Peyronie’s disease: current therapy
Introduction
Peyronie’s disease is a connective tissue disorder affecting the tunica albuginea of the penis, causing a myriad of problems including penile pain, erectile dysfunction, penile deformity, and difficulty in performing coitus. Francois de la Peyronie first described this in 1743 while he was the surgeon for Louis XIV of France. Although the exact prevalence is unknown, it is relatively common with varying data quoting a prevalence of about 3.2-8.9% with more than 75% of cases occurring in men between 45 and 65 years of age. The incidence of PD following radical prostatectomy is reported to be as high as 15.9% and a recent study showed that penile curvature is a common finding (38.6%) at IPP implantation surgery for ED after prostate cancer treatment (1). The exact etiology is not known but many studies suggest an inciting event causes inflammation of the tunica albuginea with altered wound healing. Examples of inciting events include minor penile trauma during intercourse, history of other genital or perineal injuries, transurethral prostatectomy, and cystoscopy. Other proposed risk factors include diabetes, cigarette smoking, alcohol consumption, hypertension, autoimmune disease, malnutrition, and propranolol administration. There is also a correlation in patients with Dupuytren’s contractures. It has been proposed that Peyronie’s disease has 2 distinct stages: an early/acute inflammatory phase followed by a mature/quiescent stage. Surgery has long been the gold standard for treatment but with improved understanding of the pathophysiology of this disease, more conservative treatment modalities have been used with varying degrees of success.
Oral therapy
Potassium para-aminobenzoate
Potassium para-aminobenzoate (POTABA) is a compound used in the past for treatment for such fibrotic disorders as dermatomyositis and scleroderma. Its efficacy is thought to be due to stabilization of tissue serotonin monoamine oxidase and inhibition of fibroblast glycosaminoglycan secretion (2). Early studies showed its ability to decrease plaque size and penile deviation but none of these were controlled studies. Unfortunately POTABA has shown less promising results in placebo-controlled studies. Weidner et al. published a prospective placebo controlled study in 2005 that showed a statistically significant improvement in plaque size but no effect on penile deviation (2). However, the placebo arm did see a significant deterioration in penile deviation not seen in the treatment arm suggesting POTABA has an additive stabilizing effect. Similar results have been seen in other controlled studies.
Vitamin E, propionyl-l-carnitine
Vitamin E and propionyl-l-carnitine (PLC) are two additional oral therapies used in Peyronie’s treatment. Vitamin E is a potent antioxidant that is known to inactivate free radicals that saturate nitric oxide (NO), thereby keeping active NO levels high and allowing proper wound healing to commence. Propionyl-l-carnitine is a carnitine derivative that has been shown to have an antiproliferative effect on endothelial cells through its ability to stabilize the cell membrane (3). In 2007 a double-blinded placebo controlled study was published investigating the effects of Vitamin E, PLC, and the combination of Vitamin E/PLC (3). They found no significant difference in pain, plaque size, or penile curvature between the three groups.
Colchicine
Colchicine is an antimicrotubule agent thought to be an effective treatment for Peyronie’s disease due to its ability to inhibit collagen secretion from fibroblasts. Safarinejad conducted a 4-month randomized placebo controlled study with oral colchicine versus placebo with over 80 patients enrolled and saw no utility of the drug as there was no significant improvement in penile pain, curvature, or plaque size between the two groups (4). It should also be noted that in the same study there were significant gastrointestinal side effects with approximately 5% of the patients dropping out of the study due to severe diarrhea.
Pentoxifylline
Although most of the oral medications investigated for treatment of Peyronie’s disease have shown poor outcomes in controlled studies, pentoxifylline has fared much better. Pentoxifylline is a nonspecific phosphodiesterase inhibitor with known anti-inflammatory and antifibrogenic properties (5). Because of these properties and the utility of pentoxifylline in the treatment of autoimmune diseases, Safarinejad et al. conducted the first large double-blinded, placebo-controlled study using pentoxifylline in patients with early chronic Peyronie’s disease (5). Over 200 patients were randomized to receive 400 mg of pentoxifylline sustained release (PTX-SR) or placebo over a 6 month period. The results were promising as there were significant decreases in penile plaque size, curvature, progression in the treatment arm (5). Patients also had subjective improvements as the IIEF score was also significantly higher in the treatment are (5). With these results there are sure to be further studies performed to evaluate its efficacy.
Intralesional therapy
Interferons
Interferon injections, particularly interferon alpha 2b, have been explored on the basis of the ability of interferons to alter the metabolic activity of fibroblasts to cause a decrease in collagen production while simultaneously increasing collagenase activity. Various studies have produced drastically conflicting results. Although interferon alpha 2b has been shown to be highly effective in decreasing the penile pain associated with PD, many studies show little to no benefit in decreasing plaque size or degree of penile curvature (6). Some of the trials were not free of side effects as there were high rates of myalgias, fevers, and flu like symptoms; especially in studies where the injections were intralesional. At this time there is little evidence proving intralesional interferons to be an efficacious treatment modality.
Prostacyclins
Prostacyclins have long shown efficacy in treatment of many vascular diseases such as Raynaud’s phenomenon, systemic sclerosis, and peripheral arterial disease. These drugs inhibit fibrosis and stimulate fibrinolysis by inhibiting type I collagen production and inhibiting the expression of vascular cell adhesion molecule-1 (VCAM-1) as well as inter-cellular adhesion molecule-1 (ICAM-1). A small phase I study was conducted in Italy using weekly intralesional iloprost, a prostacyclin analogue, in PD patients with stable, late plaques. After a 5 week treatment course 29% of the patients reported a decrease in penile curvature and pain (7). This will certainly pave the way for future randomized trials using prostacyclins.
Calcium channel blockers
Intralesional calcium channel blockers have been long theorized to provide benefit in Peyronie’s disease with mixed results. This idea is based on the ability of calcium channel blockers to decrease platelet-derived growth factor B-dependent collagen deposition in the extracellular matrix. This was first proposed by Levine et al. in 1994 after he was able to show improvement in subjective plaque narrowing and penile curvature as well as objective improvements in plaque softening, and plaque volume in patients receiving biweekly intralesional verapamil over a 12-week period (8). However, this was a small, non-controlled study in patients with mild, small plaques. This has been contradicted by a recent prospective, randomized, single blind study that showed no statistically significant change in pain, ED, penile curvature, plaque size, or plaque softening in patients also injected biweekly with intralesional verapamil (9). The authors have proposed that their data is likely contradictory to other studies due to their patient population typically having large (>2 cm), mature plaques. At this time there are no large scale placebo controlled studies proving intralesional calcium channel blockers to be efficacious for Peyronie’s disease.
Collagenase
Intralesional collagenase has also provided favorable responses in Peyronie’s disease treatment. Collagenase is an enzyme that lyses collagen types I and III in PD plaques. Intralesional collagenase was first studied by Gelbard et al. in 1982. Gelbard also published the first prospective, double blind study using intralesional collagenase and saw improvement in penile curvature but only in patients with plaques less than 2 cm and less than 20* (10). Jordan et al. was able to see a greater therapeutic effect with decreased angle deviation, plaque width, plaque length, and subjective responses (11). However, this study was not blinded or placebo controlled with only 19 patients completing the study. At this time it is unknown how efficacious intralesional collagenase is but there is a current multicenter placebo-controlled study that is under investigation that should help clarify this.
Transdermal therapy
Iontophoresis/EMDA
Iontophoresis (electromotive drug administration/EMDA) is a non-invasive technique whereby a small electric charge is used to deliver a substance transdermally. This is popular due to the ease of administration as well as the minimal side effect profile because it allows one to bypass hepatic metabolism. Due to the inability of topical verapamil to achieve detectable levels in the tunica albuginea, iontophoresis using verapamil was proposed as an alternative treatment (12). The early results were very promising with several studies showing large improvements in penile curvature but none of the studies were randomized, placebo controlled studies. Greenfield et al. were first to perform a randomized, placebo controlled trial in 2003 with conflicting results to these earlier studies (13). In this study, 42 patients were randomized to semiweekly treatments with either 10 mg verapamil in 4cc saline or just 4cc of saline delivered by electromotive drug administration (EMDA) via the Mini-Physionizer for 20 minutes/session for a 3 month treatment period (13). Although 65% of the treatment group saw a measureable improvement in curvature (mean of 9.1 degrees), there was also improvement in the curvature of the 58% of the placebo group (mean of 7.6 degrees) with no statistical significance seen between the two groups (13). However, in 2005 Di Stasi et al. performed another placebo controlled trial that showed promise, though the study groups differed to the previous study as approximately 70 patients were randomized to either 5 mg of verapamil with 8mg of dexamethasone or 2% lidocaine (14). The treatment schedule was also different with the patients receiving 4 treatments a week for a 6 week period (14). They found a significant decrease in both plaque volume (from 824 to 348 mm3) and penile curvature (from 43 to 21 degrees) while there was no change in plaque volume or curvature in the control group (14). The results between these two studies are drastically different and it has been suggested that the reason could be the different treatment schedules, different treatment combinations and placebos, idea that lidocaine acts as a membrane stabilizer, different evaluation methods, and plaques in different stages. At this point, iontophoresis is a safe treatment modality with varying degrees of success that will need further evaluation before being used as a first line treatment.
Combination therapies
Concomitant ED is found in approximately 1/3rd of Peyronie’s disease. Surgical intervention with penile prosthesis implantation has long been the standard of care with minimal success in less invasive modalities. However, a recent study was performed in Italy in patients with ED and Peyronie’s. The prospective, randomized study revealed significantly higher IIEF-5 scores, QoL scores, and number of patients declaring normal erectile function in patients that underwent ESWL + daily 5 mg tadalafil as compared to only ESWL (15).
Local therapy with devices
Extracorporeal shock wave lithotripsy (ESWL)
Extracorporeal shock wave lithotripsy (ESWL) was first introduced into as a non invasive treatment for Peyronie’s disease with minimal side effects in 1996. A therapeutic effect was postulated on the ability of ESWL to possibly cause plaque damage directly and increase plaque vascularity to bring forth plaque resorption. The efficacy of ESWL is controversial with an exploratory meta analysis of 17 clinical studies revealing ESWL to be effective in subjective measures such as penile pain during erection and sexual function with no improvement in objective measures including plaque size and penile curvature (16). The improvement in pain symptoms is thought to be due to direct disturbance of pain receptors and hyperstimulation analgesia. This analysis was not without flaws as the meta analysis was only exploratory rather than confirmatory because of large differences in the subject medical history and symptoms severity between the study groups as well as inconsistent selection of outcome measures among the studies. At the time of publication there were no controlled, blinded studies performed. The first prospective, randomized, placebo-controlled trial was finally conducted in Italy by Palmieri et al. in 2009 [(17), see Figure 1 below]. Their 100 study patients were randomized to either 4 weeks of ESWL therapy or a non functioning transducer. Results mirrored earlier studies with significant improvement in pain scores on IIEF-5 questionnaires and QofL questionnaires. No statistical significance was found between plaque size or penile curvature between the two groups. However, there was a significant increase in both plaque size and penile curvature in the placebo group suggesting ESWL might be useful in halting plaque progression. In 2010 the International Consultation on Sexual Medicine (ICSM) stated that there is evidence confirming ESWL’s role in improving Peyronie’s related pain but that evidence also exists that ESWL doesn’t improved Peyronie’s deformities (18).
Penile traction
The idea of penile traction has also been explored as a treatment for Peyronie’s disease. Levine et al. published the first trial using penile traction in 2008 with positive results [(19), see Figure 2 below]. Ten patients were enrolled and underwent daily treatment wearing the FastSize Penile Extender for a minimum of 2 hours daily for 6 months. All patients saw a reduction in penile curvature with a mean decrease of 33% as well as increased penile length and girth. All but one patient claimed improvement in sexual function as well. However, it should be noted that this was a small pilot study that was not controlled.
Gontero et al. conducted a similar phase II prospective study with less favorable results in 2009 (20). Nineteen patients were enrolled and subjected to a minimum of 5 hours of daily traction therapy using Androgens for a 6-month period. There was no statistically significant improvement seen in penile curvature or girth but there was a significant increase in length. The authors attributed their conflicting results to patient selection. It remains to be seen how effective penile traction will be for management of PD patients.
Vacuum therapy
Using the idea of the molding technique and penile traction for penile straightening, vacuum therapy has recently been investigated for treatment of Peyronie’s disease. In 2010, Raheem et al. published a case series showing positive outcomes and promise for this modality as a future treatment. This case series involved 31 patients that were subjected to two 10-minute daily sessions using the Osbon ErecAid vacuum pump for a twelve-week period [(21), see Figure 3 below].
Results were promising as there was a significant decrease in penile curvature with 90% of the patients having either a stable degree of curvature or decrease in curvature (range, 5-25 degrees). There were also significant decreases in penile pain and increases in penile length (mean of 0.5 cm) (21). The treatment success was attributed to the thought that the device mechanically stretches the penis and allows for remodeling of the fibrous plaque, which would aid in penile straightening. Although this was a case series with a large dropout rate, this will no doubt spur interest in trials using vacuum therapy as a non-surgical intervention for Peyronie’s disease.
Future treatment modalities
Because transforming growth factor-beta1 (TGF-B1) has shown to play a prominent role in the development of the fibrotic plaques in Peyronie’s disease, some novel therapies have been tested in TGF-B1 pathway. In this pathway, TGF-B type 1 receptors (such as ALK5) are activated which then activates TGF-B1, causing downstream molecules like Smad2 and Smad3 to later induce tissue fibrosis. A recent study in Korea evaluated IN-1130 as an inhibitor of ALK5 in human tissue derived from Peyronie’s plaques and it’s effects on fibroblasts in vivo. This was shown to block TGF-B1 signaling as well as inhibit extracellular matrix production (22). This has shown promise for future animal studies and clinical trials to follow.
Surgical therapy
Surgical therapy has long been considered the gold standard for Peyronie’s treatment. There are 4 common criteria Urologists use to identify surgical need; severe curvature >1 year, stable plaque for >3 months, impaired sexual function secondary to penile curvature, and shortened penis. The three main types of surgical procedures include plication procedures to shorten the convex tunica, grafting to lengthen the concave tunica, and penile prosthesis implantation with grafting.
Carson et al. described the ideal graft as one that is pliable and compliant, has low antigenicity and infection transmission risk, causes minimal inflammation, is packaged, is available in multiple sizes, and is affordable (23).
Plication procedures
Plication procedures and similar procedures such as the Nesbit procedure are the most popular with reconstructive Urologists. The Nesbit procedure was first described by Reed Nesbit in 1965 and then first employed for Peyronie’s treatment by Pryor et al. in 1977 whereby an elliptical excision of tunica albuginea was made opposite to the side of the Peyronie’s plaque, effectively shortening the non effected side and straightening the penile shaft (24,25). A circumglandular incision is made and the penile shaft degloved before inducing an artificial erection with saline injection with the aid of a tourniquet (26). Buck’s fascia is then incised and dissected to expose the tunica before the ellipsis is excised and closed with nonabsorbable suture (26).
The results of the Nesbit procedure have been nothing short of impressive as multiple retrospective studies have shown high rates of patient satisfaction and definitive correction of penile deformities with improvement in sexual function. Savoca et al. retrospectively evaluated almost 300 patients who underwent a Nesbit procedure at a median follow up of 89 months and discovered an almost 84% patient satisfaction rate with approximately 86% of patients reporting definitive correction of their curvature (27). This procedure is not without side effects as 16.5% saw a significant (>1.5 cm) shortening in penile length and 11.5% reporting worsening erectile function and 11% reporting penile sensory changes (27).
With all of the success seen long term with the Nesbit procedure, there have been several variations performed. One such variation utilizes plication without excision of tissue via a penoscrotal approach, thus eliminating the need to delgove the penis. Dugi III et al. first described this technique and the results of a single institution’s 4-year experience in 2010 (28). First, an erection is induced with 10-20 ug of alprostadil before making a 2 cm longitudinal incision at the penoscrotal junction on the side opposite the direction of maximal curvature (28).
The incision is carried down through Buck’s fascia and the tunica albuginea is exposed before a parallel series of nonabsorbable braided sutures are placed in a vertical mattress pattern (28).
Once the correction is straightened adequately the skin in closed in 3 layers and a circumferential dressing is applied (28).
They have reported a high rate of patient satisfaction (93%) with no loss of penile length or sensation (28). Although it was once widely thought that plication procedures are appropriate for penile curvature <60* while any larger degree of curvature greater than 60* should be better served with plaque excision and grafting, a follow up paper was published at the same aforementioned institute showing high success rates with penoscrotal incisions and plication on complex penile deformities (i.e., >60*) (29). This is a modification of a plication procedure first described by Gholami and Lue [2002] that utilized plication sutures on the side opposite of the Peyronie’s plaque without excision of the plaque itself (30). Commonly termed the “Lue 16 dot plication”, 16 (2 pairs) or 24 (3 pairs) of dots are placed approximately 0.5 cm apart and 2-0 polyester sutures are placed full thickness through the tunica albuginea [(30), see Figures 4,5 below]. One knot was placed and clamped with a rubber shod until adequate straightening of the penis was achieved and all of the sutures were then tied with 5 knots (30). The greater the curvature, the greater number of plication sutures needed. If the procedure is being performed for a dorsal curvature then a ventral longitudinal incision is made in the dartos overlying the corpus spongiosum with 1 cm of strip of tissues overlying the cavernosum excised before placing the aforementioned sutures 2 mm lateral to the spongiosum [see illustration below, (1)]. They retrospectively evaluated 132 patients treated with this procedure over a 5 year period and found that 93% of patients claimed to have straight erections at their 6 month follow up with recurrence of curvature reported to be 15% at a mean follow up of 2.6 years (30). They do however; report penile shortening (0.5 to 1.5 cm) in 41% of patients with 7% of patients complaining this shortening affected their sexual activity (30).
There are countless variations of the plication procedure performed today but we will not discuss these due to their similarity to the aforementioned procedures.
Excision and grafting procedures
Although much success has been seen with plication, Nesbit, and other similar procedures, until recently incision/excision and grafting procedures have been utilized for more complex Peyronie’s cases with angles of curvature typically >60*. These procedures are all similar, to some degree, in their method of plaque incision/excision but differ greatly in the type of grafts used. The three main categories of grafts are autologous, xenograft/allograft, and synthetic grafts.
Autologous: Dermal grafts were once popular for grafting materials due to their ability to easily be harvested and a utility in covering large tunical defects but have fallen out of favor due to high rates of de novo ED (approaching 20%) and graft retraction causing loss of penile rigidity (31). The most commonly used autologous graft is the saphenous graft which has slightly fallen out of favor due to high rates of orgasmic and erectile dysfunction. Although the saphenous grafting procedure is not complex in nature, it is not without complications as leg wound infection, prolonged lymphatic leakage, lymphocele formation, and thigh wound hypoesthesia have all been documented (31). Several small studies have also been performed documenting tunica vaginalis and tunica albuginea as grafting materials with mixed results. Buccal mucosa grafting has also been met with mixed results with one study showing high rates of satisfaction with minimal ED and curvature recurrence with another showing just the opposite (31). The significant differences in the results of the two studies were attributed to patient selection strategies. Autologous fascial grafts such as temporalis fascia, fascia lata and rectus sheath can be used and have seen moderate success likely due to their similar morphological makeup, low metabolic demand preventing contraction and fibrosis, and strong flexible composition (31). Although the issue of tissue compatibility is not a factor with autologous grafts, their drawbacks continue to be the longer operative times and associated donor site morbidities (32).
Xenografts/Allografts: xenografts and allografts are graft tissues from another species or person that are composed of extracellular matrices that promote native tissue ingrowth and support. This is achieved through promotion of neovascularization through promotion of angiogenesis and growth factor migration. One type of xenograft utilized in Peyronie’s surgery is small intestinal submucosa, usually composed of porcine jejunum. There are several published case series using porcine small intestine submucosa with vastly varying results. One study reported high success rates with recurrent curvature rates of 9% with a complication rate of 5% while another smaller series had an extremely high complication rate of 37%, mostly attributed to hematoma formation (31). Also seen in the latter study was a recurrence rate of 75%. Lentz et al. believe these complications, especially hematoma, are easily avoidable with the use of aerolized sealant between the graft and tunical defect before closure (31). Bovine pericardium has been used with moderate results as well. The recently found high rates of failure and small study sizes combined with short follow up times have left the utility of xenografts and allografts in question (32).
Synthetic: synthetic grafts have been explored but have fallen out of favor due to increased risk of infections and higher levels of fibrosis compared to other graft types as seen in animal models (33).
Due to this antigenicity and inappropriate functional properties these grafts are essentially obsolete (32).
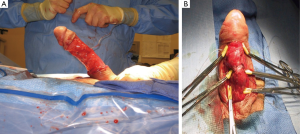
Penile prosthesis implantation with modeling, grafting, or plication
Penile prosthesis implantation with either modeling, grafting, or plication is a valuable option for patients with Peyronie’s and concurrent erectile dysfunction. The inflatable prosthesis (IPP) is preferred in this setting. The method of prosthesis implantation with post implantation manual modeling allows the surgeon to repeat manipulation to achieve maximal correction but runs the risk of possible urethral injury [see Figure 6 below]. IPP implantation with plication utilizes one of the aforementioned “dot” procedures before prosthesis implantation. Finally, IPP implantation with grafting is only indicated for severe persistent curvature >30* with severe indentation or penile shortening.
Conclusions
Although there have been many advances in the treatment of Peyronie’s disease, surgical therapy still remains the most successful treatment modality available. With the many investigational agents currently being investigated there is hope for less invasive treatment options with equivalent results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lin H, Alba F, Romero C, et al. Penile curvature is a common finding at the penile prosthesis implantation for patients with erectile dysfunction after radical prostatectomy. J Urol 2011;abstr 1815.
- Weidner W, Hauck EW, Schnitker J, et al. Potassium paraaminobenzoate (POTABA) in the treatment of Peyronie’s disease: a prospective, placebo-controlled, randomized study. Eur Urol 2005;47:530-5. [PubMed]
- Safarinejad MR, Hosseini SY, Kolahi AA. Comparison of vitamin E and propionyl-L-carnitine, separately or in combination, in patients with early chronic Peyronie’s disease: a double-blind, placebo controlled, randomized study. J Urol 2007;178:1398-403. [PubMed]
- Safarinejad MR. Therapeutic effects of colchicine in the management of Peyronie’s disease: a randomized double-blind, placebo-controlled study. Int J Impot Res 2004;16:238-43. [PubMed]
- Safarinejad MR, Asgari MA, Hosseini SY, et al. A double-blind placebo-controlled study of the efficacy and safety of pentoxifylline in early chronic Peyronie’s disease. BJU Int 2010;106:240-8. [PubMed]
- Brake M, Loertzer H, Horsch R, et al. Treatment of Peyronie’s disease with local interferon-alpha 2b. BJU Int 2001;87:654-7. [PubMed]
- Pavone C, Napoli G, Caruana G, et al. Safety and tolerability of local treatment with iloprost, a prostacyclin analogue, in patients with Peyronie’s disease: a phase I study. BJU Int 2012;110:117-21. [PubMed]
- Levine LA, Merrick PF, Lee RC. Intralesional verapamil injection for the treatment of Peyronie’s disease. J Urol 1994;151:1522-4. [PubMed]
- Shirazi M, Haghpanah AR, Badiee M, et al. Effect of intralesional verapamil for treatment of Peyronie’s disease: a randomized single-blind, placebo-controlled study. Int Urol Nephrol 2009;41:467-71. [PubMed]
- Gelbard MK, James K, Riach P, et al. Collagenase versus placebo in the treatment of Peyronie’s disease: a double-blind study. J Urol 1993;149:56-8. [PubMed]
- Jordan GH. The use of intralesional clostridial collagenase injection therapy for Peyronie’s disease: a prospective, single-center, non-placebo-controlled study. J Sex Med 2008;5:180-7. [PubMed]
- Mulhall JP, Badwan K, Martin D, et al. Does transdermal verapamil applied to the penis infiltrate the tunica albuginea? J Urol 2002;167:abstr 826.
- Di Stasi SM, Giannantoni A, Capelli G, et al. Transdermal electromotive administration of verapamil and dexamethasone for Peyronie’s disease. BJU Int 2003;91:825-9. [PubMed]
- Greenfield JM, Shah SJ, Levine LA. Verapamil versus saline in electromotive drug administration for Peyronie’s disease: a double-blind, placebo controlled trial. J Urol 2007;177:972-5. [PubMed]
- Palmieri A, Imbimbo C, Creta M, et al. Tadalafil once daily and extracorporeal shock wave therapy in the management of patients with Peyronie’s disease and erectile dysfunction: results from a prospective randomized trial. Int J Androl 2012;35:190-5. [PubMed]
- Hauck EW, Mueller UO, Bschleipfer T, et al. Extracorporeal shock wave therapy for Peyronie’s disease: exploratory meta-analysis of clinical trials. J Urol 2004;171:740-5. [PubMed]
- Palmieri A, Imbimbo C, Longo N, et al. A first prospective, randomized, double-blind, placebo-controlled clinical trial evaluating extracorporeal shock wave therapy for the treatment of Peyronie’s disease. Eur Urol 2009;56:363-9. [PubMed]
- Ralph D, Gonzalez-Cadavid N, Mirone V, et al. The management of Peyronie’s disease: evidence-based 2010 guidelines. J Sex Med 2010;7:2359-74. [PubMed]
- Levine LA, Newell M, Taylor FL. Penile traction therapy for treatment of Peyronie’s disease: a single-center pilot study. J Sex Med 2008;5:1468-73. [PubMed]
- Gontero P, Di Marco M, Giubilei G. Use of penile extender device in the treatment of penile curvature as a result of Peyronie’s disease. Results of a phase II prospective study. J Sex Med 2009;6:558-66. [PubMed]
- Raheem AA, Garaffa G, Raheem TA, et al. The role of vacuum pump therapy to mechanically straighten the penis in Peyronie’s disease. BJU Int 2010;106:1178-80. [PubMed]
- Jang JH, Ryu JK, Suh JK. Activin Receptor-Like Kinase 5 Inhibitor Attenuates Fibrosis in Fibroblasts Derived from Peyronie’s Plaque. Korean J Urol 2012;53:44-9. [PubMed]
- Carson CC, Chun JL. Peyronie’s disease: surgical management: autologous materials. Int J Impot Res 2002;14:329-35. [PubMed]
- Nesbit RM. Congenital curvature of the phallus: report of three cases with corrective operation. J Urol 1965;93:230-2. [PubMed]
- Pryor JP, Fitzpatrick JM. A new approach to the correction of the penile deformity in Peyronie’s disease. J Urol 1979;122:622-3. [PubMed]
- Ralph DJ. The Nesbit and Plication Procedures for Peyronie’s Disease. In: Levine LA. eds. Current Clinical Urology: Peyronie’s Disease: A Guide to Clinical Management. Totowa, NJ: Humana Press, 2007:133-44.
- Savoca G, Scieri F, Pietropaolo F, et al. Straightening corporoplasty for Peyronie’s disease: a review of 218 patients with median follow-up of 89 months. Eur Urol 2004;46:610-4. [PubMed]
- Dugi DD 3rd, Morey AF. Penoscrotal plication as a uniform approach to reconstruction of penile curvature. BJU Int 2010;105:1440-4. [PubMed]
- Adibi M, Hudak SJ, Morey AF. Penile plication without degloving enables effective correction of complex Peyronie’s deformities. Urology 2012;79:831-5. [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. [PubMed]
- Lentz AC, Carson CC 3rd. Peyronie’s surgery: graft choices and outcomes. Curr Urol Rep 2009;10:460-7. [PubMed]
- Kadioglu A, Sanli O, Akman T, et al. Graft materials in Peyronie’s disease surgery: a comprehensive review. J Sex Med 2007;4:581-95. [PubMed]
- Leungwattanakij S, Bivalacqua TJ, Yang DY, et al. Comparison of cadaveric pericardial, dermal, vein, and synthetic grafts for tunica albuginea substitution using a rat model. BJU Int 2003;92:119-24. [PubMed]