Optimizing patient selection for focal therapy—mapping and ablating the index lesion
Optimizing patient selection for focal therapy (FT)—localizing the index lesion
As experience with FT for clinically localized prostate cancer (PCa) increases, well-defined clinical guidelines for patient selection continue to evolve (1-7).
Early consensus recommendations relied upon clinical parameters such as prostate specific antigen (PSA), clinical stage, and transrectal ultrasound (TRUS) biopsy, seeking to identify the 20–40% of men with unifocal disease as the ideal candidates for hemiablation (4,5). Hindered by the diagnostic inaccuracy of TRUS biopsy to localize the site(s) of significant disease, these consensus groups recommended restricting patient selection to low grade, low volume disease and encouraged transperineal mapping biopsy (TPMBx) in order to most accurately identify unilateral disease (4,8).
The use of active surveillance (AS) for low grade, low volume PCa has steadily gained acceptance and is supported by guidelines adopted by the American Urologic Association (AUA), Society of Urologic Oncologists (SUO) and National Cancer Care Network (NCCN) (9). Realizing that low risk disease generally does not mandate immediate intervention, consensus is emerging that the optimal candidates for FT include men with intermediate-risk, unifocal Gleason score 7 cancer or larger volume Gleason 6 PCa (6,7).
Ultimately, the tantamount selection criteria for successful focal ablation must be based on accurate identification of the location and volume of all significant disease within the prostate. The combination of multi-parametric prostate magnetic resonance imaging (mpMRI) with targeted biopsy prostate sampling offers a significant advance in diagnostic evaluation that has provided the key foundation in disease localization necessary for selecting cases for FT.
Multiparametric MRI of the prostate—critical non-invasive disease evaluation
mpMRI ushered in a sea change in prostate diagnostics by offering an imaging method capable of localizing significant PCa (10,11). The utility of prostate MRI has evolved from staging to dynamic, multi-parametric sequences that provide detailed anatomic evaluation combined with assessments of cellular density and vascularity which facilitates localization of significant PCa. Ultimately, the ability of mpMRI to accurately identify and characterize PCa depends upon disease size, location, and aggressiveness (10).
Equally as important as disease localization, mpMRI excludes the presence of high grade disease when the imaging appears normal, with estimates for the negative predictive value (NPV) of a “normal” MRI to detect high grade disease ranging from 69% to 93% (3). Recent Level 1b evidence from Ahmed et al. reported a NPV of mpMRI of 89% for any Gleason 4+3 or a cancer core length of greater than 5 mm TPMBx in the PROMIS trial (11). Lending to the external validity of this finding, it is important to note that these results were obtained with mpMRI using 1.5T magnet at 11 centers in the UK, many of which were not high-volume prostate MRI centers.
Given the improvement in localization of significant disease that mpMRI offers over the existing TRUS systematic sampling paradigm, patient selection for focal ablation requires a pretreatment evaluation with mpMRI (12). Preferably this imaging takes place at a center with sufficient clinical experience in prostate MRI, although debate continues regarding the ideal equipment necessary for optimal imaging. Prostate imaging findings should be analyzed and reported according to Prostate Imaging-Reporting and Data System (PI-RADS) version 2 (13).
Additional ablation information from mpMRI
Beyond localizing disease, mpMRI provides further information regarding anatomical features that influence both patient selection for treatment as well as selection of type of focal ablation energy.
Tumor proximity to critical anatomical structures such as the urethra, external sphincter, bladder neck and prostate capsule influences the planning of a successful ablation that balances oncological control and complications. Furthermore, recognition of treatment impact on these structures aids in pre-treatment counseling for patients considering ablation treatment. For instance, ablation of tumors near the urethra potentially increases risk of urethral toxicity such as tissue sloughing and stricture formation (14).
Imaging with mpMRI also provides information regarding disease features unavailable on biopsy or other clinical evaluations including seminal vesical invasion, evidence of gross extracapsular extension, proximity of disease relative to the neurovascular bundle and urethra and local staging information regarding nodal status and bony features (15,16). These features ultimately may influence patient suitability for focal ablation from the perspective of oncologic efficacy and toxicity risk and extent of margins during treatment planning.
Imaging with mpMRI also provides accurate assessment of overall prostate volume, an anatomical feature that ultimately influences eligibility for focal ablation as certain technologies are limited by gland dimensions or disease location (16). Tumors that are located in anterior locations greater than 4 cm from the rectum are not effectively treated with energy sources such as high intensity focused ultrasound (HIFU) (17). In addition, cryoablation probes are restricted to a maximum length and effective treatment volume. Prostate dimensions or tumor volumes may extend beyond these physical limitations and risk decreased efficacy as well as increase risk for complications.
The index lesion—target of focal ablation
The “index lesion” hypothesis represents the critical oncologic challenge to the FT paradigm (18,19). Although the hypothesis of the index lesion remains controversial, the concept has been a proven approach in multiple organ preserving oncologic strategies such as those employed in breast and kidney cancer.
Multi-parametric MRI localizes the index tumor in 80–95% of cases, with accuracy improving with the size, Gleason score and location of the lesion (10,20-25). From the perspective of FT patient selection, these findings suggest that mpMRI reliably identifies the highest oncologic risk disease and thus allows for confirmation using targeted biopsy. Based upon the results of targeted biopsy, the presence and location of an index lesion can be determined, allowing for index lesion based treatment strategies. The most recent consensus statement on FT defines FT as treatment directed towards ablation of the index lesion (6). Embracing this concept assists in defining optimal candidates for focal ablation. Patients with unilateral, MR visible disease, confirmed to be of the highest grade/volume on targeted prostate biopsy represent the ideal candidate for focal ablation. However, patients with a dominant lesion, MR visible, of low to intermediate risk lesion on targeted biopsy, who may have contralateral low grade, small volume, MR invisible disease, represent ideal candidates for focal ablation using an index lesion approach.
Ensuring accurate ablation—defining and destroying the index tumor
Ultimately, focal PCa ablation presents a three-dimensional problem. A zone of tissue containing the tumor and a margin of healthy tissue must be included in a confluent treatment volume. Defining the necessary ablation zone to achieve optimal oncologic outcome remains a controversial yet critical challenge for focal ablation strategies. However, defining this ablation zone requires a clear understanding of the correlation between tumor volume on MRI and histologic tumor volume. Furthermore, understanding how each focal ablation technology achieves a confluent ablation zone is critical for FT selection.
Treatment margin
Optimizing the treatment margin in focal ablation is the core concept of FT. Excessive treatment margin risks toxicity by damaging critical structures and inadequate treatment margins risk rendering focal ablation as sham therapy. In addition, more extensive treatment margins may render future treatments, such as radical prostatectomy, more challenging (26). Estimation of margin and extent of disease is best obtained through careful pre-ablation TPMBx. However, this approach is burdensome to patients and the health system alike.
Ideally, mpMRI offers a non-invasive estimate of disease volume and margin. Current data supports a systematic underestimation of histologic tumor volume based on MRI tumor volume (10). The degree of this underestimation varies by study. Recent consensus panels recommend a minimum margin of ≥5 mm on planned ablation volume, although several studies suggest a margin of approximately 10 mm or more may be more appropriate (6,27,28). As understanding of the relationship between histologic tumor volume and tumor volume on MRI improves, focal margin will likely vary depending on tumor size, grade and location. As of now, conservative margins between 5 to 10 mm, including a margin beyond the prostate capsule when disease abuts the capsule, are recommended (29). This treatment margin must also consider anatomic boundaries such as the prostate capsule, external sphincter, urethra and neurovascular bundle (27). Treatment margins that ablate tissue beyond the prostate capsule risk damage to surrounding structures such as the neurovascular bundle and external urethral sphincter. Ablation of these critical structures hamper the side effect profile of focal ablation and thus provide an important limitation for patient selection.
Treatment beyond the ablation zone
A critical conceptual limitation of focal ablation is that PCa is multi-focal in about 75–80% of cases selected for radical prostatectomy (30). Complete ablation of the MRI index lesion may ultimately not eradicate all disease that meets definition for clinical significance, or “aggressive” disease. Kenigsberg et al. examined theoretical oncological control in men fulfilling criteria for unilateral focal ablation who underwent radical prostatectomy (31). In this evaluation, approximately 25% of men had Gleason 4 pattern disease outside of the ablation zone, of which 65% were on the contralateral side of the gland. Twenty percent of these tumor foci were dominant Gleason pattern 4% and 50% of these foci demonstrated a median cancer core length of less than 1 mm. Based upon these results, ultimately ablating only the index lesion a with a 10 mm treatment margin, or performing an ipsilateral hemiablation, leaves Gleason pattern 4 disease untreated in 23.7% and 18.6% respectively. This untreated disease would meet selection criteria for AS in many cohorts (9,32). The higher risk of disease progression in men with untreated Gleason pattern 4 mandates that men undergoing focal ablation require close surveillance, amounting to an AS of the untreated prostate.
Additional treatment volume considerations
The ablation zone volume needed to achieve confluent tissue destruction depends upon multiple factors. From the perspective of factors intrinsic to ablation technique, each ablation energy achieves tissue destruction in a defined volume. Capability to coalesce these treatment volumes into a confluent “kill” zone that includes and surrounds the target volume determines oncological disease control. For example, performing HIFU on anterior gland lesions, located at a significant distance from the HIFU transducer, risks incomplete ablation due to energy absorption in posterior tissue and incomplete energy deposition in the target volume. Cryoablation of lesions that cross the midline risk inadequate ablation secondary to heat sink effects from the urethral warming catheter and anatomical limitations regarding placement of the cryoprobes (i.e., inability to place probes in the midline due to risk of urethral penetration).
Additional factors important to confluent ablation zone include imaging co-registration error intrinsic in translation of MRI to TRUS (the imaging modality utilized for the majority of focal ablation technologies). Several studies have demonstrated that registration error between MRI and TRUS vary by size of the region of interest as well as registration technique, with elastic registration commonly improving this error (33,34). Treatment planning must also account for alterations in treatment anatomy secondary to treatment such as gland distortion from needle placement or energy absorption and patient movement during treatment (35).
Most mpMRI imaging is evaluated in two dimensions (2D). Most focal ablation modalities utilize 2D TRUS imaging, Prostate disease volume and margin are three-dimensional (3D) concepts. At the current time, lesions are cognitively estimated as geometric shapes in 2D imaging with linear margins of a given length applied around this shape to provide an arbitrary ablation zone margin (10). This rudimentary approach does not account for multiple variables such as variations in ablation energy volume, gland movement and gland distortion during treatment.
While existing MRI-US fusion platforms create 3D surface models to translate mpMRI to TRUS, similar platforms for focal ablation planning and execution are in early stages of development. Critical features that these imaging models must address include estimating 3D treatment volume with variable treatment margins, elastic registration processes to account for alteration of gland anatomy through the ablation process and tools to optimize margin near critical structures such as the urethra or neurovascular bundle. Ideally, such software would also provide objective measures to assess for ablation efficacy (e.g., microbubble contrast-enhanced US or Doppler assessment of disruption of vascularity in the treatment zone). Currently MR thermometry enables objective measurement of tissue temperature and has been employed for assessment of MR guided laser ablation and HIFU (36,37). These techniques remain limited to treatments applied in the MR gantry, thus limiting applicability for TRUS guided ablation techniques.
Acknowledging these critical 3D variables and pre-treatment planning based upon 3D tumor models represents an area of active development. Such disease modeling in a 3D model may offer improved methods for treatment selection as well as enhance treatment efficacy.
Disease follow-up
Optimal follow-up strategies for FT remain to be defined. Utilizing mpMRI offers potential for non-invasive evaluation of treatment success and post-treatment surveillance. The optimal follow-up imaging regimen also remains to be determined.
Post-treatment imaging approximately 2–3 weeks following focal ablation offers assessment of accuracy of ablation targeting. Although these early results do not predict treatment success, the ability of early follow-up MRI to assess gross targeting may be useful during the initial adoption of an ablative treatment. Surveillance mpMRI using contrast enhancement assesses for viable tissue within or around the treatment zone by assessing for enhancement on post-contrast T1 imaging (38). Post-ablation, DCE imaging appears to be more sensitive than DWI for detection of local recurrence (39). However, follow up imaging characteristics vary by the type of ablation energy utilized (38).
At this time, a standard post-ablation follow-up protocol has yet to be defined. However, mpMRI is recommended for both treatment planning as well as follow up evaluation. The indications for biopsy of the ablation zone also remain highly controversial. Ideally, a non-invasive post-treatment surveillance protocol would likely improve adherence and minimize patient burden.
Targeted biopsy—critical tool for patient selection
Currently, the exact specificity for detection of clinically significant disease with mpMRI remains to be fully determined (11). This fact precludes the ability to simply treat off imaging findings. Disease localization requires biopsy confirmation. Further studies are necessary to define the optimal biopsy strategy to evaluate the findings on mpMRI. However, the ideal biopsy approach should serve to address not only confirmation of disease presence, but also accurately assess the boundaries of disease.
Prostate biopsy with MRI-US fusion biopsy technique allows increased identification of high grade disease and reduced detection of low grade disease (40-42). Subsequently, this technique facilitates confirmation of the location of the index tumor. As MRI-US fusion biopsy provides limited information on disease mapping, future studies are needed to further characterize the utility of inclusion of additional mapping biopsies. Several recent studies report TRUS biopsy results from regions around focal ablations and suggest that targeted biopsy and systematic biopsy are needed to evaluate for patient eligibility for focal ablation (29,31). At this time, consensus statements recommend utilization of TPMBx for inclusion for patient selection in the absence of mpMRI-US fusion biopsy (6).
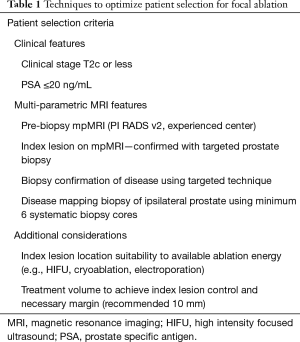
In summary, from the perspective of FT, mpMRI is essential as an imaging study to identify candidates for FT. Further confirmation with targeted biopsy and systematic biopsy remain necessary for disease confirmation and provide limited information on disease mapping (3). Consensus panel recommendations for FT patient selection criteria continue to evolve. However, recent panel recommendations emphasize the shift toward inclusion of intermediate risk disease and the role of mpMRI (Table 1) (7).
Full table
Conclusions
Strategies to optimize patient selection for FT remain in their early stages and are under ongoing evaluation. At this time, the disease states amenable to focal ablation are best identified using pre-treatment mpMRI following by targeted biopsy tissue confirmation. Identifying the myriad of additional factors necessary for achieving the central goal of focal ablation, namely the in-situ destruction of aggressive disease while preserving genitourinary function, rely heavily upon the accuracy and interpretation of imaging prior to and during ablation. Additional studies are needed to improve the understanding of these factors. The growing field of genomics will also likely provide a significant influence patient selection for focal ablation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ahmed HU, Akin O, Coleman JA, et al. Transatlantic Consensus Group on active surveillance and focal therapy for prostate cancer. BJU Int 2012;109:1636-47. [Crossref] [PubMed]
- Bostwick DG, Waters DJ, Farley ER, et al. Group consensus reports from the Consensus Conference on Focal Treatment of Prostatic Carcinoma, Celebration, Florida, February 24, 2006. Urology 2007;70:42-4. [Crossref] [PubMed]
- Muller BG, Futterer JJ, Gupta RT, et al. The role of magnetic resonance imaging (MRI) in focal therapy for prostate cancer: recommendations from a consensus panel. BJU Int 2014;113:218-27. [Crossref] [PubMed]
- Eggener SE, Scardino PT, Carroll PR, et al. Focal therapy for localized prostate cancer: a critical appraisal of rationale and modalities. J Urol 2007;178:2260-7. [Crossref] [PubMed]
- de la Rosette J, Ahmed H, Barentsz J, et al. Focal therapy in prostate cancer-report from a consensus panel. J Endourol 2010;24:775-80. [Crossref] [PubMed]
- Donaldson IA, Alonzi R, Barratt D, et al. Focal therapy: patients, interventions, and outcomes--a report from a consensus meeting. Eur Urol 2015;67:771-7. [Crossref] [PubMed]
- Jarow JP, Ahmed HU, Choyke PL, et al. Partial Gland Ablation for Prostate Cancer: Report of a Food and Drug Administration, American Urological Association, and Society of Urologic Oncology Public Workshop. Urology 2016;88:8-13. [Crossref] [PubMed]
- Barzell WE, Melamed MR. Appropriate patient selection in the focal treatment of prostate cancer: the role of transperineal 3-dimensional pathologic mapping of the prostate--a 4-year experience. Urology 2007;70:27-35. [Crossref] [PubMed]
- Bruinsma SM, Bangma CH, Carroll PR, et al. Active surveillance for prostate cancer: a narrative review of clinical guidelines. Nat Rev Urol 2016;13:151-67. [Crossref] [PubMed]
- Wysock JS, Lepor H. Multi-parametric MRI imaging of the prostate-implications for focal therapy. Transl Androl Urol 2017;6:453-63. [Crossref] [PubMed]
- Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 2017;389:815-22. [Crossref] [PubMed]
- Scheltema MJ, Tay KJ, Postema AW, et al. Utilization of multiparametric prostate magnetic resonance imaging in clinical practice and focal therapy: report from a Delphi consensus project. World J Urol 2017;35:695-701. [Crossref] [PubMed]
- Weinreb JC, Barentsz JO, Choyke PL, et al. PI-RADS Prostate Imaging - Reporting and Data System: 2015, Version 2. Eur Urol 2016;69:16-40. [Crossref] [PubMed]
- Mundy AR, Andrich DE. Posterior urethral complications of the treatment of prostate cancer. BJU Int 2012;110:304-25. [Crossref] [PubMed]
- de Rooij M, Hamoen EH, Witjes JA, et al. Accuracy of Magnetic Resonance Imaging for Local Staging of Prostate Cancer: A Diagnostic Meta-analysis. Eur Urol 2016;70:233-45. [Crossref] [PubMed]
- Delongchamps NB, Beuvon F, Eiss D, et al. Multiparametric MRI is helpful to predict tumor focality, stage, and size in patients diagnosed with unilateral low-risk prostate cancer. Prostate Cancer Prostatic Dis 2011;14:232-7. [Crossref] [PubMed]
- Cordeiro ER, Cathelineau X, Thuroff S, et al. High-intensity focused ultrasound (HIFU) for definitive treatment of prostate cancer. BJU Int 2012;110:1228-42. [Crossref] [PubMed]
- Perera M, Krishnananthan N, Lindner U, et al. An update on focal therapy for prostate cancer. Nat Rev Urol 2016;13:641-53. [Crossref] [PubMed]
- Tareen B, Sankin A, Godoy G, et al. Appropriate candidates for hemiablative focal therapy are infrequently encountered among men selected for radical prostatectomy in contemporary cohort. Urology 2009;73:351-4; discussion 4-5. [Crossref] [PubMed]
- Rosenkrantz AB, Hindman N, Lim RP, et al. Diffusion-weighted imaging of the prostate: Comparison of b1000 and b2000 image sets for index lesion detection. J Magn Reson Imaging 2013;38:694-700. [Crossref] [PubMed]
- Delongchamps NB, Lefèvre A, Bouazza N, et al. Detection of Significant Prostate Cancer with Magnetic Resonance Targeted Biopsies—Should Transrectal Ultrasound-Magnetic Resonance Imaging Fusion Guided Biopsies Alone be a Standard of Care? J Urol 2015;193:1198-204. [Crossref] [PubMed]
- Baco E, Ukimura O, Rud E, et al. Magnetic resonance imaging-transectal ultrasound image-fusion biopsies accurately characterize the index tumor: correlation with step-sectioned radical prostatectomy specimens in 135 patients. Eur Urol 2015;67:787-94. [Crossref] [PubMed]
- Radtke JP, Kuru TH, Boxler S, et al. Comparative analysis of transperineal template saturation prostate biopsy versus magnetic resonance imaging targeted biopsy with magnetic resonance imaging-ultrasound fusion guidance. J Urol 2015;193:87-94. [Crossref] [PubMed]
- Rud E, Klotz D, Rennesund K, et al. Detection of the index tumour and tumour volume in prostate cancer using T2-weighted and diffusion-weighted magnetic resonance imaging (MRI) alone. BJU Int 2014;114:E32-42. [Crossref] [PubMed]
- Le JD, Tan N, Shkolyar E, et al. Multifocality and prostate cancer detection by multiparametric magnetic resonance imaging: correlation with whole-mount histopathology. Eur Urol 2015;67:569-76. [Crossref] [PubMed]
- Peretsman S, Brooks J. Salvage robotic prostatectomy following whole gland high-intensity focused ultrasound with a Sonablate 500 device: technical feasibility and safety. J Robot Surg 2017;11:217-21. [Crossref] [PubMed]
- Le Nobin J, Rosenkrantz AB, Villers A, et al. Image Guided Focal Therapy for Magnetic Resonance Imaging Visible Prostate Cancer: Defining a 3-Dimensional Treatment Margin Based on Magnetic Resonance Imaging Histology Co-Registration Analysis. J Urol 2015;194:364-70. [Crossref] [PubMed]
- Priester A, Natarajan S, Khoshnoodi P, et al. Magnetic Resonance Imaging Underestimation of Prostate Cancer Geometry: Use of Patient Specific Molds to Correlate Images with Whole Mount Pathology. J Urol 2017;197:320-6. [Crossref] [PubMed]
- Nassiri N, Chang E, Lieu P, et al. Focal Therapy Eligibility Determined by Magnetic Resonance Imaging/Ultrasound Fusion Biopsy. J Urol 2018;199:453-8. [Crossref] [PubMed]
- Humphrey PA. Complete histologic serial sectioning of a prostate gland with adenocarcinoma. Am J Surg Pathol 1993;17:468-72. [Crossref] [PubMed]
- Kenigsberg AP, Llukani E, Deng FM, et al. The Use of Magnetic Resonance Imaging to Predict Oncological Control Among Candidates for Focal Ablation of Prostate Cancer. Urology 2018;112:121-5. [Crossref] [PubMed]
- Aghazadeh MA, Frankel J, Belanger M, et al. NCCN Favorable Intermediate Risk Prostate Cancer: Is Active Surveillance Appropriate? J Urol 2018;199:1196-201. [Crossref] [PubMed]
- Wegelin O, Henken KR, Somford DM, et al. An Ex Vivo Phantom Validation Study of an MRI-Transrectal Ultrasound Fusion Device for Targeted Prostate Biopsy. J Endourol 2016;30:685-91. [Crossref] [PubMed]
- Lai WS, Zarzour JG, Gordetsky JB, et al. Co-registration of MRI and ultrasound: accuracy of targeting based on radiology-pathology correlation. Transl Androl Urol 2017;6:406-12. [Crossref] [PubMed]
- Halstuch D, Baniel J, Lifshitz D, et al. Assessment of Needle Tip Deflection During Transrectal Guided Prostate Biopsy: Implications for Targeted Biopsies. J Endourol 2018;32:252-6. [Crossref] [PubMed]
- Napoli A, Anzidei M, De Nunzio C, et al. Real-time magnetic resonance-guided high-intensity focused ultrasound focal therapy for localised prostate cancer: preliminary experience. Eur Urol 2013;63:395-8. [Crossref] [PubMed]
- Bomers JGR, Cornel EB, Futterer JJ, et al. MRI-guided focal laser ablation for prostate cancer followed by radical prostatectomy: correlation of treatment effects with imaging. World J Urol 2017;35:703-11. [Crossref] [PubMed]
- Patel P, Mathew MS, Trilisky I, et al. Multiparametric MR Imaging of the Prostate after Treatment of Prostate Cancer. Radiographics 2018;38:437-49. [Crossref] [PubMed]
- Kim CK, Park BK, Lee HM, et al. MRI techniques for prediction of local tumor progression after high-intensity focused ultrasonic ablation of prostate cancer. AJR Am J Roentgenol 2008;190:1180-6. [Crossref] [PubMed]
- Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015;313:390-7. [Crossref] [PubMed]
- Meng X, Rosenkrantz AB, Mendhiratta N, et al. Relationship Between Prebiopsy Multiparametric Magnetic Resonance Imaging (MRI), Biopsy Indication, and MRI-ultrasound Fusion-targeted Prostate Biopsy Outcomes. Eur Urol 2016;69:512-7. [Crossref] [PubMed]
- Gordetsky JB, Thomas JV, Nix JW, et al. Higher Prostate Cancer Grade Groups Are Detected in Patients Undergoing Multiparametric MRI-targeted Biopsy Compared With Standard Biopsy. Am J Surg Pathol 2017;41:101-5. [Crossref] [PubMed]


