Successful management of cavernosal artery pseudoaneurysm using microcoil embolization
Introduction
Erectile dysfunction (ED) is a common condition among men and has several causes. In a multinational study of 27,839 men aged 20–75, the overall prevalence of ED was estimated to be 16% worldwide and 22% in the United States (1). Some of the etiologies of ED include neurologic, psychogenic, structural, hormonal, drug-induced, and vasculogenic (2). Among men under the age of 40, pelvic or perineal trauma is the most common cause of ED. Pelvic or perineal trauma often results in arterial injury as the likely mechanism of ED (3,4). In a study of 19 young men who suffered from ED after perineal trauma, cavernosal arterial injury was found in 37% (5). Therefore, arteriogenic ED is a typical presentation of men who suffer from pelvic or perineal trauma.
While post-traumatic, arteriogenic ED is discussed in the literature, there is currently no established standard management for this condition. Management instead depends upon physician experience and preference. We present a 14-year-old adolescent who was diagnosed with a cavernosal artery pseudoaneurysm secondary to blunt perineal and pelvic trauma. He was successfully managed by vascular interventional radiology (VIR) with superselective microcoil embolization. We also review the current literature regarding the management techniques of post-traumatic, arteriogenic ED.
Case presentation
A 14-year-old boy presented to the Urology clinic with a 2-month history of ED related to a blunt force straddle injury in which his urethra was damaged. The patient had been using a suprapubic catheter since the injury and was scheduled for reconstructive urethroplasty. Erectile function at the time of presentation was reported by the patient to be sufficient for penetration but insufficient for maintenance until orgasm. Penile duplex ultrasound after 5U Trimix and 80% erection demonstrated a right-sided corporal pseudoaneurysm with bilateral peak systolic volumes of 9 cm/sec on right and 27 cm/sec on left, and end-diastolic volumes of 2 and 4 cm/sec on the right and left respectively. It was determined at this time that the pseudoaneurysm had a reasonable likelihood of resolving spontaneously and it was safe to proceed with reconstructive surgery as planned. About 10 months after urethroplasty and removal of the suprapubic catheter, the patient was able to attain 50% erection not sufficient for penetration. Referral to interventional radiology was made at this time. Repeat duplex ultrasound revealed that the right-sided corporal pseudoaneurysm had not spontaneously closed.
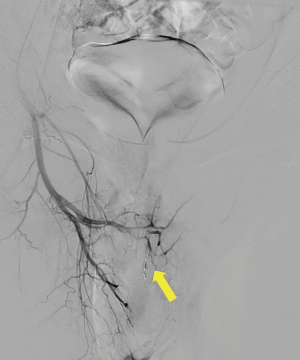
Superselective angiography of the right bulbar penile artery (Figure 1) demonstrated a complex appearing pseudoaneurysm with measurements of 2.4 cm × 1.2 cm (Figure 2). A 2 mm × 4 cm detachable Concerto microcoil was placed within the pseudoaneurysm and feeding vessel (Figure 3). Post-embolization angiography demonstrated complete cessation of blood flow into the pseudoaneurysm and redistribution of flow to the distal aspect of the cavernosal artery (Figure 4). Post-embolization penile duplex ultrasound demonstrated complete resolution of the pseudoaneurysm. At 6-week follow-up after procedure patient reported marked symptomatic improvement.
Discussion
We present a 14-year-old adolescent who was diagnosed with a cavernosal artery pseudoaneurysm secondary to blunt perineal and pelvic trauma who was successfully managed with superselective microcoil embolization. Post-traumatic, arteriogenic ED is typically caused by blunt force trauma to the perineum or incidental trauma sustained during a urologic procedure resulting in arteriovenous fistulae (AVF) or pseudoaneurysm (3). The management of post-traumatic, arteriogenic ED with superselective embolization is well described in the literature. However, there is no consensus regarding the best materials to be used (7). We believe that microcoil and Gelfoam are the preferred techniques for embolization of these defects given their similar outcomes, however choosing between them is a matter of physician preference.
Doppler ultrasound (US) has an important role in the management of post-traumatic arteriogenic ED. Doppler US is used to establish the relationship of ED to trauma as well as to categorize arteriogenic ED based on the pattern of blood flow (8). After embolization of pseudoaneurysms and AVFs, Doppler US is also used to evaluate the cessation of flow through embolized lesions. Doppler US findings vary depending on the type of lesion causing arteriogenic ED, therefore it is important to be able to recognize these findings (3). It should be noted however that diagnosis of arteriogenic ED should be confirmed by penile arteriography (8).
VIR treatment options for pseudoaneurysms and AVFs include procedures such as coil embolization, covered stent placement, stent-assisted coil embolization and transcatheter application of cast-forming agents (Gelfoam) (9). Table 1 shows a review of the recent literature describing embolization of AVFs and pseudoaneurysms causing ED or high flow priapism.

Full table
What can be appreciated is that with all embolization techniques chosen, outcomes are very similar. Erectile function at follow-up returned to normal in all reports—unfortunately results may be biased because negative outcomes are rarely reported. Previous studies have estimated preservation of erectile function after angiographic embolization to be 80% at long term follow-up (8). What can also be appreciated from the literature is an overall trend in recent years towards the use microcoil for pseudoaneurysms and AVFs, likely due to their versatility. Microcoil fibers elicit a thrombogenic response, causing superimposed thrombosis and vessel occlusion. Coils also range in diameter from submillimeter to several centimeters, and include configurations such as straight, helical, spiral, and various three-dimensional shapes, making them a uniquely versatile option. Gelfoam is also a commonly used material for embolization of cavernosal artery. Gelfoam is available a sponge or a powder. The sponge form is typically used for large vessel embolization, as in the case of arteriogenic ED. Vessels embolized with Gelfoam recanalize over the ensuing weeks to months, however, this recanalization can be unpredictable. Autologous clot is also used in the setting of large vessel embolization but clots tend to lyse too quickly for effective treatment (23,24). Given the similar outcomes observed between microcoil and Gelfoam, it can therefore be concluded that both options are equally valid. Our study is limited by having a case report with short follow-up following embolization of cavernosal artery.
Conclusions
Trauma is the most common cause of ED in men under the age of 40. Arteriogenic ED resulting from the formation of pseudoaneurysm or AVF is a typical presentation of post-traumatic ED. We presented the case of a 14-year-old adolescent diagnosed with a pseudoaneurysm causing arteriogenic ED secondary to blunt force trauma to the perineum. We conclude through successful management of this case that superselective embolization is a safe and effective treatment modality for pseudoaneurysm causing arteriogenic ED. We conclude through a review of the literature that the use of microcoil and Gelfoam as the embolizing technique yield similar outcomes. We believe that it is important for urologists to be familiar with the various VIR treatment techniques in order to properly manage post-traumatic arteriogenic ED.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this report and any accompanying images.
References
- Rosen RC, Fisher WA, Eardley I, et al. The multinational Men's Attitudes to Life Events and Sexuality (MALES) study: I. Prevalence of erectile dysfunction and related health concerns in the general population. Curr Med Res Opin 2004;20:607-17. [Crossref] [PubMed]
- Shamloul R, Ghanem H. Erectile dysfunction. Lancet 2013;381:153-65. [Crossref] [PubMed]
- Kim SH, Kim SH. Post-traumatic erectile dysfunction: doppler US findings. Abdom Imaging 2006;31:598-609. [Crossref] [PubMed]
- Donatucci CF, Lue TF. Erectile dysfunction in men under 40: etiology and treatment choice. Int J Impot Res 1993;5:97-103. [PubMed]
- Penson DF, Seftel AD, Krane RJ, et al. The hemodynamic pathophysiology of impotence following blunt trauma to the erect penis. J Urol 1992;148:1171-80. [Crossref] [PubMed]
- Masterson JM, Savio LF, Ramasamy R, et al. Successful management of cavernosal artery pseudoaneurysm using microcoil embolization. Asvide 2017;4:443. Available online: http://www.asvide.com/articles/1762
- Lloret F, Martínez-Cuesta A, Domínguez P, et al. Arterial microcoil embolization in high flow priapism. Radiologia 2008;50:163-7. [Crossref] [PubMed]
- Kim SH. Doppler US evaluation of erectile dysfunction. Abdom Imaging 2002;27:578-87. [Crossref] [PubMed]
- Celtikci P, Ergun O, Tatar IG, et al. Superselective arterial embolization of pseudoaneurysm and arteriovenous fistula caused by transurethral resection of the prostate. Pol J Radiol 2014;79:352-5. [Crossref] [PubMed]
- Dallas KB, Guo D, Harris C, et al. Intermittent Projectile Urethraggia: An Unusual Sequela of a Skateboarding Accident in an Adolescent Male. Urology 2017. [Epub ahead of print]. [Crossref] [PubMed]
- José CS, Nicolás BP, Pablo AA, et al. Urethrorrhagia Secondary to Traumatic Penile Pseudoaneurysm. Urol Case Rep 2016;7:10-3. [Crossref] [PubMed]
- Tan ZY, Burnes J. Post-traumatic pre-pubertal high-flow priapism: bilateral superselective embolisation. J Med Imaging Radiat Oncol 2011;55:498-501. [Crossref] [PubMed]
- Ringe KI, Waalkes S, Herrmann T, et al. Superselective transarterial coil embolization for therapy of high-flow priapism: a case report. Urologe A 2010;49:747-9. [Crossref] [PubMed]
- Sandler G, Chennapragada SM, Soundappan SS, et al. Pediatric high-flow priapism and super-selective angiography--an Australian perspective. J Pediatr Surg 2008;43:1898-901. [Crossref] [PubMed]
- Towbin R, Hurh P, Baskin K, et al. Priapism in children: treatment with embolotherapy. Pediatr Radiol 2007;37:483-7. [Crossref] [PubMed]
- Lee YC, Shen JT, Shih MC, et al. Bilateral superselective arterial microcoil embolization in post-traumatic high-flow priapism: a case report. Kaohsiung J Med Sci 2003;19:79-83. [Crossref] [PubMed]
- Volkmer BG, Nesslauer T, Kraemer SC, et al. Prepubertal high flow priapism: incidence, diagnosis and treatment. J Urol 2001;166:1018-23. [Crossref] [PubMed]
- Talic RF, Al-Damegh SA. Post traumatic high-flow arterial priapism. The need for increased awareness among health care professionals. Saudi Med J 2000;21:382-5. [PubMed]
- Mourikis D, Chatziioannou AN, Konstantinidis P, et al. Superselective microcoil embolization of a traumatic pseudoaneurysm of the cavernosal artery. Urol Int 2000;64:220-2. [Crossref] [PubMed]
- de Pablo Cárdenas A, Jiménez Calvo JM, Grasa Lanau V, et al. High-flow priapism in the pediatric age Arch Esp Urol 1999;52:862-9. review. [PubMed]
- Neubauer S, Derakhshani P, Krug B, et al. Posttraumatic high-flow priapism in a 10-year-old boy: superselective embolization of the arteriovenous fistula. Eur Urol 1998;33:337-9. [Crossref] [PubMed]
- Miller SF, Chait PG, Burrows PE, et al. Posttraumatic arterial priapism in children: management with embolization. Radiology 1995;196:59-62. [Crossref] [PubMed]
- Yesilkaya Y, Peynircioglu B, Gulek B, et al. Autologous blood-clot embolisation of cavernosal artery pseudoaneurysm causing delayed high-flow priapism. Pol J Radiol 2013;78:54-6. [Crossref] [PubMed]
- Lubarsky M, Ray CE, Funaki B. Embolization agents-which one should be used when? Part 1: large-vessel embolization. Semin Intervent Radiol 2009;26:352-7. [Crossref] [PubMed]




