The extra-tunical grafting procedure for Peyronie’s disease hourglass and indent deformities
Introduction
Peyronie’s disease (PD) is a characterized by localized fibrosis of the penile tunica albuginea (TA), the fibrous connective tissue covering of the corpora cavernosa of the penis (1). PD is known to have a significant impact on patients’ quality of life, psychological fitness, and emotional wellbeing (2,3). Patients with PD often suffer from depression, embarrassment, and performance anxiety due to concerns about physical appearance, leading to loss of sexual confidence and sexual dysfunction. The prevalence of the PD is estimated to be 3–10% in the general population and up to 20% in patients with concomitant diabetes mellitus and erectile dysfunction (ED) (4). The prevalence of PD at young age (<40 years) has been reported to be between 1.5% and 10.5%, but a recent study revealed that 17% of men presenting with PD were ≤40 years of age (5). All of these figures, however, are thought to be under-reported for numerous reasons including patient embarrassment and limited screening.
The clinical course of PD is commonly divided into acute and chronic phases. The acute, or active, phase lasts between 6–12 months is characterized by pain, evolving plaque, inflammation, and evolving penile deformity. In 12–18 months pain typically resolves and curvature or deformity stabilizes, marking the chronic, or stable, phase of the disease (1). While the etiology of PD is not fully understood, it is thought to be a genetic connective tissue disorder exacerbated by repetitive microtrauma causing ischemia followed by abnormal wound healing (6). This leads to the development of inelastic, fibrous plaque in the TA. These plaques prevent penile expansion during erection, resulting in deformities such as curvature, hourglass (HG) deformity, indentation, shortening, and loss of girth. Dorsal penile curvature is the most commonly reported curvature, followed by lateral, then ventral (7). Indent, or notching, deformities are less commonly encountered. HG deformity is one of the most complex deformities, defined as circumferential narrowing, or waisting, of the TA (8).
Because of the dynamic nature of penis and the complex psychosocial factors involved with penile deformity and ED, PD is a challenging disease to treat. Treatment success is dependent not only on the objective physical improvement but also on the patient’s perception of the surgical result, the factor that most profoundly impacts patient satisfaction with treatment. Treating patients with indent and HG is particularly challenging. Plaque incision and grafting in these patients often requires dissection of the neurovascular bundle (NVB) and necessitates an incision into the TA, which may lead to a significant risk of hypoesthesia (9) and ED secondary to intracavernous fibrosis (10) and loss of veno-occlusive function at the area of grafting (11). In one series, despite high short term post-operative satisfaction (12), patient dissatisfaction rate at a minimum of 5-year follow-up after PD grafting surgery was over 65% with the major reasons for dissatisfaction being penile length loss and development of de novo ED (13). Understandably, it is probable that length loss in these patients was related to the pathophysiology of PD and not exclusively a post-operative complication, but patient perception remains the most important outcome in this patient population. To minimize the surgical risks as much as possible and to maximize patient satisfaction, it is advantageous to preserve the fundamental structure of the penis with minimal disruption of the NVB and the TA.
The extra-tunical grafting (ETG) procedure is a new surgical approach to penile indent and HG which avoids both incision into the TA and disruption of the NVB to virtually eliminate the risks of post-operative impotence and sensation loss. The ETG procedure reinforces the TA of the penis with a cadaveric fascia graft, much like an engineer “retrofits” an unstable house to protect it during an earthquake. The goal of the present study is to introduce this novel surgical intervention for PD patients and to evaluate the post-operative outcomes of erectile function, penile sensation, and patient satisfaction after ETG.
Methods
An IRB-approved, retrospective chart review of ETG patients was performed to collect data including pre-operative deformity, operation performed, and post-operative patient-reported perception of deformity, erectile function, penile sensation, and overall satisfaction with the ETG operation. The indications for surgery were difficulty with sexual intercourse due to deformity and/or poor cosmesis of the penis. Pre-operatively all patients had erections adequate for intercourse with or without medications. The patients were followed post-operatively for an average of 21 months (range, 6–44 months).
Penile deformity was evaluated in clinic after injection with a vasoactive agent to produce rigid erection. All assessments, documentation, and surgical interventions were performed by the same urologist. Informed consent was obtained from the patients for publication of images. Prior to surgical intervention, all eligible patients were offered injection with collagenase clostridium histolyticum (CCH) (14) to correct penile curvature. If the patient reported continued cosmetic or functional bother from the HG or indent deformity and if erection was strong enough for intercourse with or without medications, the patient was offered the ETG procedure to correct the deformity. If the erection was not adequate for intercourse, the patient was offered penile prosthesis placement.
All ETG patients including those with penile curvature who opted for penile plication at the same surgical setting were included in this retrospective chart review. In some cases, patients had both indent and/or HG plus curvature but opted not to have the curvature corrected, choosing instead for either no curvature treatment or CCH treatment at a future date. Plaque incision/grafting and plaque excision/grafting techniques were presented to the patients as surgical options, but these procedures are not routinely offered at our institution due to risks of impotence and sensation loss (15).
The ETG procedure is performed in the operative suite with the patient supine on the operating room table. Depending on the patient and anesthesia provider’s preferences, either sedation plus local anesthesia or general anesthesia may be utilized for the operation. For most patients, ETG or ETG plus penile plication can be accomplished with minimum alveolar concentration (MAC) and local anesthesia. A rigid erection is induced using vasoactive agent injection, and the patient’s skin is prepared in the usual sterile fashion (Figure 1). A local anesthetic is injected into the planned incision site and a penile ring block is performed at the base of the penis. The planned incision site is marked with a surgical marking pen.
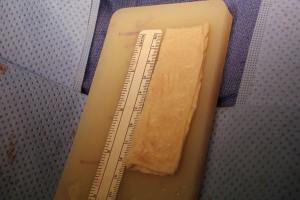
After instillation of local anesthetic, a longitudinal penile incision is made sharply with a 15-blade knife over the area of concern. Dissection continues through dartos fascia towards Buck’s fascia (Figure 2). The anatomy and length of the deformity is assessed and measured. If there is a curvature, the curvature is corrected with the 16-dot plication procedure (16) prior to addressing the indent or HG. A Tutoplast Suspend® graft (6 cm × 8 cm), which is chemically-processed, gamma-irradiated, dehydrated fascia lata, is then soaked in antibiotic solution for 5–10 minutes and tailored to fit the deformity (Figure 3). The goal of the procedure is to fill and fortify TA defects to produce a straight contour from penile base to distal penile shaft and to provide structural reinforcement for the narrowed region to prevent hinging during intercourse.
The graft is sized slightly thicker than the normal erect penile girth to allow for eventual partial resorption of the graft material. If the patient has an HG deformity, the NVB is not dissected from the TA. Rather, an omega-shaped graft is wrapped around the penis and secured to the ventral corpora with multiple interrupted 3-0 polydioxanone sutures placed adjacent to the corpus spongiosum on both sides (Figure 4). The corpus spongiosum is excluded from the graft. If the patient has indentation, the graft is placed in the location of the indent without the need for circumferential dissection. The graft material may need to be tailored or multiply layered to completely fill the deformity. It may be necessary to double, triple, or quadruple the thickness of the graft in order to appropriately correct the deformity and multiple grafts of different thicknesses may be needed for multiple deformities. In some cases, the graft may need to be layered on one side but not the other to properly correct an HG deformity.
The wound is irrigated repeatedly during the ETG procedure, and contact with the patient’s skin during the operation is minimized to reduce infection risk. The shaft skin is returned to anatomic position to assess the final surgical outcome after placement of the graft (Figure 5). An erection should be induced if pharmacologic erection has softened to ensure that the graft material is not trapping the penis or limiting erectile length or girth. Finally, the skin incision is closed in layers using interrupted 4-0 polyglactin sutures for the deepest layers and interrupted 5-0 polyglactin suture for superficial fascia. For the longitudinal skin incision, 5-0 polyglactin interrupted vertical mattress sutures are used for skin closure to avoid foreshortening of the shaft skin. The wound is dressed with surgical skin sealant, sterile gauze, and a loosely applied self-adherent elastic compressive dressing.
The ETG procedure is performed on an outpatient basis and typically takes approximately 1 hour to accomplish. Follow-up is recommended at serial intervals to ensure proper wound healing and ultimate patient outcome. During each post-operative visit, post-surgical factors assessed included degree of residual deformity, erectile function, penile sensation, and patient satisfaction level.



Results
From October 2013 to June 2017, 36 patients had the ETG procedure performed for indent and/or HG. Results with a minimum of 6 months of follow-up could be extracted for 18 of the patients. One was excluded as he required concurrent excision of a large calcified tunical plaque, which necessitated incision into the TA. Four patients had ETG only, and 13 had ETG with concurrent penile plication. Patients were seen in follow-up at various intervals with the range of follow-up between 6 and 44 months (average 21 months).
All patients reported satisfactory resolution of the HG or indent, with post-operative stabilization at the location of deformity during sexual intercourse. No patients reported a change in erectile function subsequent to the operation. Two patients (11.8%) reported slight reduction in penile sensation. Both of these patients had previously been circumcised, and one had multiple prior penile degloving surgeries for a history of significant penile trauma. No post-operative evidence of tissue rejection or infection was noted in any patient. Ten of the patients reported being “very satisfied” and six reported being “satisfied” with the procedure. One was neutral. None reported being “dissatisfied”. All patients reported that they would recommend the procedure to a friend, and all would repeat the same surgery if presented with the options again.
Discussion
As compared to previously employed, more invasive surgical techniques such as plaque incision or excision and grafting, the ETG procedure reduces anesthesia, operative, and recovery times and virtually eliminates the surgical risks of impotence, and hypoesthesia. In addition, no complications were encountered post-operatively with regards to surgical site infection or graft rejection. The current series of patients demonstrates that this straightforward surgical approach to complex penile HG and indent deformities also delivers high levels of patient satisfaction, with 16/17 being satisfied or very satisfied with the procedure (94.1%).
Strengths of this review are that the same surgeon performed all assessments, documentation, and operations, and that average post-operative follow-up was 21 months, suggesting that the ETG is a durable procedure. Weaknesses of this review are its retrospective nature and small number of patients. In addition, concomitant plication surgery in some cases may have skewed results. Lack of a consistently administered, validated questionnaire for patient assessment is an additional limitation. We also consider the lack of measurements of penile girth pre- and post-operatively as a weakness of this study, but our intent was to measure patient subjective, not objective, outcomes.
The ETG operation was developed originally for indent and HG deformities to reinforce, or thicken, the narrowed portion of the penile shaft to prevent buckling or hinging during sexual intercourse. Over time the operation has been modified to treat other penile pathologies including congenital weakness of the TA, corporeal herniation through the TA after CCH injection, and thinned TA after tunica-sparing excision of ossified Peyronie’s plaque (17). All of these pathologies are associated with significant negative consequences to erectile function due to the natural history of such a condition. Many of the traditional surgeries offered for treatment carry additional significant risk. With the ETG procedure, the surgeon may reassure the patient of minimal negative impact on erectile function.
As previously stated, our preferred graft material is gamma-irradiated cadaveric fascia lata. Although use of autologous materials, such as vein, dermis, or fascia, may cause less inflammation, the primary disadvantage is the need for an additional surgical site with the attendant risks of pain and infection along with increased operative time for harvesting and prolonged recovery time. Using an off-the-shelf allograft minimizes the morbidity of the procedure by avoiding the need to harvest an autograft and thus minimizing anesthesia time, eliminating the second incision, and speeding the recovery for the patient. Chemically treated, gamma irradiated acellular cadaveric fascia is thin, easy to handle, and easily flattens against the irregular surface profiles of the diseased TA. Tutoplast Suspend® has excellent tensile strength and multidirectional elasticity. These attributes are essential for the dynamic processes of penile erection, sexual intercourse, and detumescence (18).
Finally, it is worth noting that in the flaccid state the location of the graft will be more prominent, or thicker, than the remainder of the penile shaft. This is most apparent in the flaccid state in the early post-operative period. In the rigid state, the graft is minimally apparent even immediately after surgery. It is important to discuss this cosmetic change with the patient during pre-operative counseling to avoid post-operative patient discontent. The patient should be counseled that the graft acts as a tissue scaffold to allow for tissue ingrowth, which then provides biomechanical support for the hinging region of the penis. The girth difference becomes less evident over time as the graft material is partially resorbed during the normal healing process (10). By 6 months post-operatively, the graft is minimally apparent in both the flaccid (Figure 6) and rigid states.
Conclusions
The ETG procedure is a novel approach to penile indent and HG deformities with excellent patient satisfaction rates and very low associated risks of ED and penile sensation change. This operation augments the surgical armamentarium of reconstructive urologists and maximizes outcomes for PD patients with complex penile deformities.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the UCSF, Mount Zion Panel (#16-19430) and written informed consent was obtained from all patients.
References
- Nehra A, Alterowitz R, Culkin DJ, et al. Peyronie's Disease: AUA Guideline. J Urol 2015;194:745-53. [Crossref] [PubMed]
- Paulis G, Romano G, Paulis A. Prevalence, psychological impact, and risk factors of erectile dysfunction in patients with Peyronie's disease: a retrospective analysis of 309 cases. Res Rep Urol 2016;8:95-103. [Crossref] [PubMed]
- Terrier JE, Nelson CJ. Psychological aspects of Peyronie's disease. Transl Androl Urol 2016;5:290-5. [Crossref] [PubMed]
- Arafa M, Eid H, El-Badry A, et al. The prevalence of Peyronie's disease in diabetic patients with erectile dysfunction. Int J Impot Res 2007;19:213-7. [Crossref] [PubMed]
- Paulis G, Cavallini G, Barletta D, et al. Clinical and epidemiological characteristics of young patients with Peyronie's disease: a retrospective study. Res Rep Urol 2015;7:107-11. [Crossref] [PubMed]
- Lue TF. Peyronie's disease: an anatomically-based hypothesis and beyond. Int J Impot Res 2002;14:411-3. [Crossref] [PubMed]
- Hellstrom WJ, Bivalacqua TJ. Peyronie's disease: etiology, medical, and surgical therapy. J Androl 2000;21:347-54. [PubMed]
- Cakan M, Akman T, Oktar T, et al. The clinical characteristics of Peyronie's patients with notching deformity. J Sex Med 2007;4:1174-8. [Crossref] [PubMed]
- Hatzichristodoulou G, Osmonov D, Kubler H, et al. Contemporary Review of Grafting Techniques for the Surgical Treatment of Peyronie's Disease. Sex Med Rev 2017;5:544-52. [Crossref] [PubMed]
- Leungwattanakij S, Bivalacqua TJ, Caulfield JJ, et al. Evaluation of cadaveric pericardium in the rat for the surgical treatment of Peyronie's disease. Urology 2000;56:1075-80. [Crossref] [PubMed]
- Leungwattanakij S, Bivalacqua TJ, Reddy S, et al. Long-term follow-up on use of pericardial graft in the surgical management of Peyronie's disease. Int J Impot Res 2001;13:183-6. [Crossref] [PubMed]
- Kovac JR, Brock GB. Surgical outcomes and patient satisfaction after dermal, pericardial, and small intestinal submucosal grafting for Peyronie's disease. J Sex Med 2007;4:1500-8. [Crossref] [PubMed]
- Chung E, Clendinning E, Lessard L, et al. Five-year follow-up of Peyronie's graft surgery: outcomes and patient satisfaction. J Sex Med 2011;8:594-600. [Crossref] [PubMed]
- Gelbard M, Goldstein I, Hellstrom WJ, et al. Clinical efficacy, safety and tolerability of collagenase clostridium histolyticum for the treatment of peyronie disease in 2 large double-blind, randomized, placebo controlled phase 3 studies. J Urol 2013;190:199-207. [Crossref] [PubMed]
- Carson CC, Levine LA. Outcomes of surgical treatment of Peyronie's disease. BJU Int 2014;113:704-13. [Crossref] [PubMed]
- Brant WO, Bella AJ, Lue TF. 16-Dot procedure for penile curvature. J Sex Med 2007;4:277-80. [Crossref] [PubMed]
- Eisenberg ML, Smith JF, Shindel AW, et al. Tunica-sparing ossified Peyronie's plaque excision. BJU Int 2011;107:622-5. [Crossref] [PubMed]
- Hellstrom WJ, Reddy S. Application of pericardial graft in the surgical management of Peyronie's disease. J Urol 2000;163:1445-7. [Crossref] [PubMed]




