Penile rehabilitation after radical prostatectomy: patients’ attitude and feasibility in China
Introduction
Prostate cancer (PCa) is the second most frequently diagnosed cancer and the sixth leading cause of cancer death in males, accounting for 14% [903,500] of the total new cancer cases and 6% [258,400] of the total cancer deaths in males in 2008 (1). In contrast to the trends in Western countries, incidence and mortality rates of PCa are rapidly rising in several Asian countries, such as China. An eightfold increase from 0.8 to 6.9 PCa cases per 100,000 person-years was reported in Shanghai in the past 30 years (2).
Radical prostatectomy (RP) is the gold standard therapeutic option for patients with clinically localized prostate cancer who have a life expectancy of longer than 10 years (3). Despite several improvements in surgical technique, the rate of erectile dysfunction (ED) after surgery ranges from 20% to 90% in patients treated with bilateral nerve-sparing radical prostatectomy (BNSRP) (4). Consequently, ED has the most negative impact on patients’ health-related quality of life (HRQoL) in the long run (5). In this context, penile rehabilitation, which means the use of drugs and/or devices following RP to maximize the chances of erectile function recovery, is warranted.
Although penile rehabilitation of post-RP patients is a prevalent practice among American Urological Association (AUA), International Society for Sexual Medicine (ISSM) and French urologists, there’s no data about its use in developing country, such as China (6-8). Rehabilitation patterns and patients’ attitude towards accepting penile rehabilitation to recover their erectile function are largely unknown.
In this study, we retrospectively studied the behavior in a series of Chinese patients after RP who were offered the penile rehabilitation to assess their attitude towards this treatment and to identify indicators and reasons for refusal. We think this can help us to evaluate the feasibility and necessity for penile rehabilitation after RP in Chinese patients.
Materials and methods
From January 2011 to March 2012, a series of Chinese PCa patients who underwent RP, either nerve-sparing or non-nerve-sparing, at Fudan University Shanghai Cancer Center were included in this study. The day before surgery, after obtaining informed consent, we administered the abridged 5-item International Index of Erectile Function (IIEF-5) to acquire data on each patient’s physiological and sexual history, together with a short questionnaire to gain information about his attitude towards sexual life and penile rehabilitation post-RP: (I) Do you wish to preserve sexual activity after surgery? (II) Do you have interest in penile rehabilitation to recover your erectile function?
At our institution, we recommended to all patients who had a wish to preserve sexual activity after they underwent RP, whether nerve-sparing or non-nerve-sparing, to participate in the penile rehabilitation in one of interventions as follows: phosphodiesterase type 5 inhibitor (PDE-5i); vacuum erection device (VED) or combination of both (PDE-5i together with VED). Patients were provided with information about the usefulness of rehabilitation, the efficacy and potential complications of each intervention, as well as the administration protocol. Sildenafil (Pfizer Inc, Shanghai, China) was prescribed as PDE-5i at the dose of 50 mg once daily at nighttime. Osbon ErecAid (Timm Medical, MN, USA) was used as VED. The men were instructed to inflate the device for two consecutive 5-min periods after a brief release of suction in between inflations, and were allowed to use the constriction band for intercourse if desired until second month after RP. None of the medications, such as prostaglandin E1 or papaverine for patients’ intracavernosal injection or urethral suppositories insertion by themselves, was available in China so far.
Descriptive statistics included frequencies for discreet variables: the rehabilitation rate (percentage of patients who accept penile rehabilitation), the median rehabilitation initiation time and duration time, and the reasons for patients’ refusing penile rehabilitation. We used univariate analysis (t-test or chi-square test) to compare patients participating in rehabilitation with those not doing so to identify indicators of participating rehabilitation post-RP. The successful intercourse rate six months after treatment was compared among three rehabilitation interventions using Fisher’s exact test. All statistic analyses were outlined with SPSS 16.0 (SPSS Inc., Chicago, IL, USA.). A P<0.05 was considered to indicate statistical significance.
Results
A total of 187 patients underwent RP in our institution. Their mean age was 65.6 years. Of 187 patients 141 (75.4%) reported being sexually active in the six months before RP; 122 (65.2%) wished to preserve sexual activity and 80 (42.8%) had interest in penile rehabilitation after RP (Table 1).

Full table
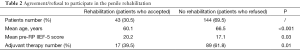
The penile rehabilitation was accepted by 43 (30.5%) patients and refused by 144 (69.5%) post-RP. The median [range] initiation time of penile rehabilitation was 6 months (range: 1-18 months). The median [range] rehabilitation duration was 6 months (range: 3-18 months) (Table 1). Patients who accepted the penile rehabilitation were younger (60.1 vs. 66.5, P<0.001) and had a higher mean pre-RP IIEF-5 score (20.2 vs. 17.1, P=0.03) than those who did not (Table 2). In addition, the adjuvant therapy (hormonal and/or radiation therapy) significantly decreased the number of patients who accepted the penile rehabilitation (P=0.01, Table 2).
Full table
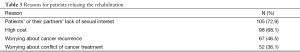
With respect to the reasons for patients not to accept the rehabilitation, there were 105 (72.9%) patients’ or their partners’ lack of sexual interest and 98 (68.1%) patients’ refusal for high cost of rehabilitation. Meanwhile, refusal to participation was also attributed to other reasons: 52 (36.1%) patients worried that penile rehabilitation would conflict with their cancer treatment; 67 (46.5%) patients worried that PCa would recur under the rehabilitation strategies (Table 3).
Full table
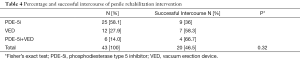
Of the 43 patients who accepted the rehabilitation, 25 (58.1%) used PDE-5i only, 12 (27.9%) used VED only and 6 (14.0%) attempted the combination rehabilitation therapy. The successful intercourse rate of all patients who accepted the rehabilitation was recorded as 46.5%. There was no significant difference in each treatment, with 36% for PDE-5i only, 58.3% for VED only and 66.7% for combination therapy, respectively (P=0.32, Table 4).
Full table
Discussion
Post-RP ED may be caused by cavernous nerve trauma, insufficient arterial inflow, absence of cavernosal oxygenation, neuropraxia-associated damage to erectile tissue resulting in veno-occlusive dysfunction, or any combination of these factors (9). The concept of penile rehabilitation revolves around the use of a medication, combination of medications, and/or devices to preserve erectile tissue health (10). It’s suggested that these options should be considered in the early postoperative period to promote erections and to improve caver-nosal oxygenation, which in turn may play a role in limiting corporal fibrosis (11).
In this study, we found 75.4% of Chinese patients were sexually active preoperatively and 65.2% wished to preserve sexual activity post-RP. This was surprisingly close to the multi-centric observational study, showing 69.2% of Europeans were interested in preserving sexual activity post-RP (12). In the past thirty years, the Chinese economy has developed to the second largest in the world after that of the United States, which has led the Chinese population to enjoy their life and to look for high quality of life. Moreover, the western culture introduced by the opening-up reform makes Chinese people open their mind and awaken their sexual consciousness. The Chinese life expectancy also rose a lot. For example in some developed cities such as Shanghai, the registered residents’ life expectancy in 2010 reached 79.82 for men. We think these factors may contribute to the Chinese patients’ similarly high wish for preserving their sexual activity post-RP.
Our study showed 42.8% of patients had interest in penile rehabilitation after RP. However, only 30.5% of patients accepted the rehabilitation program, which was lower than the response rate of 51% and 63.5% in previous studies (13,14). Meanwhile, we found several factors contributing to these responses, such as age, IIEF-5 score preoperatively and adjuvant therapy like hormonal manipulation or radiation, which were also demonstrated by the previous study (14). Besides, the low response rate in our study was also attributed to common reasons. As a result, patients’ or their partners’ lack of sexual interest ranked the first reason. However, we found that many patients also worried penile rehabilitation would conflict with their cancer treatment or even make the tumor recur. This implicated a part of Chinese PCa patients had a misunderstanding about the role and mechanism of penile rehabilitation. Unlike previous investigations (13,14), we demonstrated high cost of rehabilitation program stated as one of the main reasons for refusal of rehabilitation in Chinese PCa patients. Nowadays, the cost for ED treatment by either PDE-5i or VED was not covered by the Chinese National Medical Insurance. Consequently, many Chinese PCa patients, who refused to participate in rehabilitation, considered a total cost of 1,500 US dollars using PDE-5i and/or 800 US dollars using VED for 6 months’ rehabilitation would yield an extra cost for their family.
The median initiation time of penile rehabilitation in our study was six months post-RP, which was much later than that in previous surveys of AUA members, ISSM members and French Urologists (6-8). They started the rehabilitation immediately at/after patients’ catheter removal or within 3 months post-RP. Meanwhile, the median rehabilitation duration in our study was six months, nearly half of that in previous surveys (6-8). Together with the low response rate of rehabilitation in China, the different practice pattern was also contributed to another two aspects: one is the traditional Chinese culture and the other is the Chinese doctors who perform rehabilitation for RP patients. In China, it’s still considered shameful to talk about sex in public, especially for the elders. Many patients and their partners felt embarrassing when doctors asked their sexual history and sexual needs after surgery. Besides, some theories in the traditional Chinese medicine also state that it’s not good for the patient to preserve sexual life after cancer treatment. Penile rehabilitation after RP was introduced to China recently. Lack of adequate education made urologists pay little attention to performing rehabilitation after RP. Moreover, some urologists were not interested in preserving patients’ sex lives by themselves. These inadequate consultations and inactive support from doctors also make penile rehabilitation an uncommon practice for RP patients in China.
The present study demonstrated over fifty percent of patients accepted PDE-5i as their rehabilitation option followed by VED and a combination of both. PDE-5i was most commonly and easily accepted by patients as it was a convenient, safe and effective strategy for penile rehabilitation which had been proven in previous studies (15-17). It was remarkable that there were 42% of patients using VED or as a combination option for rehabilitation, which was higher than that in previous studies (7). Early intervention with the daily use of VED had been shown to preserve penile length (18,19). Therefore, the relatively high acceptance of VED use for rehabilitation implicated many Chinese RP patients did care about their penile size together with their erectile function. As the sample size was limited, the successful intercourse rates during the six months after treatment were not statistically different among three interventions. Although the combination intervention seems to be more effective, a randomized controlled study is needed to compare the outcome among each penile rehabilitation option.
This was a single center study in a developed city of China, which was also a limitation besides the sample size. However, our institution was a good representative of a typical institution in China with more and more RP patients. Anyway, we think the results of the present study can tell people the status and feasibility of penile rehabilitation in China.
Conclusions
Results from the current study indicated that less than one-third of Chinese RP patients accepted penile rehabilitation postoperatively. Patients’ attitude towards rehabilitation was conservative with a late initiation time and a short duration time. The reasons for this attitude and low rehabilitation rate were attributed to many reasons from traditional Chinese culture, doctors and patients themselves. Penile rehabilitation is feasible and effective in Chinese RP patients with only PDE-5i and VED available in China today.
Acknowledgements
Funding: This study was supported in part by grants from 985 phase III project of Fudan University (D.W.Y) and Youth Fund of Shanghai Municipal Health Bureau (Y.J.S).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [PubMed]
- Cullen J, Elsamanoudi S, Brassell SA, et al. The burden of prostate cancer in Asian nations. J Carcinog 2012;11:7. [PubMed]
- Catalona WJ, Ramos CG, Carvalhal GF. Contemporary results of anatomic radical prostatectomy. CA Cancer J Clin 1999;49:282-96. [PubMed]
- Tal R, Alphs HH, Krebs P, et al. Erectile function recovery rate after radical prostatectomy: a meta-analysis. J Sex Med 2009;6:2538-46. [PubMed]
- Madalinska JB, Essink-Bot ML, de Koning HJ, et al. Health-related quality-of-life effects of radical prostatectomy and primary radiotherapy for screen-detected or clinically diagnosed localized prostate cancer. J Clin Oncol 2001;19:1619-28. [PubMed]
- Tal R, Teloken P, Mulhall JP. Erectile function rehabilitation after radical prostatectomy: practice patterns among AUA members. J Sex Med 2011;8:2370-6. [PubMed]
- Teloken P, Mesquita G, Montorsi F, et al. Post-radical prostatectomy pharmacological penile rehabilitation: practice patterns among the international society for sexual medicine practitioners. J Sex Med 2009;6:2032-8. [PubMed]
- Chartier-Kastler E, Amar E, Chevallier D, et al. Does management of erectile dysfunction after radical prostatectomy meet patients’ expectations? Results of a national survey (REPAIR) by the French Urological Association. J Sex Med 2008;5:693-704. [PubMed]
- Magheli A, Burnett AL. Erectile dysfunction following prostatectomy: prevention and treatment. Nat Rev Urol 2009;6:415-27. [PubMed]
- Mulhall JP, Bella AJ, Briganti A, et al. Erectile function rehabilitation in the radical prostatectomy patient. J Sex Med 2010;7:1687-98. [PubMed]
- Wang R. Penile rehabilitation after radical prostatectomy: where do we stand and where are we going? J Sex Med 2007;4:1085-97. [PubMed]
- Imbimbo C, Creta M, Gacci M, et al. Patients’ desire to preserve sexual activity and final decision for a nerve-sparing approach: results from the MIRROR (Multicenter Italian Report on Radical Prostatectomy Outcomes and Research) Study. J Sex Med 2011;8:1495-502. [PubMed]
- Salonia A, Gallina A, Zanni G, et al. Acceptance of and discontinuation rate from erectile dysfunction oral treatment in patients following bilateral nerve-sparing radical prostatectomy. Eur Urol 2008;53:564-70. [PubMed]
- Polito M, d’Anzeo G, Conti A, et al. Erectile rehabilitation with intracavernous alprostadil after radical prostatectomy: refusal and dropout rates. BJU Int 2012;110:E954-7. [PubMed]
- Padma-Nathan H, McCullough AR, Levine LA, et al. Randomized, double-blind, placebo-controlled study of postoperative nightly sildenafil citrate for the prevention of erectile dysfunction after bilateral nerve-sparing radical prostatectomy. Int J Impot Res 2008;20:479-86. [PubMed]
- Montorsi F, Nathan HP, McCullough A, et al. Tadalafil in the treatment of erectile dysfunction following bilateral nerve sparing radical retropubic prostatectomy: a randomized, double-blind, placebo controlled trial. J Urol 2004;172:1036-41. [PubMed]
- Montorsi F, Brock G, Lee J, et al. Effect of nightly versus on-demand vardenafil on recovery of erectile function in men following bilateral nerve-sparing radical prostatectomy. Eur Urol 2008;54:924-31. [PubMed]
- Köhler TS, Pedro R, Hendlin K, et al. A pilot study on the early use of the vacuum erection device after radical retropubic prostatectomy. BJU Int 2007;100:858-62. [PubMed]
- Dalkin BL, Christopher BA. Preservation of penile length after radical prostatectomy: early intervention with a vacuum erection device. Int J Impot Res 2007;19:501-4. [PubMed]


