Pure transumbilical approach for oncologic surgeries of the male pelvis is now closer to become a reality
Urologic surgery has always been pioneer to promote minimally invasive surgery in the last decades of the history of medicine. Transurethral resection, extracorporeal shock wave lithotripsy, retrograde intrarenal surgery, ureterorenoscopy, and percutaneous nephrolithotomy are some good examples of this evolution. Nowadays kidney tumors, previously requiring high morbidity incisions, such as lumbotomy, are treated routinely in most centers by regular or robot-assisted laparoscopy. It is not surprising that the medical specialty best prepared to give impetus to these new minimally invasive techniques has been Urology.
Laparoendoscopic single-site surgery (LESS) has become widely applicable in different urological settings, especially for renal surgery, life-donor nephrectomy and reconstructive procedures (1). New technical developments that include the application of precise manual and robotic systems are contributing to further development of this field, especially in urologic pelvic surgery where LESS surgery has not been so popular (2,3). However, it is evident that LESS application for prostate and bladder cancer surgery remains one of the least used indications, possibly for the drawback that constitutes performance of such time-consuming and complex procedures like radical prostatectomy or radical cystoprostatectomy, lymph node dissection and urinary diversion (4,5). In fact, once performed the extirpative procedure with oncologic safety (i.e., disease control with adequate surgical margins and also optimized surgical results regarding potency and continence), the exigent steps of an accurate reconstructive surgery, sometimes including an orthotopic neobladder, must follow. This is the main reason for the undeniable drawback to perform surgical urologic oncology procedures through an ultra-minimally invasive approach such as transumbilical surgery.
The navel, due to its topographical situation, is one of the most suitable places for LESS, as it allows an access to both renal and retroperitoneal surgery. Moreover, strictly speaking, umbilical LESS is an embryonic natural orifice transluminal endoscopic surgery (E-NOTES), since the navel is a natural embryonic opening and the scar of an umbilical surgery can be completely hidden within the natural scar itself. That is why umbilical surgery is an option equally attractive for men than vaginal surgery for females, as it totally fulfills the criteria to be considered “surgery without incision” or “scarless surgery” (2). Surgery through a multichannel single port placed in the umbilicus can be performed using both conventional straight laparoscopic instruments and desirably using new curved or flexible instruments that allow an optimal degree of deflection (6,7).
The first description of a LESS procedure was a tubal ligation performed in 1972 through a 1-cm infraumbilical incision, with a laparoscopy optic inserted to identify and cauterize each fallopian tube (8). The cosmetic benefit of this technique led gynecologists to explore more complex procedures, including umbilical hysterectomy with double adnexectomy in 1991 (9). General surgeons also began to explore the benefits of umbilical surgery to perform appendectomies and cholecystectomies (10,11). The first transumbilical urological procedure with multiple trocars was a nephrectomy, described by Raman et al. in 2007 (12). In the following years the experience increased exponentially using different single-port devices, either reusable or disposable (and sometimes even handmade) both through conventional or robotic-assisted laparoscopy (1). However, in the very recent years the umbilical urological experience has cooled down and suffered an important drawn-back, waiting for the development of more precise and helpful technical developments to ease difficulties and save both time and surgical effort. Also the notorious movement of most of the well-experienced and very skilful urologic surgeons to robotic platforms is another explanation for the current slow-down of development within the field of laparoscopic LESS (13,14). There is no doubt that currently developed laparoscopic aids cannot be better or more precise than the not-totally yet developed robotic platforms and systems that hopefully will allow utmost technically efficient robotic-NOTES complex surgeries in a near future.
At the beginning of LESS surgery, surgeons performed the procedures with conventional laparoscopic instruments through a single skin incision accompanied by several fascial incisions (7). Articulated clamps, endobag and standard endoclips were used, along with a 5-mm and 45◦ rigid optic. A significant clushing of intra and extracorporeal instruments with very limited maneuverability, lack of vision, and difficulty for vascular control are easily recognized and constitute the major step backwards for widespread use of umbilical surgery, at least in its present form. Besides, a very significant learning curve needing specific teaching programs is another unfortunate reality (15). Rapid innovation is needed to effectively face the difficulties inherent to complex surgical techniques, such as radical prostatectomy or radical cystectomy, including reduced visual field in which all the instruments are in parallel.
With the aim to overcome these difficulties, we developed and standardized a new single-port surgical approach to be used through an occult umbilical incision, composed of a multichannel reusable device named KeyPort® (Richard Wolf GmBH, Knittlingen, Germany), optimal for transumbilical placement. This self-retention system is perfectly attached to the aponeurosis and does not need for anchorage sutures. This platform permits the introduction of both rigid instruments and newly-developed instruments with different degrees of rotation and deflection that incorporate an attractive double-rotation allowing high precision and versatility of movement, recovery of triangulation and avoidance of instrument clashing (2).
The use of a 3.5-mm accessory trocar for radical prostatectomy, through which minilaparoscopy instruments are inserted is an optimal aid. This 3.5-mm access not only facilitates the most complex steps of surgery, such as urethro-vesical anastomosis, but also serves to extract the drain and avoid contamination of the umbilical wound leaving no scar. For radical cystectomy the 3.5-mm accessory access is substituted by a 10-mm port placed in the right iliac fossa (Figure 1). This second port is ideal to insert the suction-irrigation system in the first steps of cystectomy, and it is fundamental to perform the anastomosis for a neobladder using a straight needle-holder or to convert the port opening in the stoma for an ileal loop (16,17). Not less important is the fact that the reusable nature of most of the devices involved poses a great advantage in economical terms (18).
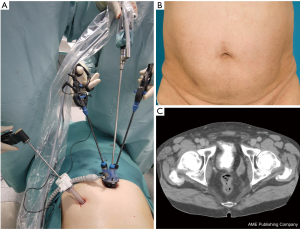
In our experience the use of minilaparoscopy accessory ports (3 to 3.5 mm) is an ideal complement to LESS, facilitates angulation and suturing with minimum cosmetic impact (15). This assistance has been postulated as a bridge to facilitate the skills needed to change conventional laparoscopy to LESS. Following this concept we were pioneer to describe the feasibility of nerve-sparing radical prostatectomy using the umbilical approach through KeyPort® system and 3.5-mm accessory port (2). Also other complex pelvic surgeries, such as partial cystectomy and ureteral reimplantation can be performed using this hybrid LESS approach (19,20). Finally we were again pioneer to describe a 2-port laparoscopic technique for radical cystectomy with a multichannel umbilical port and a 10-mm trocar on right iliac fossa (3,16,17). Our results were similar to those achieved through multiport conventional laparoscopy and patients reported better outcomes with the umbilical approach (17,20).
Some authors prefer a homemade disposable multichannel port made from two stretchable rings or a cone and a surgical glove with trocars and valves attached to its fingers through which straight elements are used (21,22) or even inserting several ports through a single aponeurotic incision in the form of a single-incision triangulated umbilical surgery (23). Pure LESS radical cystectomy without any accessory port has been performed, either using specific flexible steerable laparoscope and flexible monopolar scissors or straight instruments through a multichannel homemade device at a reasonable time, but always performing cutaneous ureterostomy or ileal conduit, thus revealing the actual technical limitations to perform continent urinary diversion through a single-port exclusively. We therefore prefer to use the two-port technique we described as we consider LESS radical cystectomy with orthotopic neobladder is the least invasive form of possibly the most invasive urologic surgery. This 2-port laparoscopic radical cystectomy has been standardized (24). The appropriateness of lymph node dissection is crucial, not only to correctly evaluate the need of adjunct therapy but also for prognosis itself. Of course continence and potency are also important issues in these patients; however, the high mortality rate of the disease leaves cosmetics, patient recovery, and analgesic needs to a second or third stage of concern.
There is no doubt that surgical fight against bladder and prostate cancer needs to assure continence and potency. Abdominal wall integrity and cosmesis are admirable goals, but are far from being important when facing such a dreadful disease as muscle-invasive bladder cancer. Also, the multiple treatment alternatives to fight localized prostate cancer force surgical technique for radical prostatectomy be refined and totally exigent. In other words, reduced likelihood of evisceration, wound infection or wound dehiscence is not enough to promote laparoendoscopic surgery. Oncological and functional results should be equivalent or superior to promote umbilical surgery over laparoscopy or robotics. Evidently achievement of better indemnity of the abdominal wall and excellent cosmesis is not enough. Multiport laparoscopy has been compared to open surgery for muscle-invasive bladder cancer (25) but no data has been reported regarding oncologic results of patients undergoing umbilical radical prostatectomy or umbilical radical cystectomy compared to the conventional laparoscopic counterparts. Retrospectively analyzed operative data reveal this surgery is within the range of security that should be expected for a center of high standard of care. Also the proportion of patients with complications according to Clavien-Dindo classification appears similar to laparoscopic radical cystectomy and laparoscopic robot-assisted cystectomy (18).
Su et al. have recently reported a very innovative solution to facilitate umbilical laparoendoscopic single-site for complex urologic surgical procedures, such as radical prostatectomy and radical cystectomy (26). They promote the use of a transurethral self-developed port, made from an outer seath of a 25-6F plasmakinetic ACMI (American Cystoscope Makers, Inc.) resectoscope, inserted through the urethra to facilitate resection of the prostate using the harmonic scalpel and toe ase performance of urethro-vesical anastomosis. This new transurethrally-assisted umbilical single multi-channel port surgery has been used in a series of 114 consecutive patients with admirable results. The concept strictly adheres to be considered pure natural orifice transluminal endoscopic surgery (NOTES) as both umbilicus and urethra are natural openings.
However, several major drawbacks must be criticized in their experience. In the first place a nerve-sparing approach has never been even intended and potency results are not taken into account. This fact is absolutely critical, especially if a transumbilical approach is expected to be competitive with robotic prostatectomy. On the other hand urinary continence recovery reported by these authors is surprisingly high, thus revealing another important limitation that is the absence of patient reported outcomes to properly evaluate continence recovery. A third important restraint of this experience is the fact that cutaneous ureterostomy, and not ureteroileostomy, has been the only non-continent urinary diversion used. Unfortunately this form of diversion is absolutely outdated and should not regularly be used in patients with muscle-invasive bladder cancer undergoing cystectomy. The fourth criticism to be raised to this experience is that the median number of nodes removed at the time of cystectomy is insufficient to achieve a high-quality pelvic lymph node dissection, what is of primary importance in these patients (27). Last but not least another impediment resides in the fact that no recurrence-free data is nowadays available to endorse this transurethral-assisted umbilical surgery as an elective approach. Apart from these severe limitations, Su et al. give a fresh breath to the unevolving issue of umbilical LESS for complex male pelvic surgeries and the authors should be congratulated for their effort and ingenious proposal.
There is no doubt that in a close future new platforms will be developed that further close the gap between reality and dreams to make non-incision surgery easier and more reproducible. Popularization of many present and future adjuncts such as auto-hitch sutures, organ retrieval systems, wound closing devices, hemostatic agents, adhesives and sealants is also crucial in the field. Improved quality of vision, together with higher precision and reliability of instruments will also be a reality soon. Instrument developers and investigators are in the direction to make surgery more satisfactory both for patients and doctor. We believe the performance of radical pelvic surgery (prostatectomy and cystectomy) through the natural scar of the navel is not far from becoming a reality. More precise articulating instruments and optical aids will be developed to facilitate the difficult reconstructive steps of the surgery. In the meantime intelligent steps such as the use of an accessory minilaparoscopy port or the use of an accessory transurethral port described by Su et al. (26), or any other facilitators still to be developed, could favour umbilical access and make performance of complex oncologic pelvic procedures less time-consuming, more accurate, more efficient and also more secure.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kaouk JH, Autorino R, Kim FJ, et al. Laparoendoscopic-single-site surgery in urology: worldwide multi-institutional analysis of 1076 cases. Eur Urol 2011;60:998-1005. [Crossref] [PubMed]
- Cáceres F, Cabrera PM, García-Tello A, et al. Safety study of umbilical single-port laparoscopic radical prostatectomy with a new DuoRotate system. Eur Urol 2012;62:1143-9. [Crossref] [PubMed]
- Angulo JC, Cáceres F, Arance I, et al. Cistectomía radical laparoscópica con neovejiga ileal ortotópica a través de puerto único umbilical. Actas Urol Esp 2012;36:554-61. [Crossref] [PubMed]
- White MA, Haber GP, Autorino R, et al. Robotic laparoendoscopic single-site radical prostatectomy: technique and early outcomes. Eur Urol 2010;58:544-50. [Crossref] [PubMed]
- Kaouk JH, Goel RK, White MA, et al. Laparoendoscopic single-site radical cystectomy and pelvic lymph node dissection: initial experience and 2-year follow-up. Urology 2010;76:857-61. [Crossref] [PubMed]
- Humphrey JE, Canes D. Transumbilical laparoendoscopic single site surgery in urology. Int J Urol 2012;19:416-28. [Crossref] [PubMed]
- García-Mediero JM, Cabrera PM, Cáceres F, et al. Current state of single-port transumbilical surgery in urology: Challenges and applications. Actas Urol Esp 2013;37:106-13. [Crossref] [PubMed]
- Wheeless CR Jr. Outpatient laparoscope sterilization under local anesthesia. Obstet Gynecol 1972;39:767-70. [PubMed]
- Pelosi MA, Pelosi MA 3rd. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med 1991;88:721-6. [PubMed]
- Navarra G, Pozza E, Occhionorelli S, et al. One-wound laparoscopic cholecystectomy. Br J Surg 1997;84:695. [Crossref] [PubMed]
- D’Alessio A, Piro E, Tadini B, et al. One-trocar transumbilical laparoscopic-assisted appendectomy in children: our experience. Eur J Pediatr Surg 2002;12:24-7. [Crossref] [PubMed]
- Raman JD, Vénzala K, Bagrodia A, et al. Laboratory and clinical development of single keyhole umbilical nephrectomy. Urology 2007;70:1039-42. [Crossref] [PubMed]
- Ramirez D, Maurice MJ, Kaouk JH. Robotic single-port surgery: paving the way for the future. Urology 2016;95:5-10. [Crossref] [PubMed]
- Nelson RJ, Chavali JSS, Yerram N, et al. Current status of robotic single-port surgery. Urol Ann 2017;9:217-22. [Crossref] [PubMed]
- Cáceres F, Cabrera PM, Mateo E, et al. Onset of a training program for single-port laparoscopic urology. Actas Urol Esp 2012;36:418-24. [Crossref] [PubMed]
- Angulo JC, Cáceres F, Cabrera PM, et al. Two-port laparoscopic radical cystectomy with reusable umbilical system: a feasibility study. Urology 2014;84:1088-93. [Crossref] [PubMed]
- Angulo JC, García-Tello A, Mateo E, et al. Two-port approach compared to standard laparoscopic radical cystectomy. J Endourol 2015;29:1030-7. [Crossref] [PubMed]
- García-Tello A, Cabrera PM, Cáceres F, et al. Umbilical laparoendoscopic urological surgery with a novel reusable device. Scand J Urol 2014;48:301-8. [Crossref] [PubMed]
- Redondo C, Pérez S, Gimbernat H, et al. Umbilical laparoendoscopic partial cystectomy. Actas Urol Esp 2015;39:451-5. [Crossref] [PubMed]
- Angulo JC, Pérez S, García-Tello A, et al. Two-port laparoscopic reconstructive surgery of the urinary tract with reusable umbilical system (Hybrid Less): A Proof of Concept Study. Urol Int 2016;97:179-85. [Crossref] [PubMed]
- Lin T, Huang J, Han J, et al. Hybrid laparoscopic endoscopic single-site surgery for radical cystoprostatectomy and orthotopic ileal neobladder: an initial experience of 12 cases. J Endourol 2011;25:57-63. [Crossref] [PubMed]
- Ma LL, Bi H, Hou XF, et al. Laparoendoscopic single-site radical cystectomy and urinary diversión: initial experience in China using a homemade single-port device. J Endourol 2012;26:355-9. [Crossref] [PubMed]
- Horstmann M, Kugler M, Anastasiadis AG, et al. Laparoscopic radical cystectomy: initial experience using the single-incision triangulated umbilical surgery (SITUS) technique. World J Urol 2012;30:619-24. [Crossref] [PubMed]
- Angulo JC, Cáceres F, Cabreara PM. LESS radical cystectomy. In: Kaouk JH, Stein RJ, Haber GP, editors. Atlas of Laparoscopic and Robotic Single Site Surgery. New York: Springer, 2016, Chapter 15, pp 151-68.
- Esquinas C, Alonso JM, Mateo E, et al. Prospective study comparing laparoscopic and open radical cystectomy: Surgical and oncological results. Actas Urol Esp 2017. [Epub ahead of print]. [PubMed]
- Su J, Zhu Q, Yuan L, et al. Transumbilical laparoendoscopic single-site radical prostatectomy and cystectomy with the aid of a transurethral port: a feasibility study. BJU Int 2017. [Epub ahead of print]. [Crossref] [PubMed]
- Núñez-Mora C, García Mediero JM, Cabrera-Castillo PM, et al. Feasibility of lymphadenectomy in laparoscopic radical cystectomy. Urology 2010;76:759-63. [Crossref] [PubMed]


