Describing the learning curve for bulbar urethroplasty
Introduction
Learning curves have been described for a number of urological procedures including radical prostatectomy and laparoscopic nephrectomy but rarely for urethroplasty. The criteria used to define learning curves vary from: time to optimum operative duration, time to minimum serious adverse effects or time to optimum long-term functional outcomes (1). Bulbar urethroplasty, in its various forms, is the commonest and simplest type of urethroplasty performed (2). We describe the learning curve in a single surgeon’s series of bulbar urethroplasties in terms of time to optimum stricture recurrence rates.
Methods
A retrospective case note review of a prospectively acquired database of 91 consecutive men of median age 32 years (range, 15–66 years) having bulbar urethroplasty performed between 2004 and 2011 by a single surgeon following training in a Specialist Unit was performed. Data was collected on: patient demographics, type of urethroplasty, restricture rate (as defined by routine urethrogram or urethrogram to investigate recurrent symptoms) and duration of follow up.
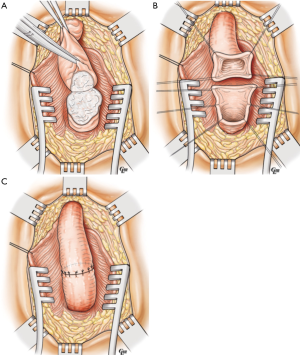
BBA was performed by: excision of stricture, 1 cm spatulation of the ventral aspect of the distal segment and of the dorsal aspect of the proximal segment (Figure 1A-C: Bulbo-Bulbar Anastomotic Urethroplasty) (3-5).
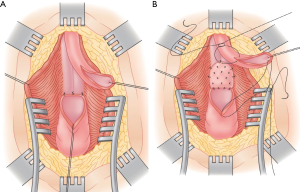
Augmented BBA was conducted by excision of the stricture, 1cm dorsal spatulation of both urethral segments and dorsal onlay of cheek BMG (Figure as per Webster’s description (Figure 2A,B; Augmented Bulbo-Bulbar Urethroplasty) (6).
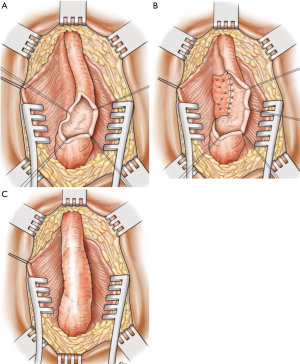
Dorsal onlay was conducted as per Barbagli (7) with dorsal stricturotomy 1cm into healthy tissue either side of stricture and dorsal onlay of cheek BMG (Figure 3A-C; Dorsal Onlay Buccal Mucosal Graft Urethroplasty).
All urethroplasties were performed in standard social lithotomy position, using a 16 Ch silicone catheter and patients discharged home after a 23-hour stay (the following day) unless social problems prevented this (4 patients).
All patients had a pericatheter urethrogram performed in the uroradiology department at 3 weeks post surgery with removal of catheter at this time if healed (N=73 or 80%). For those patients with leakage documented on urethrogram at 3 weeks post surgery, further weekly urethrograms were performed until healing was documented and catheter removed (all <6 weeks).
All patients had FR, PVR and ascending and descending urethrogram preoperatively and at 3, 12, 24 and 36 months post surgery. Patients were thereafter instructed to contact us on an as required basis if they had any concerns or symptoms.
The restricture rates were compared by quartiles (first 25%, second 25%, third 25% and fourth 25% of bulbar urethroplasties performed) and statistical analysis was by χ2 between the first and fourth quartiles.
Results
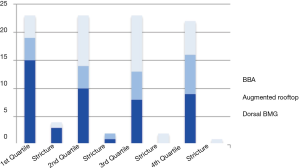
The 91 men had 42 dorsal onlay buccal mucosal graft (Dorsal BMG), 20 BMG augmented bulbobulbar anastomotic (Augmented Rooftop) and 29 bulbobulbar anastomotic (BBA) urethroplasties performed. Median follow up was 39 months for the first quartile, 42 months for the second, 36 months for the third, and 35 months for the fourth. The number of restrictures per quartile is demonstrated in Figure 4.
Restricture occurred in 9 (9.9%) of patients: 4/23 in the first quartile (17%); 2/23 in the second quartile (8.7%); 2/23 in the third quartile (8.7%); and 1/22 in the fourth quartile (4.5%).
There were no restrictures noted after 24 months. There was a significantly different (χ2 P<0.01) and clinically important reduction in restricture rate from first quartile (17%) to fourth quartile (4.5%).
Discussion
To our knowledge this is the first report of a learning curve for bulbar urethroplasty alone. Bulbar urethroplasty is perhaps the simplest type of urethroplasty and as such minimum numbers to achieve stable and optimum restricture rates are highly relevant as they will also be applicable as minimum number guides for the more complex procedures of penile and posterior urethroplasty. The suggestion that it may take as many as 90 bulbar urethroplasties to obtain optimal stricture recurrence rates is supported by the data from Faris et al. (8). Their recently published study analyzed success at 18 months in 613 consecutive cases of bulbar and penile urethroplasty performed by 6 specialist surgeons. They found an 88.2% success for bulbar and a 78.3% success for penile urethroplasty at 18 months post surgery. There was a statistically significant trend to improvement in outcomes and reduction in complications especially with bulbar urethroplasty. They concluded that a minimum of 70 bulbar urethroplasties were required before optimal proficiency occurred (defined as success >90%). Rompré et al. (9) found a similar learning curve for TIP urethroplasty in pediatric urology with a reduction in complications to plateau observed after 50–75 cases.
This is at variance with Fossati et al. in 2016 (10) who looked again at learning curves for both bulbar and penile urethroplasty. This time the learning curve was defined upon long-term outcomes for 564 urethroplasties with a median follow-up 69 months. The overall 5-year success rate was 77% and they concluded that long-term outcomes failed to plateau even after 500 cases. The inclusion of penile urethroplasty outcomes in this data may well be responsible for this extended learning curve.
Learning curves have been looked at for many urological procedures in particular laparoscopic and robotic procedures. Various surrogate and true quality outcomes have been assessed including: operative time, early complication rates, late complication rates and histological outcomes (10-16). Medium or long-term functional outcomes have rarely been addressed.
Conclusions
There appears to be a learning curve for bulbar urethroplasty. A significantly reduced restricture rate was noted with each quartile increase in number of bulbar urethroplasty performed. It may take as many as 90 cases to reach restricture plateau and optimize urethroplasty outcomes.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Abboudi H, Khan MS, Guru KA, et al. Learning curves for urological procedures: a systematic review. BJU Int 2014;114:617-29. [Crossref] [PubMed]
- Mundy AR, Andrich DE. Urethral Strictures. BJU Int 2011;107:6-26. [Crossref] [PubMed]
- Turner-Warwick R. Urethral stricture surgery. In: Mundy AR. editor. Current Operative Surgery + Urology. London: Balliere Tindall, 1988:160-218.
- Eltahawy EA, Virasoro R, Schlossberg SM, et al. Long-term followup for excision and primary anastomosis for anterior urethral strictures. J Urol 2007;177:1803-6. [Crossref] [PubMed]
- Santucci RA, Mario LA, McAninch JW. Anastomotic urethroplasty for bulbar urethral stricture: analysis of 168 patients. J Urol 2002;167:1715-9. [Crossref] [PubMed]
- Guralnick ML, Webster GD. The augmented anastomotic urethroplasty: indications and outcome in 29 patients. J Urol 2001;165:1496-501. [Crossref] [PubMed]
- Barbagli G, Selli C, Tosto A, et al. Dorsal free graft urethroplasty. J Urol 1996;155:123-6. [Crossref] [PubMed]
- Faris SF, Myers JB, Voelzke BB, et al. Assessment of the Male Urethral Reconstruction Learning Curve. Trauma and Urologic Reconstruction Network of Surgeons (TURNS). Urology 2016;89:137-42. [Crossref] [PubMed]
- Rompré MP, Nadeau G, Moore K, et al. Learning curve for TIP urethroplasty: A single-surgeon experience. Can Urol Assoc J 2013;7:E789-11. [PubMed]
- Fossati N, Barbagli G, Larcher A, et al. The Surgical Learning Curve for One-stage Anterior Urethroplasty: A Prospective Single-surgeon Study. Eur Urol 2016;69:686-90. [Crossref] [PubMed]
- Srivastava A, Sureka SK, Vashishtha S, et al. Single-centre experience of retroperitoneoscopic approach in urology with tips to overcome the steep learning curve. J Minim Access Surg 2016;12:102-8. [Crossref] [PubMed]
- Chang Y, Qu M, Wang L, et al. Robotic-Assisted Laparoscopic Radical Prostatectomy From a Single Chinese Center: a Learning Curve Analysis. Urology 2016;93:104-11. [Crossref] [PubMed]
- Roman A, Ahmed K, Challacombe B. Robotic partial nephrectomy - Evaluation of the impact of case mix on the procedural learning curve. Int J Surg 2016;29:132-6. [Crossref] [PubMed]
- Linder BJ, Anand M, Weaver AL, et al. Assessing the learning curve of robotic sacrocolpopexy. Int Urogynecol J 2016;27:239-46. [Crossref] [PubMed]
- Kretschmer A, Mandel P, Buchner A, et al. Surgical learning curve for open radical prostatectomy: Is there an end to the learning curve? World J Urol 2015;33:1721-7. [Crossref] [PubMed]
- Komori M, Izaki H, Daizumoto K, et al. Complications of Flexible Ureteroscopic Treatment for Renal and Ureteral Calculi during the Learning Curve. Urol Int 2015;95:26-32. [Crossref] [PubMed]