Amniotic therapeutic biomaterials in urology: current and future applications
Historical medical uses of amniotic membrane
The medical uses of the human placenta probably date back centuries, with the first description of its use in a treatise in 1593 by a Chinese clinician Li Shi-Zhen (1). The first mention of the medical use of amniotic membrane in the Western literature appeared in 1910 by Davis, who reported on a series of cases where it was used as a skin graft in a large case series at Johns Hopkins Hospital (2). This was shortly followed by Drs. Stern and Sabella, collaborators who separately published studies using this material in wounds and burns (3,4). Through the rest of the 20th century the medical use of the placenta, and more specifically the amniotic membrane, was described in a number of medical indications including; but not limited to, the following types of cases: (I) skin grafting; (II) lower extremity diabetic ulcers (5); (III) lower extremity venous leg ulcers (6); (IV) general wounds (7); (V) conjunctival surgery and repair (8); (VI) burns (9,10); (VII) periodontal disease and dentistry (11,12); (VIII) vaginal reconstruction and OB/GYN applications (13); (IX) neurosurgical applications including spine surgery (14,15); (X) orthopedic surgery applications (16).
Properties and function of amniotic tissues
While amniotic membrane was originally used because of its recognized ability to substitute as a skin like tissue with healing properties, the underlying physiologic, biochemical and cytological properties of the tissue are reported to confer a number of additional properties, in addition to simply performing as a skin substitute. These properties include: (I) contains essential growth factors (17); (II) modulation of inflammation (18); (III) reduction of scar tissue formation (18); (IV) barrier properties (14); (V) immunologically privileged tissue (19); (VI) enhancement of wound healing (20); (VII) reduction of pain in burns and wounds; (VIII) innate antibiotic properties (21). There are varying degrees of documentation of each of the above properties, but these attributes appear regularly in the literature.
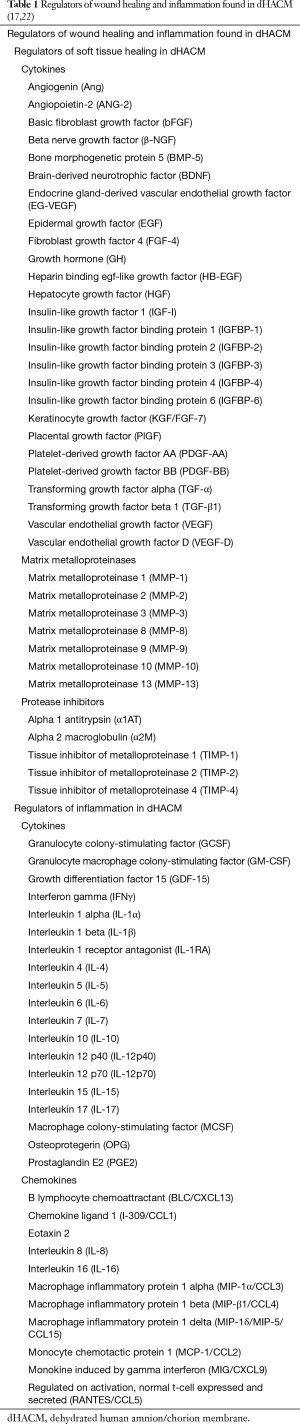
The underlying bimolecular mechanisms responsible for the above properties are becoming increasingly well characterized, in a growing, robust literature (1,17,22-24) (Table 1). Briefly, active participation of mesenchymal and circulating stem cells, activated by a wide array of growth factors and cytokines, and the provision of a collagen based architecture present a unique structure that promotes healing and regeneration of tissues in which the amniotic membrane and its components are applied (22).
Preclinical urologic applications of amniotic tissue products
The general history of the use of amniotic membrane products and the more recent understanding of the underlying mechanism of action behind their properties suggested a number of urologic applications. Preclinical work has explored a number of urogenital applications.
The use of amniotic membrane as a potential material for bladder repair extends back to the early 1980s (25). More recently, Iigma and others demonstrated that transplantation of preserved human amniotic membrane could successfully be used for bladder augmentation in rats, with resulting regeneration of a number of tissues in the bladder being demonstrated as early as 3 months postoperatively (26).
Salehipour et al. have evaluated the use of human amniotic membrane in the reconstruction of long ureteral defects in dogs (27). In this study, the use of human amniotic membrane for the reconstruction of ureteral defects in a canine model was studied. The authors used chorion prepared and properly treated for surgical insertion into dogs with circumferentially cut defects, and while they did not believe the approach to be useful for long (3 cm) defects, they speculated that use of the amniotic membrane might be studied for shorter defects or as a patch graft.
Shakeri et al. looked at the use of amniotic membrane as a xenograft for urethroplasty in rabbits. The authors concluded that amniotic membrane technology was an inexpensive, easy, and biodegradable graft yielding very little antigen effect and a viable option in surgical urethroplasty approaches (28).
Wang et al. looked at a variation of this idea, namely using the collagen scaffolding of amniotic membrane as a potential regenerative material in urethroplasty, and obtained preliminary success in that approach (29). The author’s concluded that tissue-engineered denuded human amniotic scaffold (dHAS) created by separating the basement membrane layer of amniotic membrane minimizes potential rejection and maximizes the biocompatibility of amniotic membrane, making it a potential ideal xenograft for urethral reconstruction. This concept was also explored by Gunes and others, who compared the use of buccal mucosa and amniotic membrane for urethroplasty in a rabbit model (30). The group examined whether buccal mucosa, amniotic membrane, or both might be useful in urethroplasty using epithelial transformation as the experimental endpoint, noting highest efficacy in the combined tissue application. After 8 weeks, the best epithelial transformations were observed in the combined group.
In another study, Shakeri also noted that amniotic membrane maybe a substitute for transitional epithelium of the bladder in dogs. The authors concluded that grafts remained in place in all cases, except in one of the dogs in the augmentation group that developed patch perforation, urine leakage and finally peritonitis. In others, histological examinations revealed evidence of regeneration of normal-appearing urothelium, lamina propria, neovascularization, retracting placental patch, and reconstitution of a normal-appearing and functioning bladder. This suggests that placental membranes, because of their low antigenic properties, easy availability and tolerability by the host urinary tract, could provide an excellent graft material for urinary tract reconstructions (31).
Comparison of amniotic membrane with other materials in preclinical work was conducted by Sharifiaghdas et al. (32). They examined the use of poly lactic-co-glycolic acid (PLGA), PLGA/collagen and human amniotic membrane (hAM) for human urothelial and smooth muscle cell engineering. The authors demonstrated significant improvement of cell attachment and growth achieved by collagen coating (PLGA/collagen) compared to PLGA and hAM. hAM was a weaker matrix for bladder engineering purposes.
Human amniotic fluid and isolates prepared from human amniotic membrane derived mesenchymal stem cells have also had some preliminary scientific work performed on their inherent biological properties. Human amniotic membrane mesenchymal stem cells were interestingly noted to have a suppressive effect on prostate cancer cells (33). Sedrakyan et al. found that amniotic fluid stem cells seemed to reduce the formation of renal fibrosis in a mouse model of acute tubular necrosis (34).
Amniotic membrane has also been used as a supportive scaffold for other procedures. For example, Burgers et al. used nerve grafts, nerve growth factor and a supportive scaffold made from amniotic membrane to repair surgically induced erectile dysfunction in rats. In this study, the use of fetal amniotic membrane as an alternative growth factor matrix was used to improve the regeneration of ablated cavernous nerves in rats as a model to study surgically damaged nerves. The use of membrane as an alternative nerve growth matrix improved electrically stimulated erections and mating behavior in these mice (35).
The underlying logic in many of these preclinical studies focuses on both the structural and regenerative properties of amniotic membrane. In the first case, the underlying structure of the membrane, created by various collagen types, forms an architecture or scaffold that assists in the re-creation of normal tissue. In the second case, the biologically active growth factors, cytokines and other biomolecules initiate and modulate the regenerative process that involves the recruitment and activation of stem cells and fibroblasts in the area under consideration.
Clinical urological applications of amniotic tissues in humans
The broadly recognized ability of amniotic tissues to help in healing and regenerative repair of tissues suggested a number of other direct clinical applications. Preclinical work and initial evaluation of these tissues have been attempted in a number of urogenital indications. Koziak et al. built on the previous preclinical work described above and investigated the use of amniotic membrane in the reconstruction of long ureteral strictures in 11 patients (36,37). Several reports of the use of amniotic membrane to repair vesicovaginal fistulas have also been reported. In each case, successful use of the material has permitted a less aggressive operative or non-operative approach to this problem (38).
Most recently, the use of an amniotic membrane protective layer in the surgical field of patients undergoing robotic assisted laparoscopic prostatectomy as a means of protecting adjacent nerve bundles from scarring has been advanced by a number of clinicians (39,40). The notion that amniotic membrane might be useful in preventing adhesions at the surgical site in DaVinci robot prostatectomies was initially developed and evolved across a number of sites. Patel et al. published a retrospective series of these patients demonstrating improvement in both urinary incontinence and erectile function in the short-term post-operative period (41). For completeness, it is worth noting that amniotic membrane has found numerous applications in OB/GYN surgery as well, with applications in the repair of various abnormalities of the vagina, uterus and related structures in patients (42-49).
At our institutions, we have applied amniotic membrane technology in the following four realms of adult and pediatric urology: (I) proximal and redo-hypospadias repairs; (II) complex penile reconstruction in Peyronie’s disease; (III) microsurgical cord denervation procedures; (IV) posterior urethroplasty in the male with a history of pelvic radiation.
In the field of hypospadias surgery, proximal hypospadias comprises most of the severe cases and results in higher surgical complication rates (50). Between 6–20% of hypospadias patients are diagnosed with proximal hypospadias (51,52). Hypospadias is corrected surgically with the goal of improving cosmetic appearance as well as normalizing erectile function and voiding. Surgery creates a straight phallus, with the meatus residing at the tip of the glans, with a proper and symmetrical appearance of both the glans and penile shaft. For more severe hypospadias, specifically for proximal hypospadias, a variety of surgical techniques can be employed. Unfortunately, even the most skilled surgeons cannot guarantee a positive outcome. Complications from proximal hypospadias repair range from 6–30% depending on the severity of the defect, the surgical technique utilized, and the experience of the surgeon (53). Surgical results are also poorer in re-operative cases. Common complications include urethrocutaneous fistulas (UCF), urethral stricture, urethral diverticulum, and persistent ventral curvature (54). UCF, or a reopening of the surgical site, can occur in 13–33% of patients, depending on the different surgical techniques utilized (50-52,55-58). Current data suggests that an experienced pediatric urologist successfully can close fistulas in 71%, 72%, 77%, 100%, and 100% of patients after fistula repairs 1 to 5, respectively (59). With these high reoperation rates, there is a significant need to investigate innovative approaches to reduce complication rates. One such approach is the potential application of dehydrated human amnion/chorion membrane (dHACM). The underlying premise is to provide a barrier layer with a robust source of tissue and vascular growth factors and provide a local anti-inflammatory environment, thus optimizing soft tissue healing of the surgical site (20,41,60-62).
In the field of Peyronie’s disease, surgical correction of curvature with either permanent plication sutures or graft material usually requires full or partial mobilization of the deep dorsal neurovascular bundle to allow for proper placement of surgical material as well as to avoid potentially devastating complications such as glans numbness and ischemia. Typically, the neurovascular bundle is placed back in its anatomical position and in most cases, it will overly the site of surgical curvature correction. The inflammatory response associated with healing and the subsequent formation of fibrotic tissue and neuroma has been theorized as the cause for post-operative pain with the associated graft material or suture knots. The use of dHACM has been postulated to be used as an interposition graft in between the plication knots or graft material and the neurovascular bundle in an effort to reduce fibrosis and neuroma formation and therefore improve pain outcomes. Anecdotally, we have noticed diminished postoperative pain and more rapid recovery, and are currently studying, in a more formal manner, the utility of using this interposition graft in these cases.
In the field of chronic orchialgia, management strategies are aimed at identifying specific etiologies of the pain and managing those directly (i.e., varicocelectomy, vasectomy reversal, epididymectomy). When a specific etiology cannot be identified, the individual has failed conservative management, or has failed surgical management and spermatic cord denervation may be discussed. Methods that have been employed to improve outcomes of spermatic cord denervation include the use of a provocative pre-operative spermatic cord block and the intraoperative use of the operating room microscope. Even with these improvements in pre-operative screening and surgical techniques the success rate of the procedure is still not 100% (current studies success rates range from 70–90%) and there is a reported orchiectomy rate of 10–20% after the surgery due to persistent pain (63,64). The utilization of dHACM as a wrap at the site of denervation has been theorized to reduce the formation of fibrosis and neuroma and therefore reduce persistent pain post-operatively (63).
In the field of posterior urethral contracture in the male with a history of pelvic radiation, surgical management is aimed at resecting the affected scarred or infected tissue, achieving a watertight tension free anastomosis, and providing a healthy bed of tissue to allow for good wound healing. However, even with these surgical tenants, necrosis and reformation of scar tissue still may occur even in the most skilled hands. The use of dHACM as a wrap at the site of urethral anastomosis has been theorized to recruit healthy tissue ingrowth and improve surgical outcomes. Clinical outcomes are currently being evaluated.
Potential future applications of human amniotic tissues
The broad number of properties found in amniotic membrane, coupled with its immunologically privileged status presents a number of future applications, particularly given the historical preclinical and clinical uses described above. New applications continue to be proposed, and the potential for combining amniotic membrane allografts with other biomaterials expands this horizon further.
Acknowledgements
The authors are indebted to Dr. Donald E. Fetterolf for providing critical suggestions to this review surrounding amnion/chorion technology.
Footnote
Conflicts of Interest: William O. Brant: proctor, consultant, and grant recipient, Boston Scientific; Siam Oottamasathien: scientific advisory consultant, GlycoMira Therapeutics Inc. The other authors have no conflicts of interest to declare.
References
- Silini AR, Cargnoni A, Magatti M. The Long Path of Human Placenta, and Its Derivatives, in Regenerative Medicine. Front Bioeng Biotechnol 2015;3:162. [Crossref] [PubMed]
- Davis JW. Skin transplantation with a review of 550 cases at the Johns Hopkins Hospital. Johns Hopkins Medical Journal 1910;15:307-96.
- Stern M. The grafting of preserved amniotic membrane to burned and ulcerated surfaces, substituting skin grafts. JAMA 1913;60:973-4. [Crossref]
- Sabella N. Use of fetal membranes in skin grafting. Med Records NY 1913;83:478-80.
- Zelen CM, Serena TE, Snyder RJ. A prospective, randomised comparative study of weekly versus biweekly application of dehydrated human amnion/chorion membrane allograft in the management of diabetic foot ulcers. Int Wound J 2014;11:122-8. [Crossref] [PubMed]
- Serena TE, Carter MJ, Le LT. A multicenter, randomized, controlled clinical trial evaluating the use of dehydrated human amnion/chorion membrane allografts and multilayer compression therapy vs. multilayer compression therapy alone in the treatment of venous leg ulcers. Wound Repair Regen 2014;22:688-93. [Crossref] [PubMed]
- Forbes J, Fetterolf DE. Dehydrated amniotic membrane allografts for the treatment of chronic wounds: a case series. J Wound Care 2012;21:290-292,294-6. [Crossref] [PubMed]
- Asoklis RS, Damijonaityte A, Butkiene L. Ocular surface reconstruction using amniotic membrane following excision of conjunctival and limbal tumors. Eur J Ophthalmol 2011;21:552-8. [Crossref] [PubMed]
- Adly OA, Moghazy AM, Abbas AH. Assessment of amniotic and polyurethane membrane dressings in the treatment of burns. Burns 2010;36:703-10. [Crossref] [PubMed]
- Kesting MR, Wolff KD, Hohlweg-Majert B. The role of allogenic amniotic membrane in burn treatment. J Burn Care Res 2008;29:907-16. [Crossref] [PubMed]
- Chen E, Tofe A. A literature review of the safety and biocompatibility of amnion tissue. J Imp Adv Clin Dent 2010;2:67-75.
- Holtzclaw D, Toscano N. Amnion chorion allograft barrier: indications and techniques update. J Imp Adv Clin Dent 2012;4:25-38.
- Sarwar I, Sultana R, Nisa RU. Vaginoplasty by using amnion graft in patients of vaginal agenesis associated with Mayor-Rokitansky-Kuster-Hauser syndrome. J Ayub Med Coll Abbottabad 2010;22:7-10. [PubMed]
- Tao H, Fan H. Implantation of amniotic membrane to reduce postlaminectomy epidural adhesions. Eur Spine J 2009;18:1202-12. [Crossref] [PubMed]
- Subach BR, Copay AG. The use of a dehydrated amnion/chorion membrane allograft in patients who subsequently undergo reexploration after posterior lumbar instrumentation. Adv Orthop 2015;2015:501202. [Crossref] [PubMed]
- Demirkan F, Colakoglu N, Herek O. The use of amniotic membrane in flexor tendon repair: an experimental model. Arch Orthop Trauma Surg 2002;122:396-9. [Crossref] [PubMed]
- Koob TJ, Rennert R, Zabek N. Biological properties of dehydrated human amnion/chorion composite graft: implications for chronic wound healing. Int Wound J 2013;10:493-500. [Crossref] [PubMed]
- Tseng SC, Li DQ, Ma X. Suppression of transforming growth factor-beta isoforms, TGF-beta receptor type II, and myofibroblast differentiation in cultured human corneal and limbal fibroblasts by amniotic membrane matrix. J Cell Physiol 1999;179:325-35. [Crossref] [PubMed]
- Hao Y, Ma DH, Hwang DG. Identification of antiangiogenic and antiinflammatory proteins in human amniotic membrane. Cornea 2000;19:348-52. [Crossref] [PubMed]
- Zelen CM, Serena TE, Denoziere G. A prospective randomised comparative parallel study of amniotic membrane wound graft in the management of diabetic foot ulcers. Int Wound J 2013;10:502-7. [Crossref] [PubMed]
- Stock SJ, Kelly RW, Riley SC. Natural antimicrobial production by the amnion. Am J Obstet Gynecol 2007;196:255.e1-6. [Crossref] [PubMed]
- Lim JJ. A Primer on Amniotic Membrane Regenerative Healing. Grand Rapids: MiMedx Group 2015.
- Parolini O, Caruso M. Review: Preclinical studies on placenta-derived cells and amniotic membrane: an update. Placenta 2011;32 Suppl 2:S186-95. [Crossref] [PubMed]
- Parolini O, Solomon A, Evangelista M. Human Term Placenta as a Therapeutic Agent: From the first clinical applications to future perspectives. In: Berven E, ed. Human Placenta: Structure and Development. Hauppauge, NY: Nova Science 2010:1-48.
- Norris MA, Cohen MS, Warren MM. Bladder reconstruction in rabbits with glutaraldehyde-stabilized amniotic membranes. Urology 1982;19:631-5. [Crossref] [PubMed]
- Iijima K, Igawa Y, Imamura T. Transplantation of preserved human amniotic membrane for bladder augmentation in rats. Tissue Eng 2007;13:513-24. [Crossref] [PubMed]
- Salehipour M, Mohammadian R, Jahanbini S. Is amniotic membrane a suitable biomaterial for reconstruction of long ureteral defects? Saudi J Kidney Dis Transpl 2013;24:135-8. [Crossref] [PubMed]
- Shakeri S, Haghpanah A, Khezri A. Application of amniotic membrane as xenograft for urethroplasty in rabbit. Int Urol Nephrol 2009;41:895-901. [Crossref] [PubMed]
- Wang F, Liu T, Yang L. Urethral reconstruction with tissue-engineered human amniotic scaffold in rabbit urethral injury models. Med Sci Monit 2014;20:2430-8. [Crossref] [PubMed]
- Güneş M, Altok M, Güneş A. A Novel Approach to Penile Augmentation Urethroplasty Using Buccal Mucosa and Amniotic Membrane: A Pilot Study in a Rabbit Model. Urology 2016;87:210-5. [Crossref] [PubMed]
- Shakeri S, Masoudi P, Yazdani M. Evaluation of human amniotic membrane as a substitute for transitional epithelium of bladder in dog. J Appl Anim Res 2008;33:55-59. [Crossref]
- Sharifiaghdas F, Naji M, Sarhangnejad R. Comparing supportive properties of poly lactic-co-glycolic acid (PLGA), PLGA/collagen and human amniotic membrane for human urothelial and smooth muscle cells engineering. Urol J 2014;11:1620-8. [PubMed]
- Rolfo A, Giuffrida D, Giuffrida MC. New perspectives for prostate cancer treatment: in vitro inhibition of LNCaP and PC3 cell proliferation by amnion-derived mesenchymal stromal cells conditioned media. Aging Male 2014;17:94-101. [Crossref] [PubMed]
- Sedrakyan S, Da Sacco S, Milanesi A. Injection of amniotic fluid stem cells delays progression of renal fibrosis. J Am Soc Nephrol 2012;23:661-73. [Crossref] [PubMed]
- Burgers JK, Nelson RJ, Quinlan DM. Nerve growth factor, nerve grafts and amniotic membrane grafts restore erectile function in rats. J Urol 1991;146:463-8. [Crossref] [PubMed]
- Koziak A, Marcheluk A, Dmowski T. Reconstructive surgery of male urethra using human amnion membranes (grafts)--first announcement. Ann Transplant 2004;9:21-4. [PubMed]
- Koziak A, Salagierski M, Marcheluk A. Early experience in reconstruction of long ureteral strictures with allogenic amniotic membrane. Int J Urol 2007;14:607-10. [Crossref] [PubMed]
- Barski D, Gerullis H, Ecke T. Repair of a vesico-vaginal fistula with amniotic membrane - Step 1 of the IDEAL recommendations of surgical innovation. Cent European J Urol 2015;68:459-61. [PubMed]
- Razdan S. Protective patch linked to erectile function recovery: 90% of patients receiving membrane during robotic RP regain function at 3 months. Available online: http://urologytimes.modernmedicine.com/urology-times/news/protective-patch-linked-erectile-function-recovery?page=full
- Razdan S. First in the world use of amniotic membrane in robotic prostatectomy for early return of erections. Available online: https://www.youtube.com/watch?v=osfAIT6QTws
- Patel VR, Samavedia S, Bates AS. Dehydrated Human Amnion/Chorion Membrane Allograft Nerve Wrap Around the Prostatic Neurovascular Bundle Accelerates Early Return to Continence and Potency Following Robot-assisted Radical Prostatectomy: Propensity Score-matched Analysis. Eur Urol 2015;67:977-80. [Crossref] [PubMed]
- Amer MI, Abd-El-Maeboud KH, Abdelfatah I. Human amnion as a temporary biologic barrier after hysteroscopic lysis of severe intrauterine adhesions: pilot study. J Minim Invasive Gynecol 2010;17:605-11. [Crossref] [PubMed]
- Amer MI, Abd-El-Maeboud KH. Amnion graft following hysteroscopic lysis of intrauterine adhesions. J Obstet Gynaecol Res 2006;32:559-66. [Crossref] [PubMed]
- Ashworth MF, Morton KE, Dewhurst J. Vaginoplasty using amnion. Obstet Gynecol 1986;67:443-6. [PubMed]
- Chou CT, Lee C, Hwang JL. Amniotic membrane used for vulvar adhesion treatment. Arch Gynecol Obstet 2001;265:223-4. [Crossref] [PubMed]
- Fotopoulou C, Sehouli J, Gehrmann N, et al. Functional and anatomic results of amnion vaginoplasty in young women with Mayer-Rokitansky-Küster-Hauser syndrome. Fertil Steril 2010;94:317-23. [Crossref] [PubMed]
- Mhaskar R. Amniotic membrane for cervical reconstruction. Int J Gynaecol Obstet 2005;90:123-7. [Crossref] [PubMed]
- Zafar M, Saeed S, Kant B. Use of amnion in vaginoplasty for vaginal atresia. J Coll Physicians Surg Pak 2007;17:107-9. [PubMed]
- Price DT, Price TC. Robotic repair of a vesicovaginal fistula in an irradiated field using a dehydrated amniotic allograft as an interposition patch. J Robot Surg 2016;10:77-80. [Crossref] [PubMed]
- Steven L, Cherian A, Yankovic F. Current practice in paediatric hypospadias surgery; A specialist survey. J Pediatr Urol 2013;9:1126-30. [Crossref] [PubMed]
- Duckett JW, Baskin L. Hypospadias In: Adult and Pediatric Urology. 3rd. St. Louis: Mosby 1996.
- Schneuer FJ, Holland AJ, Pereira G. Prevalence, repairs and complications of hypospadias: an Australia population-based study. Arch Dis Child 2015;100:1038-43. [Crossref] [PubMed]
- Bhat A, Mandal AK. Acute postoperative complications of hypospadias repair. Indian J Urol 2008;24:241-8. [Crossref] [PubMed]
- Retik AB, Atala A. Complications of hypospadias repair. Urol Clin North Am 2002;29:329-39. [Crossref] [PubMed]
- Huang LQ, Ge Z, Tian J. Retrospective analysis of individual risk factors for urethrocutaneous fistula after onlay hypospadias repair in pediatric patients. Ital J Pediatr 2015;41:35. [Crossref] [PubMed]
- Pippi Salle JL, Sayed S, Salle A. Proximal hypospadias: A persistent challenge. Single institution outcome analysis of three surgical techniques over a 10-year period. J Pediatr Urol 2016;12:28.e1-7. [Crossref] [PubMed]
- Snodgrass W, Bush N. Tubularized incised plate proximal hypospadias repair: Continued evolution and extended applications. J Pediatr Urol 2011;7:2-9. [Crossref] [PubMed]
- Snodgrass WT, Granberg C, Bush NC. Urethral strictures following urethral plate and proximal urethral elevation during proximal TIP hypospadias repair. J Pediatr Urol 2013;9:990-4. [Crossref] [PubMed]
- Waterman BJ, Renschler T, Cartwright PC. Variables in successful repair of urethrocutaneous fistula after hypospadias surgery. J Urol 2002;168:726-30. [Crossref] [PubMed]
- Fetterolf D, Savage R. Dehydrated human amniotic tissue improves healing time, cost of care. Today's Wound Clinic 2013:19-20.
- Group M. Products: AmnioFix 2016. Available online: http://www.mimedx.com
- Sheikh ES, Sheikh ES, Fetterolf DE. Use of dehydrated human amniotic membrane allografts to promote healing in patients with refractor non-healing wounds. Int Wound J 2014;11:711-7. [Crossref] [PubMed]
- Craig JR, Hotaling JM, Brant WO. Use of Dehydrated Amniotic Membrane Allograft at the Time of Microscopic Denervation of the Spermatic Cord for Chronic Orchialgia Improves Outcomes 2016 Annual Fall Scientific Meeting of SMSNA. Scottsdale, AZ: Sexual Medicine Society of North America, 2016.
- Strom KH, Levine LA. Microsurgical denervation of the spermatic cord for chronic orchialgia: long-term results from a single center. J Urol 2008;180:949-53. [Crossref] [PubMed]