Postgraduate course in minimally invasive urological surgery
Introduction
The number of urologic laparoscopic procedures has increased since the first laparoscopic radical nephrectomy was described (1,2). Minimally invasive surgery is usually the method of choice for the management of most urological diseases (3-5). However, the development of minimally invasive surgery has created an educational challenge for surgeons who have never experienced such techniques during training (6-8). In addition, most laparoscopic procedures have a long learning curve, as the skills required for laparoscopy are different of those for open surgery, such as the counter-intuitive movements of the instruments and an indirect view of the surgical site (9,10).
The acquisition of skills in laparoscopy is associated with a learning curve that traditionally has been acquired during residency training and specialization in short- and long-term postgraduate courses (6,10,11). Some courses last from hours to a few days, while others are held over months or years; the latter are usually less available. There are many typical ways to acquire laparoscopic skills, such as theoretical classes, practice in traditional and virtual simulators, and surgeries in animal models (12-14).
The postgraduate course in minimally invasive urological surgery of our institution has been completed for five years. The program has already certified 50 students; however, it has never been evaluated or validated. The aim of this study is to evaluate the impact of the postgraduate course on the daily practice of these certified urologists.
Methods
The postgraduate course is composed of 10 modules, one per month, from March to December. Each module lasts for 36 hours and is divided in three consecutive days. Total postgraduate time is 360 hours, including 80 hours for research project development. Each 36-hour module is divided in 12 hours of theoretical classes, 12 hours of training in virtual simulators and in live animal models, 6 hours observing live surgeries and 6 hours for the development of a scientific research project. A specific topic is addressed according to complexity in each month, as follows: adrenalectomy, nephrectomy (total, radical and partial), pyeloplasty, stone surgeries, ureteral re-implants, pediatric urology, urogynecological procedures, benign prostate hyperplasia surgeries, radical prostatectomy and robotic radical prostatectomy. Each student performs approximately 50 laparoscopic procedures as the first surgeon and approximately 50 as the first assistant at the end of the postgraduate course.
Laparoscopic experts present theoretical classes and discuss videos of minimally invasive surgical techniques in each of the modules. Practical training is performed in an experimental surgical center that has ten fully equipped laparoscopic sets. Animals used for live surgery are minipig BR pigs, which are anesthetized and supervised by veterinarians, in accordance with the rules of the ethics committee for animal use. The postgraduate students are divided in groups of two per pig and perform procedures supervised by urologists with experience in laparoscopy.
The students observe live surgeries, also as part of the training, in order to follow every detail regarding perioperative care for each technique. All students have to develop and present, at the end of the course, an original manuscript, a literature review, or an experimental study according to the rules of the educational program.
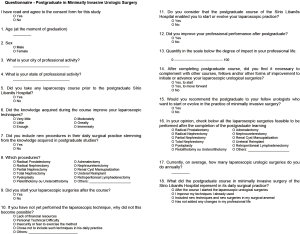
To evaluate the impact of training on daily practice of the certified surgeons, a questionnaire containing 18 questions was developed using the REDCap (Research Electronic Data Capture) digital platform (15). REDCap is a worldwide digital platform for the construction and management of online surveys and databases, specifically geared to support the capture of data for research projects (15). The questionnaire (Figure 1) was prepared by several professionals, such as biostatisticians, urologists and behavioral science specialists, covering specific issues: demographic data, impact of the postgraduate course on daily surgical activity, number of current laparoscopic procedures, experience before and after the course, type and complexity of the surgeries performed, the capacity to perform laparoscopy alone, and initiation and evolution of minimally invasive techniques. The questionnaire, approved by the Ethics Committee, was emailed to all former students. Participation in the study did not grant any advantage or disadvantage over the final course result.
Results
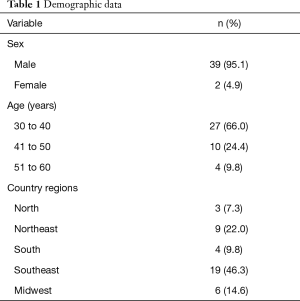
Fifty students were certified from 2010 through 2014. Forty-one of 50 (82%) students completed the questionnaire and were included in the analysis. One (2%) former student refused to participate, one (2%) student was permanently incapacitated after a brain stroke, and 7 (14%) students were not located, despite active searching. Of the 41 participants included in the survey, all filled out the consent form. Demographic data are shown in Table 1. Mean age was 39.5 years (range, 30–60 years) and only two students (4.9%) were female. Urologists from most Brazilian states were represented in the study.
Full table
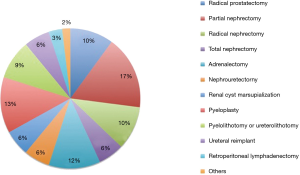
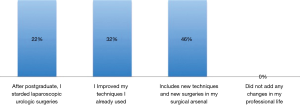
Thirty-two (78%) students had previously completed some type of laparoscopy course. Thirty (73.2%) students had already previous experience in laparoscopy, and 11 (26.8%) students had never performed any laparoscopic intervention. All students with no laparoscopic experience started performing laparoscopic urologic procedures after completing the course. In addition, 39 (92.3%) of the former students answered that they improved their surgical techniques, and 80% included new techniques or new procedures in their surgical practice. Figure 2 shows the new laparoscopic surgeries incorporated in the students’ practice. Median annual number of procedures per student was 15 and ranged from 2 to 100.
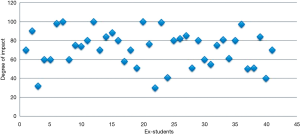
Using a visual scale bar ranging from 0 (none) to 100 (maximum), the students evaluated the degree of impact of the course on their professional activity, as shown in Figure 3. The median score was 75. The students mentioned a significant impact and influence of the course in their daily practice, including or improving laparoscopic techniques, as shown in Figure 4.
At the end of the course, 18 former students were able to perform most laparoscopic procedures but had no expertise to complete a laparoscopic radical prostatectomy. After completing the course, all students felt no necessity for fellowship programs or other forms of improvement in order to initiate or advance their laparoscopic surgeries, except for laparoscopic and robotic radical prostatectomy. All former students would recommend the course for urologists who wish to initiate or improve their minimally invasive techniques in urological laparoscopy.
Discussion
The results of this study show that the postgraduate course not only allows urologists to start laparoscopic activities but also to improve surgical techniques. All students are performing laparoscopic surgeries after the postgraduate course, and 80% of them are performing new procedures.
Brinkman et al. reported that regular training or a dedicated postgraduate course can improve the urologist’s comfort level in being willing to perform laparoscopy (16). In agreement with Brinkman et al., we also found that our students were able to improve their laparoscopic skills. Mulla et al. compared different training methods in basic laparoscopic skills and observed good efficacy of traditional and virtual simulators (17). Tjiam et al. examined the usefulness of the skills program in urological laparoscopy (PLUS), which contains five stations in training boxes and is based on the American FLS (Fundamentals of Laparoscopic Surgery) program. The authors concluded that the course is an important tool for step-by-step primary training, covering different aspects of basic laparoscopic skills (9). All PLUS stations, such as peg transfer, cutting a circle, single knot tying, clip and cut and needle guidance are included in our program training.
The postgraduate course of our institution includes all the methodologies reported by Mulla and Tjiam (9,17) and added to other teaching methods, such as lectures, article discussions, surgeries in animal models and observing live surgeries. The later ultimately will grant the students better knowledge regarding patient positioning and padding, team positioning, trocar placement and eventual difficulties in such step, immediate pre- and postoperative care and other details important to the accomplishment of each procedure that otherwise could not be learned.
Torricelli et al. analyzed the laparoscopic training program of urology residents from the University of São Paulo (18). There was a combination of virtual and manual simulators and a 10-week period in which swine models were available for training in such a program. Residents became more familiar with the procedures, the average duration of the procedures decreased and fewer surgical complications were observed at the end of the program. There ultimately were faster and safer procedures. In comparison, our course involves similar training techniques, but with a different methodology and a longer training period. In our annual course, extirpative surgeries were addressed in the initial two modules, followed by six modules of reconstructive procedures and the last two modules focused on the most challenging surgeries (laparoscopic and robotic prostatectomy).
Throughout the year, students enhance each technique through repetitive training, in accordance with the study of Gettman et al. (19). This repetitive training allows a controlled environment where all complications or possible errors can be identified and where the surgeon can plan how to avoid and manage complications. Each student performed 50 procedures as the first surgeon and 50 as the first assistant. In an ideal scenario, an experienced surgeon would do a demonstrative surgery in each of the modules. However, it is forbidden to use an animal model for such purposes due to institutional ethical concerns.
We recognize some limitations of our program. One of the main complaints of the students was the inability to safely perform a laparoscopic radical prostatectomy at the end of the course. In addition, our program does not certify students for robotic surgery. However, laparoscopic prostatectomies and robotic techniques were not the aim of the postgraduate course, as the first requires advanced laparoscopic expertise and demands a large learning curve, and the second requires specific training and certification. The study has also some limitations. Research questionnaires may generate sampling and interpretation biases, and therefore may be a limiting factor of the analysis. However, we were able to reduce such biases as the students answered the questionnaire after certification and as they had time, privacy, and freedom.
Finally, this study has even more importance in a decade where safety of residency training among patients is being questioned. Our next objective is the validation of the postgraduate course with automatic systems that are being developed and could improve the quality of data collection and analysis.
Conclusions
The annual postgraduate course is a reasonable way of acquiring urological laparoscopic skills. The course has proven to be efficient, impacting urologists’ practice in a significant manner.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The questionnaire, approved by the Ethics Committee (ID/number of ethical approval: HSL 2015-26/1.039.297), was emailed to all former students.
References
- Shalhav AL, Dabagia MD, Wagner TT, et al. Training postgraduate urologists in laparoscopic surgery: the current challenge. J Urol 2002;167:2135-7. [Crossref] [PubMed]
- Lee JY, Mucksavage P, Sundaram CP, et al. Best practices for robotic surgery training and credentialing. J Urol 2011;185:1191-7. [Crossref] [PubMed]
- Laguna MP, Schreuders LC, Rassweiler JJ, et al. Development of laparoscopic surgery and training facilities in Europe: results of a survey of the European Society of Uro-Technology (ESUT). Eur Urol 2005;47:346-51. [Crossref] [PubMed]
- Corica FA, Boker JR, Chou DS, et al. Short-term impact of a laparoscopic "mini-residency" experience on postgraduate urologists' practice patterns. J Am Coll Surg 2006;203:692-8. [Crossref] [PubMed]
- Gamboa AJ, Santos RT, Sargent ER, et al. Long-term impact of a robot assisted laparoscopic prostatectomy mini fellowship training program on postgraduate urological practice patterns. J Urol 2009;181:778-82. [Crossref] [PubMed]
- Kolla SB, Gamboa AJ, Li R, et al. Impact of a laparoscopic renal surgery mini-fellowship program on postgraduate urologist practice patterns at 3-year followup. J Urol 2010;184:2089-93. [Crossref] [PubMed]
- Miyajima A, Hasegawa M, Takeda T, et al. How do young residents practice laparoscopic surgical skills? Urology 2010;76:352-6. [Crossref] [PubMed]
- De Win G, Van Bruwaene S, Aggarwal R, et al. Laparoscopy training in surgical education: the utility of incorporating a structured preclinical laparoscopy course into the traditional apprenticeship method. J Surg Educ 2013;70:596-605. [Crossref] [PubMed]
- Tjiam IM, Persoon MC, Hendrikx AJ, et al. Program for laparoscopic urologic skills: a newly developed and validated educational program. Urology 2012;79:815-20. [Crossref] [PubMed]
- Vlaovic PD, Sargent ER, Boker JR, et al. Immediate impact of an intensive one-week laparoscopy training program on laparoscopic skills among postgraduate urologists. JSLS 2008;12:1-8. [PubMed]
- Shepherd W, Arora KS, Abboudi H, et al. A review of the available urology skills training curricula and their validation. J Surg Educ 2014;71:289-96. [Crossref] [PubMed]
- Ather MH, Siddiqui T. Urology training in the developing world: The trainers' perspective. Arab J Urol 2014;12:64-7. [Crossref] [PubMed]
- Beyer L, Troyer JD, Mancini J, et al. Impact of laparoscopy simulator training on the technical skills of future surgeons in the operating room: a prospective study. Am J Surg 2011;202:265-72. [Crossref] [PubMed]
- Sroka G, Feldman LS, Vassiliou MC, et al. Fundamentals of laparoscopic surgery simulator training to proficiency improves laparoscopic performance in the operating room-a randomized controlled trial. Am J Surg 2010;199:115-20. [Crossref] [PubMed]
- Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377-81. [Crossref] [PubMed]
- Brinkman WM, Tjiam IM, Schout BM, et al. Results of the European Basic Laparoscopic Urological Skills examination. Eur Urol 2014;65:490-6. [Crossref] [PubMed]
- Mulla M, Sharma D, Moghul M, et al. Learning basic laparoscopic skills: a randomized controlled study comparing box trainer, virtual reality simulator, and mental training. J Surg Educ 2012;69:190-5. [Crossref] [PubMed]
- Torricelli FC, Guglielmetti G, Duarte RJ, et al. Laparoscopic skill laboratory in urological surgery: tools and methods for resident training. Int Braz J Urol 2011;37:108-11; discussion 112. [Crossref] [PubMed]
- Gettman MT, Pereira CW, Lipsky K, et al. Use of high fidelity operating room simulation to assess and teach communication, teamwork and laparoscopic skills: initial experience. J Urol 2009;181:1289-96. [Crossref] [PubMed]