dressing is placed over the penis and scrotum and maintained in place with mesh panties. Over 90% of our patients are discharged home or to a local hotel on postoperative day 0.
Postoperative considerations and penile rehabilitation program
Postoperative regimen for the Sealing technique
At the end of surgery after placing the penile ring block for postoperative pain control a transurethral catheter and a light compression dressing are applied and left for 3 days. Showering is allowed after removal of the dressing.
Postoperatively, patients should refrain from sexual intercourse and sexual activities for 6 weeks. Postoperative penile rehabilitation is performed in order to reduce the risk of postoperative ED, enhance recovery of erectile function, reduce the risk of penile length loss after surgery, and optimize straightening of the penis (1,5,8,25). We advise patients to massage and stretch the penis for 30 minutes daily, beginning 3 weeks after surgery for a period of 3 months. Nocturnal PDE-5 inhibitors have been recommended in order to improve nocturnal erections, reduce the risk of postoperative ED, stretch the penis, and improve oxygenation to the applied graft (24,26). We advise patients to start this treatment 7 days after surgery for a period of 4 weeks.
Postoperative regimen for the PEG procedure
No catheter is used during or after the PEG procedure. The first postoperative visit is typically 2 weeks after surgery, at which point, the patient is instructed to begin massage and stretch therapy (29-31). The patient grasps the penis by the glans and gently pulls it away from the body. The other hand massages the shaft. We recommend 5 minute sessions twice daily for 2–4 weeks. If the patient tolerates stretch therapy well, we recommend incorporating his partner into the rehabilitation process, particularly after the first 2 weeks. This is an ideal method to reintroduce touching the penis to both the patient and his partner and also alleviates some fears about future injury to the penis in a safe setting.
External penile traction therapy is initiated 3–4 weeks postoperatively averaging greater than or equal to 3 hours daily for 3 months. The use of external penile traction devices has been encouraged to reduce postoperative penile shortening and to guide straight healing of the penis (1). We also recommend beginning a low dose PDE-5 inhibitor such as tadalafil 5 mg on postoperative evening 7, for 30 nights.
Combination approach of the Sealing technique with collagen fleece plus penile prosthesis implantation (GH)
Penile prosthesis implantation plus additional maneuvers to correct persistent penile deviation, such as the modeling maneuver, represents the surgical approach of choice for patients suffering from PD who do also experience severe ED not responding to medical treatment (15,16). However, the modeling maneuver is associated with risk of urethral injury, consequently leading to removal of the implant and abortion of the procedure (15,16). Plication techniques to correct persistent deviation during penile prosthesis implantation are associated with risk of injury of the implant and thus not preferred. Grafting techniques during penile prosthesis implantation lead to increased operative times and are also associated with risk of injury of the implant as the graft of choice has to be sewn into the tunical defect following plaque incision or partial plaque excision with the device in place.
A novel, safe and very promising approach to correct persistent penile deviation during penile prosthesis implantation in those patients is the combination of the Sealing technique and penile prosthesis implantation. This technique also represents a time-saving approach. The major steps of this novel approach will be highlighted in the following (peno-scrotal approach with 3-piece inflatable penile prosthesis):
After the 3-piece inflatable penile prosthesis is put into the cavernous bodies and the corporotomies are closed the device is inflated to the maximum. When the persistent deviation is >30°–40° then the combined approach can be performed as the chance of spontaneous improvement or resolution is minimum. The pump is placed into the scrotum and the skin is closed to reduce the risk of infection. Then the device is deflated and the Sealing technique starts with a circumcising incision, as described above. The procedure continues with penile degloving, opening of Buck’s fascia and elevation of the neurovascular bundle as the regular Sealing technique. Keep in mind that the implant is inside the cavernous bodies. However, if you pay attention to the surgical details as described above there should not be any problem or risk of damaging the implant. Once the neurovascular bundle is elevated the implant is inflated to the maximum to check the deviation. With the device fully inflated, a plaque incision is performed at the point of maximum curvature on the dorsal aspect of the penis in a transverse fashion using electrocautery. Pay attention not to use a regular scalpel/knife as this could damage the implant. Once the tunica is cut through and the tension removed you will notice an acoustic “popping”, which is the implant expanding to the maximum girth at this site. You should be able to check the result of correction immediately. In most cases with predominant dorsal deviation the penis will be absolutely straight. You can try to inflate the device more if possible, for assurance. Then the tunical defect over the implant is sealed with the collagen fleece. As with the original Sealing technique it is important that the collagen fleece overlaps the edges of the tunical defect at each side of at least 5mm. The collagen fleece is molded over the tunica and the implant, which is still inflated. As the collagen fleece does not need to be sewn into the tunical defect, there is absolutely no risk of injuring the device, which represents the major advantage of this combined approach. In the next step the neurovascular bundle is put back, Buck’s fascia is closed, and the penile skin is closed. At the end of surgery the implant is left inflated for 3 days and a loosely dressing is put around the penis and also left for 3 days. As with regular penile prosthesis surgery, a trans-urethral catheter is mandatory throughout the whole procedure. The post-operative regimen is identical with regular placement of a 3-piece inflatable penile prosthesis. Sexual intercourse should not start before 6 weeks postoperatively.
DiscussionOther Section
Grafting techniques for the surgical treatment of PD are challenging, especially in inexperienced hands. There are a lot of pitfalls before, during, and after surgery that one has to know and consider before planning such procedures in affected patients. This paper helps the reader to understand important key steps during grafting surgery, in order to avoid mistakes and failures. Moreover, the present paper summarizes important pre-, intra-, and postoperative recommendations, and lessons which the senior authors have learned from multiple repetition of their special technique.
The most important points associated with each technique (Sealing technique, PEG procedure) will be highlighted in the following section.
Sealing technique
One important step after mobilization of the neurovascular bundle is partial plaque excision (during artificial erection). This is done by excising an ellipsoid part of the tunica albuginea at the point of maximum curvature (concave side of curvature). As the direction of curvature is dorsal in most patients, this excision is performed at the dorsal aspect of the penis. It is crucial not to damage the underlying erectile tissue, as this would cause postoperative ED by impairing the veno-occlusive mechanism. This can be avoided by staying on the tunica albuginea during excision, without cutting into the deeper cavernosal tissue.
Another important step is sealing of the tunical defect with the collagen fleece. First, the collagen fleece is moistened with physiological saline by dipping the whole fleece in a bowl with saline. Then the fleece is put on the defect and the resection edges of the tunica. It is of utmost importance that the fleece overlaps the defect at each side of at least 5 mm so that it can stick on the tunica providing a watertight closure. The fleece has to be molded over the defect and the tunica with the fingers for approximately 3 minutes. The penis has to be held on moderate stretch during this step, without pulling too much.
After the tunical defect is sealed and Buck’s fascia closed an artificial erection test is performed to check the result of correction. However, it is important to know that the collagen fleece has its limitation during this very early stage. Thus, it is recommended to induce an artificial erection of about 80% of maximum erection. This is sufficient to check the result of correction.
Placement of a transurethral catheter and a loosely dressing around the penis after surgery is crucial. This is left for 3 days postoperatively.
PEG procedure
The critical aspects of the PEG procedure are similar to the aspects described above for the Sealing technique. In particular, care should be taken to stay in the plane of the tunica albuginea when elevating the Peyronie’s plaque to minimize injury to the cavernosal tissue. Critical aspects unique to the PEG procedure are described below. If the following steps are taken the rates of residual deformity, ED, and postoperative hematoma can all be reduced.
When removing the Peyronie’s plaque the focus should be the area of maximal deformity, but the plaque does not need to be completely excised. Even if the curve is lateral, the excised plaque must include the septum because this is where the scarring is anchored. Failure to remove the septal portion of the plaque will likely lead to residual curvature (32).
Once the Peyronie’s plaque is removed, special care should be taken to restore the normal caliber of the penis at the level of maximum indentation. This is done by darting the 4 corners of the defect radially in order to allow for circumferential expansion (28).
After the graft is secured with a running closure, it should be further tacked down to prevent hematoma formation. The 4-0 PDS is placed through the midline to incorporate the septal fibers. This will reduce the space under the graft. The pericardial grafting technique allows one to check for residual curvature by infusion of saline through the scalp needle in the glans. This is critical as we find up to 50% of patients who undergo the PEG procedure also require plication to optimize straightening.
Regardless of the approach taken, the patient should refrain from sexual activities for 6 weeks and follow the recommended rehabilitation program in order to achieve the best possible result. By following the above-mentioned surgical steps and by taking care of all recommendations listed above, the surgical result will be at its best.
Besides the step-by-step surgical approach, it is very important to follow preoperative recommendations and considerations in order to identify the most suitable patient for a grafting technique. The preoperative counseling helps to have well-informed patients and to eliminate unrealistic expectations. At the end, the ultimate goal should be improved patient care, safety and satisfaction.
Complications
Sealing technique
One important aspect in order to avoid postoperative ED is proper patient selection. As with grafting techniques, the Sealing technique requires good preoperative erectile function. It is recommended to perform an artificial erection test in an outpatient setting to check the degree of deviation/deformity, but also to check the erectile status of the patient, when necessary by additional penile duplex Doppler ultrasound. If the patient displays a grade 3 or 4 erection, measured by the EHS, then the Sealing technique can be performed. Should the patient display a grade 1 or 2 erection or even no erection at all, then this patient should be advised to undergo penile prosthesis implantation, e.g., the combination approach (see above). This is one major issue to avoid complications and unsatisfied patients.
Another aspect to avoid postoperative ED is the extent of plaque excision. Today, total plaque excision is not recommended due to its unacceptable high rates of ED. The authors recommend performing a partial plaque excision at the point of maximum curvature, as described above. This will lead to smaller tunical defects (compared to total plaque excision) and thus obvious less ED rates postoperatively.
Pay attention not to overfill the penis with saline during the artificial erection test after partial plaque excision and sealing with the collagen fleece. As the collagen fleece has its limitations during this very initial phase it may happen that it will come off the tunica leading to leakage. If that happens stop injecting saline and re-stick the fleece over the tunical defect. Inducing a 80% of maximum erection is sufficient to check the result of correction. Moreover, it is important to know that a 80% artificial erection test during surgery is comparable to a 100% natural erection induced spontaneously by the patient. Thus, it is not necessary to aim for more during surgery.
If the dressing around the penis after surgery is not put properly, the risk of sliding off the penis is high. This may lead to hematoma formation under the penile skin which may require surgical drainage or revision. Thus, it is recommended to fix the dressing on the skin at the base of the penis by means of a pavement. In this regard it should be mentioned that putting a catheter at the end of surgery is mandatory. This is because the dressing around the penis is put with a light compression to avoid hematoma formation. This in turn may lead to urinary retention. The best way to avoid this and further unnecessary maneuvers is to place a catheter and leave it for 3 days.
PEG procedure
While there is a reported risk of complete glans hypoesthesia and/or necrosis, the authors have not experienced this particular complication using the described technique.
ED is likely a product of multiple aspects of the surgery. Primarily, ED can result from manipulation of the neurovascular bundle as it is being dissected off the underlying tunica albuginea. This can often be a challenging portion of the procedure as inflammatory changes associated with the plaque can obscure this surgical plane. The authors recommend against the use of monopolar cautery at this stage due to its potential damaging effects on the neurovascular bundle. Instead, a combination sharp dissection and bipolar cautery should be used to carefully secure the neurovascular bundle. It is then further protected using a vessel loop.
It appears that the size of the graft plays a minor role in terms of postoperative ED. The defect created in order to achieve straightness is often 4 cm × 6 cm and does not normally produce ED. That being said, there are merits to minimizing graft size where possible. The most useful techniques to achieve this goal are the previously described method of darting the corners of the graft radially and proper identification of the plane between the Peyronie’s plaque and the cavernosal tissue below it. Darting the corners radially allows for expansion of the corporal tissue without resecting additional tunica albuginea. This reduces damage to the underlying cavernosal tissue, preserving erectile function. Similarly, identification of the PD plaque and minimizing manipulation of the cavernosal tissue during the plaque excision increases the likelihood of a favorable outcome.
More important than any surgical technique is a proper evaluation of preoperative erectile function. As the PEG procedure carries an increased risk of ED compared to other straightening procedures, the authors strongly recommend against the use of the PEG procedure in men who do not have strong erections at home with or without the aid of PDE5 inhibitors. It has been suggested that geometric changes associated with PD can contribute to ED preoperatively. Under these circumstances, it is possible that a straightening procedure could improve erectile function, but the surgeon must exercise caution when counseling these patients. These cases are rare and require extensive counseling. The patient should understand that improvement of erectile quality after the PEG procedure should not be expected.
Residual deformity is a potential complication after the PEG procedure which includes both residual curve and either residual or new narrowing. These complications can be avoided via multiple intraoperative steps. As previously discussed, the entire PD plaque need not be excised but rather should focus on the area of maximal curvature and/or indentation. The plaque, however, is anchored in the septal fibers and even if the curve is lateralized to one side, the tunica albuginea should be excised across the midline to include those septal fibers.
Narrowing, on the other hand, is due to inhibition of circumferential expansion of the erect penis. This can be the result of residual PD plaque or the graft being restrictive. The technique of darting the defect radially aids in allowing the corpora to expand circumferentially without substantially increasing the size of the tunical defect. This maneuver also allows the surgeon to produce a defect which is of equal lengths on the lateral sides, ultimately resulting in a symmetric graft along its lateral borders.
Finally, the sub-graft hematoma represents a problem which can be minimized or, when present, treated with relative ease. After the graft is sutured into position, a small (2 mm) hole is made in the graft over the septum to evacuate blood that had accumulated under the graft. Through this hole, 4-0 PDS (Ethicon, Somerville, New Jersey) anchoring sutures are placed through the septal fibers to tack the graft down onto the corpora. This minimizes the dead space and decreases the risk of hematoma formation. In the event that a hematoma does form, it can be aspirated directly through the skin in the office. Small hematomas will reabsorb in time but may be bothersome and unsightly in which case, office aspiration is performed.
ConclusionsOther Section
Grafting techniques for the surgical management of PD represent the preferred option in patients with stable disease, penile curvature >60°, short penis, or hourglass deformity with hinge effect. However, patients who are scheduled for grafting surgery must have full to near full and documented preoperative erectile rigidity. Adequate preoperative counseling of patients is crucial, and should include possible adverse effects and negative outcomes. There are many details during grafting techniques, which have to be considered in order to achieve the best result possible. The present paper offers a step-by-step tutorial for grafting techniques in PD, especially for the Sealing technique and the PEG procedure, in order to help the reader understand the major steps during surgery and to avoid pitfalls. Careful patient selection, a reliable and established surgical technique and a postoperative rehabilitation program are main predictors for treatment success.
AcknowledgementsOther Section
None.
FootnoteOther Section
Conflicts of Interest: The authors have no conflicts of interest to declare.
ReferencesOther Section
- Levine LA, Burnett AL. Standard operating procedures for Peyronie’s disease. J Sex Med 2013;10:230-44. [Crossref] [PubMed]
- Mulhall JP, Creech SD, Boorjian SA, et al. Subjective and objective analysis of the prevalence of Peyronie's disease in a population of men presenting for prostate cancer screening. J Urol 2004;171:2350-3. [Crossref] [PubMed]
- Tal R, Hall MS, Alex B, et al. Peyronie's disease in teenagers. J Sex Med 2012;9:302-8. [Crossref] [PubMed]
- Hatzichristodoulou G, Lahme S. Peyronie's Disease, In: Merseburger AS, Kuczyk MM, Moul JW. editors. Urology at a Glance. Berlin-Heidelberg: Springer Publishing, 2014:225-36.
- Kadioglu A, Kücükdurmaz F, Sanli O. Current status of the surgical management of Peyronie's disease. Nat Rev Urol 2011;8:95-106. [Crossref] [PubMed]
- Larsen SM, Levine LA. Review of non-surgical treatment options for Peyronie's disease. Int J Impot Res 2012;24:1-10. [Crossref] [PubMed]
- Nelson CJ, Mulhall JP. Psychological impact of Peyronie's disease:a review. J Sex Med 2013;10:653-60. [Crossref] [PubMed]
- Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie's disease:evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. [Crossref] [PubMed]
- Smith JF, Walsh TJ, Lue TF. Peyronie's disease:a critical appraisal of current diagnosis and treatment. Int J Impot Res 2008;20:445-59. [Crossref] [PubMed]
- Mulhall JP, Schiff J, Guhring P. An Analysis of the Natural History of Peyronie's Disease. J Urol 2006;175:2115-8. [Crossref] [PubMed]
- Hatzichristodoulou G, Gschwend JE, Lahme S. Surgical therapy of Peyronie's disease by partial plaque excision and grafting with collagen fleece: feasibility study of a new technique. Int J Impot Res 2013;25:183-7. [Crossref] [PubMed]
- Chung E, Ralph D, Kagioglu A, et al. Evidence-based management guidelines on Peyronie’s disease. J Sex Med 2016;13:905-23. [Crossref] [PubMed]
- Hatzichristodoulou G. Grafting techniques for Peyronie's disease. Transl Androl Urol 2016;5:334-41. [Crossref] [PubMed]
- Staerman F, Pierrevelcin J, Ripert T, et al. Medium-term follow-up of plaque incision and porcine small intestinal submucosal grafting for Peyronie's disease. Int J Impot Res 2010;22:343-8. [Crossref] [PubMed]
- Wilson SK, Delk JR 2nd. A new treatment for Peyronie's disease:modeling the penis over an inflatable penile prosthesis. J Urol 1994;152:1121-3. [Crossref] [PubMed]
- Wilson SK, Cleves MA, Delk JR 2nd. Long-term follow-up of treatment for Peyronie's disease:modeling the penis over an inflatable penile prosthesis. J Urol 2001;165:825-9. [Crossref] [PubMed]
- Walsh TJ, Hotaling JM, Lue TF, et al. How curved is too curved? The severity of penile deformity may predict sexual disability among men with Peyronie's disease. Int J Impot Res 2013;25:109-12. [Crossref] [PubMed]
- Kueronya V, Miernik A, Stupar S, et al. International multicentre psychometric evaluation of patient-reported outcome data for the treatment of Peyronie's disease. BJU Int 2015;115:822-8. [Crossref] [PubMed]
- Chung E, Clendinning E, Lessard L, et al. Five-year follow-up of Peyronie's graft surgery:outcomes and patient satisfaction. J Sex Med 2011;8:594-600. [Crossref] [PubMed]
- Sansalone S, Garaffa G, Djinovic R, et al. Long-term results of the surgical treatment of Peyronie's disease with Egydio's technique:a European multicentre study. Asian J Androl 2011;13:842-5. [Crossref] [PubMed]
- Taylor FL, Levine LA. Surgical correction of Peyronie's disease via tunica albuginea plication or partial plaque excision with pericardial graft:long-term follow up. J Sex Med 2008;5:2221-8. [Crossref] [PubMed]
- Hatzichristodoulou G. Surgical therapy of Peyronie’s disease by partial plaque excision and Sealing of tunical defect with collagen fleece:The Sealing technique. VJPU 2016;2:076.
- Levine LA. PEG procedure (partial plaque excision and grafting). VJPU 2015;2:053.
- Hatzichristodoulou G. Partial Plaque Excision and Grafting With Collagen Fleece in Peyronie Disease. J Sex Med 2016;13:277-81. [Crossref] [PubMed]
- Wolf JS, Benett CJ, Dmochowski RR, et al. Best Practice Policy Statement on Urologic Surgery Antimicrobial Prophylaxis. Available online: http://www.auanet.org/guidelines/antimicrobial-prophylaxis-(2008-reviewed-and-validity-confirmed-2011-amended-2012)
- Kendirci M, Hellstrom WJ. Critical analysis of surgery for Peyronie's disease. Curr Opin Urol 2004;14:381-8. [Crossref] [PubMed]
- Kadioglu A, Akman T, Sanli O, et al. Surgical treatment of Peyronie's disease:a critical analysis. Eur Urol 2006;50:235-48. [Crossref] [PubMed]
- Levine LA. Partial plaque excision and grafting (PEG) for Peyronie's disease. J Sex Med 2011;8:1842-5. [Crossref] [PubMed]
- Levine LA, Larsen SM. Surgery for Peyronie's disease. Asian J Androl 2013;15:27-34. [Crossref] [PubMed]
- Levine LA, Greenfield JM, Estrada CR. Erectile dysfunction following surgical correction of Peyronie's disease and a pilot study of the use of Sildenafil citrate rehabilitation for postoperative erectile dysfunction. J Sex Med 2005;2:241-7. [Crossref] [PubMed]
- Horton CE, Sadove RC, Devine CJ. Peyronie's disease. Ann Plast Surg 1987;18:122-7. [Crossref] [PubMed]
- Jordan GH. Peyronie's disease. In: Wein AJ, Kavoussi LR, Novick AC. editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders Elsevier, 2007:818-38.