Randomized study of percutaneous ureteroscopic plasma column electrode decortication and laparoscopic decortication in managing simple renal cyst
Introduction
Simple renal cyst (SRC) is a common cystic renal disease in urology and the prevalence is 20–50% in general population (1). The incidence is increased with age. The possibility of an increase in diameter of an SRC was 7.1 times greater in patients aged over 50 years than in those aged less than 50 years (2). The smaller renal cyst does not require treatment because it is asymptomatic and without renal function damage (3). A small proportion of SRC sometimes has symptoms, such as hematuria, pain, obstruction and hypertension. Treatment was required for patients with these symptoms.
The management of SRC includes open surgery (3), laparoscopy (4), aspiration and sclerotherapy (5), ureteral endoscope incision drainage (6,7) etc. Laparoscopic decortication is a minimally invasive and effective therapy for SRC and is quite popular in recent years (8). Ureteroscopic plasma column electrode (PCE) is used after percutaneous nephrolithotomy to decrease the surgical morbidity by electrocauterization of bleeding points (9,10). However, it was not reported to treat the SRC. We hypothesize that the advantages of this technique will also translate to the decortication of SRC. In this study, we aimed to evaluate the safety, efficacy and our initial clinical experience for this treatment.
Methods
Patients
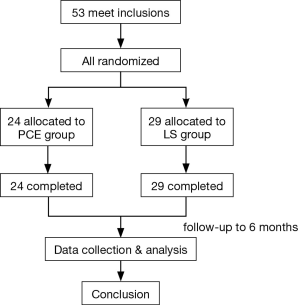
Between March 2016 and June 2017, 53 patients with symptomatic SRC were studied. The location of SRC was detected by enhanced CT scan for all patients. Bosniak grades were grade I. All the cysts were cortical. Patients were randomized divided into two groups. The PCE group comprised 24 patients. The laparoscope group comprised 29 patients. The flow diagram is shown in Figure 1. The clinical data, including sex, age, clinical presentation, operation time, blood loss, postoperative indwelling drainage tube time, intra-urethral indwelling catheter retention time and postoperative hospital stay were recorded. All patients have signed informed consent. The method of percutaneous ureteroscopic PCE renal cyst decortication and the study protocol have been approved by the ethics committee of our hospital.
Procedure
Percutaneous PCE group: the patients were in prone position after general anesthesia. Under ultrasound, cyst puncture was performed and the needle was placed. After removal of the stylet, a guidewire was passed through the needle. The skin over the puncture site was then incised. The wound was dilated and a F16 or F18 Amplatz sheath. Along the channel, an ureteroscope with PCE was introduced into Amplatz sheath. The tip of the ureteroscope and the sheath were used to separate the surrounding tissue under continuous flow saline. The cyst boundary was completely resected with a PCE. The SiMai plasma surgery system was used during the operation with parameters: electrical cutting power (60 W), coagulation power (30–40 W), flow rate (0.2 L/min) and water pressure (100 mmHg). F14 nephrostomy tube was placed after surgery.
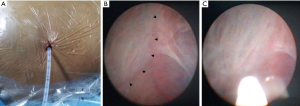
Laparoscopic group: the patients were placed in the lateral decubitus position under general anesthesia. A 2 cm skin incision was made in the posterior axillary line midway between the last rib and iliac crest. The SRC was dissected and the cyst contents were aspirated. The roof of the cyst was then excised with endoscissors and submitted together with several ‘bites’ from the floor of the cyst for a histopathological examination. The cyst edge was sealed by ultrasonic scalpel and the fat was placed in the cyst. Finally, a tube drain was placed and the wounds were closed (Figure 2).
All the patients were assessed with ultrasonography or CT examinations at 1 and 6 months after operation.
Statistical analysis
The measurement data were expressed by means (range). Statistical significance between two groups was analyzed by the student t-test and chi-square test with SPSS 20 software (IBM Corp., Somers, NY, USA). P<0.05 was considered statistically significant.
Results
The PCE group had 24 patients (10 males and 14 females). The characteristics of all 53 patients in both groups are listed in Table 1. The mean age in this group was 62.4±9.74 years (range, 48–80 years). The mean size was 6.3±1.1 cm (range, 4.6–7.9 cm). The laparoscope group had 29 patients (12 males and 17 females). The mean age was 54.6±9.6 years (range, 30–70 years). The mean size was 6.3±1.36 cm (range, 5.0–12.0 cm). The diameters of SRC were over 5 cm in 53 cases. The patients suffered with discomfort in the back and lumbar. The diameter of RSC in 1 case was 4.6 cm, but glomerular filtration rate (GFR) showed slight impairment of renal function.

Full table
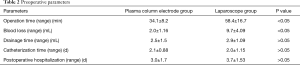
All patients did not have intraoperative complications such as hemopneumothorax, adjacent organ injury and infection. The operative parameters of all 53 patients in both groups are listed in Table 2. In the PCE group: the mean operation time was 34.1±8.2 min (range, 17–48 min). The mean blood loss was 2.0±1.16 mL (range, 1–5 mL). The mean postoperative indwelling drainage tube time was 2.5±1.5 d (range, 1–7 d). The mean intra-urethral indwelling catheter time was 2.1±0.88 d (range, 1–4 d). The mean postoperative hospital stay was 3.0±1.7d d (range, 1–7 d). One patient suffered from rupture of the collecting system during the operation, and was treated by indwelling D-J stent. After 1 month, the wound was recovered and the D-J stent was removed. In the laparoscope group: the mean operation time was 58.4±16.7 min (range, 28–93 min). The mean blood loss was 9.7±4.09 mL (range, 5–20 mL). The mean postoperative indwelling drainage tube time was 2.9±1.09 d (range, 1–5 d). The mean intra-urethral indwelling catheter time was 2.0±1.15 d (range, 1–4 d). The mean postoperative hospital stay was 3.7±1.53 d (range, 1–8 d). The overall postoperative pathology was renal cysts. The follow up for each patient was 6 months. No cysts recurrence was found by ultrasound or CT scan. Statistical analysis showed that the operation time was shorter in PCE group and intraoperative blood loss was less in electrode group (P<0.05); there was no significant difference between in postoperative hospital stay, the time of postoperative drainage tube indwelling and the time of postoperative catheterization in both groups.
Full table
Discussion
Renal cysts are quite common, and the incidence was increased with age. Clinically, renal cysts were classified with Bosniak grade (11), in our study, all the cysts were Bosniak grade I, which means the cysts were simple, thin walled, with no septation, calcification and no enhancement after contrast CT scan. For complex renal cyst, laparoscopic decortication was recommended. The vast majority of RSC remain asymptomatic, but sometimes cysts become large enough to cause mechanical effects, such as pain, hematuria, pain, obstruction and hypertension.
Only symptomatic renal cysts are needed to be treated. Several treatments have been used, such as open surgery (8), laparoscopy and percutaneous aspiration and sclerotherapy (12) etc. Laparoscopic renal cyst decortication is widely used as an effective minimally invasive treatment for renal cysts (13). Long-term follow-up (52 months) has confirmed that laparoscopic cyst decortication is an effective, minimally invasive and safe treatment for SRCs (10). Compared with open surgery, it has the advantages of less damage and quicker recovery. It was the reason we chose laparoscopy as a treatment for one group. Other treatment option includes endoscopic management. It has been reported that percutaneous ablation of renal cysts using a bipolar resection system was successfully performed (14).
Percutaneous electrode PCE was used to treat the bleeding points at the end of percutaneous renal surgery, which decreased the blood transfusion rate without causing an increase in morbidity. This procedure was safe and effective (10). In another study, this technique was applied to creating the nephrostomy tract for PCNL, which was safe, leads to less blood loss than the other techniques (15). In our study, we used this technique to the decortication of SRC. It turned out to be a safe, minimally invasive and effective therapy to treat SRCs.
The basic principle of PCE is: cutting: under the action of high frequency current, there is a high current density on the contact surface between the electrode and the perfusion fluid, which exceeds the vaporization threshold of the perfusion fluid, makes the surrounding liquid vaporize and generates plasma layer, and the high frequency electric power is concentrated in the plasma layer, and the plasma layer is maintained. When the plasma layer is close to the target tissue, the plasma layer is used to cut the tissue. Coagulation: the plasma layer does not stimulated during coagulation, and the tissue is solidified by the thermal effect of current.
Compared with laparoscopic decortication, this treatment required only 0.6 cm incision (Figure 2A) to create a single channel for all the procedures, which will reduced the operative hemorrhage and operative time (P<0.05). For the other operative parameters, including the mean postoperative indwelling drainage tube time, the mean catheter retention time, the mean postoperative hospital stay time, there were no significant differences. During 6 months follow up, there was no recurrence for renal cyst. In our opinion, this technique is safe and effective, which provides new method to treat the SRC.
There were some surgical skills for this surgery: (I) the first step is to establish the channel for operation, which is similar to the procedure of PCNL; (II) during operation, the most important part is to distinguish the cyst wall and the parenchyma of the kidney. Figure 2B shows the boundary of the cyst wall. It looks pale for the cyst part and cherry for the parenchyma; (III) it was safe and efficacy to remove the cyst wall 0.5 cm from the edge of the parenchyma; (IV) Pay special attention to the pressure of the flow and the operative time to avoid pleural and peritoneal effusion. In our experiences, the pressure of irrigation fluid (100 mmHg) and the flow rate (0.2 L/min) were good for the patients. No peritoneal or pleural effusion was found by ultrasound one day after the surgery; (V) coagulate the edge of the cyst wall properly to avoid intraoperative and postoperative hemorrhage. The PCE has two functions: electric resection and coagulation. If there was a blood vessel on the cyst wall, coagulate the end of the vessel first before resecting the cyst wall. In previous study, holmium laser with a 200 µm fiber was used to incise and drain the renal cyst (16). In our experiences, it is efficient to use the PCE to stop bleeding spots; (VI) check every part of the cyst and resect the wall of the cyst completely. Do not pull out the specimen violently; otherwise it would damage the collecting system of the kidney.
In the electrode plasma column group, one patient suffered from perforation in the collecting system, which was due to the large movement of the respiratory. The diameter of the perforation was 0.2 cm. A double J stent was placed at the end of the surgery. One month later, intravenous pyelography (IVP) was performed to check the leakage of the perforation. The wound was recovered and the double J stent was removed.
One limitation of the study is the sample size. Since this study was the first usage of the electrode plasma column to treat the RSC, there is no preexisting data. In the future, we would include more patients for this treatment.
Conclusions
Percutaneous ureteroscopic PCE decortication is a safe, minimally invasive and effective therapy to treat SRCs, with equal efficacy and advantages in shortening the operation time and reducing the amount of intraoperative bleeding compared with laparoscopic decortication.
Acknowledgements
Funding: This work was supported by grant from National Natural Science Foundation of China (No. 81500532).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: All patients have signed informed consent. The method of percutaneous ureteroscopic plasma column electrode renal cyst decortication and the study protocol have been approved by the ethics committee of our hospital.
References
- Bas O, Nalbant I, Can Sener N, et al. Management of renal cysts. JSLS 2015;19:e2014 00097.
- Park H, Kim CS. Natural 10-year history of simple renal cysts. Korean J Urol 2015;56:351-6. [Crossref] [PubMed]
- Skolarikos A, Laguna MP, de la Rosette JJ. Conservative and radiological management of simple renal cysts: a comprehensive review. BJU Int 2012;110:170-8. [Crossref] [PubMed]
- Terada N, Ichioka K, Matsuta Y, et al. The natural history of simple renal cysts. J Urol 2002;167:21-3. [Crossref] [PubMed]
- Chang CC, Kuo JY, Chan WL, et al. Prevalence and clinical characteristics of simple renal cyst. J Chin Med Assoc 2007;70:486-91. [Crossref] [PubMed]
- Yoder BM, Wolf JS Jr. Long-term outcome of laparoscopic decortication of peripheral and peripelvic renal and adrenal cysts. J Urol 2004;171:583-7. [Crossref] [PubMed]
- Basiri A, Hosseini SR, Tousi VN, et al. Ureteroscopic management of symptomatic, simple parapelvic renal cyst. J Endourol 2010;24:537-40. [Crossref] [PubMed]
- Amar AD, Das S. Surgical management of benign renal cysts causing obstruction of renal pelvis. Urology 1984;24:429-33. [Crossref] [PubMed]
- Okeke AA, Mitchelmore AE, Keeley FX, et al. A comparison of aspiration and sclerotherapy with laparoscopic de-roofing in the management of symptomatic simple renal cysts. BJU Int 2003;92:610-3. [Crossref] [PubMed]
- Jou YC, Cheng MC, Sheen JH, et al. Electrocauterization of bleeding points for percutaneous nephrolithotomy. Urology 2004;64:443-6; discussion 446-7. [Crossref] [PubMed]
- Bosniak MA. The current radiological approach to renal cysts. Radiology 1986;158:1-10. [Crossref] [PubMed]
- Agarwal M, Agrawal MS, Mittal R, et al. A randomized study of aspiration and sclerotherapy versus laparoscopic deroofing in management of symptomatic simple renal cysts. J Endourol 2012;26:561-5. [Crossref] [PubMed]
- Lifson BJ, Teichman JM, Hulbert JC. Role and long-term results of laparoscopic decortication in solitary cystic and autosomal dominant polycystic kidney disease. J Urol 1998;159:702-5; discussion 5-6. [Crossref] [PubMed]
- Korets R, Mues AC, Gupta M. Minimally invasive percutaneous ablation of parapelvic renal cysts and caliceal diverticula using bipolar energy. J Endourol 2011;25:769-73. [Crossref] [PubMed]
- Chiang PH, Su HH. Randomized and prospective trial comparing tract creation using plasma vaporization with balloon dilatation in percutaneous nephrolithotomy. BJU Int 2013;112:89-93. [Crossref] [PubMed]
- Mao X, Xu G, Wu H, et al. Ureteroscopic management of asymptomatic and symptomatic simple parapelvic renal cysts. BMC Urol 2015;15:48. [Crossref] [PubMed]