Detection of extraprostatic disease and seminal vesicle invasion in patients undergoing magnetic resonance imaging-targeted prostate biopsies
Introduction
Although rare, both extraprostatic extension (EPE) and seminal vesicle invasion (SVI) by prostate cancer (PCa) can be identified on prostate needle core biopsy. In one large retrospective study, EPE was found in only 0.6% of prostate needle core biopsy cases (1). The majority of these cases were associated with perineural invasion (PNI) on standard biopsy (SB) as well as high-risk disease on follow up radical prostatectomy. Multiparametric magnetic resonance imaging/ultrasound (MRI/US) fusion targeted biopsy (TB) has been shown to more accurately identify higher grade PCas, compared to the standard extended prostate biopsy SB (2-5). TB has also been reported to have superior detection of poor prognostic features, such as PNI (6,7). We evaluated the clinical, pathologic, and radiologic features associated with EPE and SVI on TB.
Methods
An institutional review board approved (NO. X140724007) retrospective review of patients who had undergone MRI/US fusion TB was performed on our surgical pathology database from 2014–2017. Patients who had biopsy pathologic findings of EPE and/or SVI were included. Image processing and targeting was performed using DynaCad and UroNav, respectively (Phillips/InVivo, Gainesville, FL, USA). PI-RADS v2 scoring was assigned via a multidisciplinary consensus conference with fellowship-trained radiologists and oncologic urologists specializing in prostate MRI, all with >5 years of experience with prostate MRI. Two fellowship trained oncologic urologists at the University of Alabama at Birmingham performed all MRI/US fusion prostate biopsies.
All prostate biopsies were reviewed by a single genitourinary surgical pathologist. In each case, the overall Gleason score for each SB and TB was based on the core with the highest Gleason score. Prostate cancer Grade Groups, adopted by the International Society of Urological Pathology (ISUP) and World Health Organization (WHO), were also assigned to biopsy cores (8). EPE on prostate needle core biopsy was defined as tumor cells present within the periprostatic adipose tissue. All seminal vesicle tissue was labeled as “seminal vesicle” by the urologist performing the procedure and further confirmed as seminal vesicle by histologic examination. SVI was defined as tumor invasion within the smooth muscle wall of the seminal vesicle. Clinical, pathologic, and radiologic features were evaluated.
Results
We identified 333/593 (56.2%) patients who had cancer detected on MRI/US fusion TB. Of these, 5/333 (1.5%) patients were diagnosed with EPE and/or SVI (Table 1). The average age and prostate-specific antigen (PSA) of this subset was 71 years [median: 72 years; interquartile range (IQR): 5.5] and 17 ng/mL (median: 8.88 ng/mL; IQR: 27.2), respectively. The average prostate volume was 40.3 cc (median: 31.17 cc; IQR: 34.1). Two patients had a prior negative SB for PCa, two patients had a prior positive biopsy for PCa and one patient was biopsy naïve. One patient had previously undergone radiation therapy for a PCa. All patients had a PIRADS score of 4 or 5. Four of five (80%) patients underwent both SB and concurrent TB, of which 3/4 (75%) patients had EPE identified only on TB and 1/4 (25%) patients had EPE identified only on SB. One of four (25%) patients also had concurrent SVI, identified only on TB. One patient underwent only TB for MRI suspicion of SVI, which was confirmed on TB. The average number of cores taken on TB was 4.2 (median: 4; IQR: 1.5). Prostate Grade Groups were as follows: 1/5 (20%) Grade Group 3, 2/5 (40%) Grade Group 4, and 2/5 (40%) Grade Group 5. Two of four (50%) patients had higher Grade Group PCa on TB compared to SB (Grade Group 2 to 5, 3 to 4). PNI was present in 4/5 (80%) patients on TB. Of the three patients with clinical follow-up, one completed radiation therapy and has remained disease free 3 years after his initial diagnosis. One patient is currently undergoing radiation and androgen deprivation therapy. The third patient, who had recurrent disease status post radiation therapy, underwent a salvage radical prostatectomy, with biochemical recurrence at 3 months follow-up.
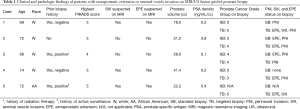
Full table
Discussion
Approximately 30,000 men in the USA die from PCa annually, making it the second-leading cause of cancer-related mortality (9). Currently the standard of care in the diagnosis of PCa is a 12-core extended-sextant prostate biopsy. This procedure consists of systematic sampling of the prostate gland from six predetermined sections of the prostate. A major pitfall of this technique is that the samples are essentially taken at random from pre-defined quadrants and the accurate detection of cancer can be somewhat limited. In contrast, multiparametric MRI is a novel diagnostic tool that specifically evaluates tissue density and vascularity, allowing for more accurate detection of lesions suspicious for PCa (10). Use of MRI in conjunction with transrectal ultrasound results in real time electronically superimposed images, allowing for the collection of tissue from the most suspicious lesional areas (2). Recent studies have suggested TB can detect more clinically significant PCas and aid in accurate detection of higher staged disease (11-13). Siddiqui and colleagues evaluated 1,003 men undergoing both MRI/US-targeted biopsy and SB and found that MRI/US fusion TB was not only associated with increased detection of high-risk PCa, but was also better able to predict final pathology on follow-up radical prostatectomy (2). Gordetsky et al. evaluated 191 patients who had undergone MRI/US fusion TB with concurrent 12-core SB, and showed that there was no difference in the cancer detection rate between TB and SB (41.4% and 49.2%, respectively, P=0.15). In addition, the degree of detection of ≥ Grade Group 3 tumors significantly favored TB over SB (7). These results hold important implications for patient management, as the use of MRI/US fusion TB is able to provide more accurate diagnoses of high-grade PCa with sampling of fewer cores (9,14).
Identification of EPE is an important component of staging in PCa patients, and is defined by the American Joint Committee on Cancer (AJCC) TNM staging system as pT3a in the presence of extension into the periprostatic fat and as pT3b in the case of SVI (1,15,16). Although the presence of EPE on SB is a rare occurrence, a significant number of patients who undergo radical prostatectomy for presumed localized disease are found to have EPE, implying that its presence is being consistently under detected on SB (15). Although the presence of EPE can sometimes be captured on MRI, it is only with moderate sensitivity and specificity (72% and 65%, respectively), which is insufficient for confirmation of its presence. The presence of EPE in radical prostatectomy specimens has been extensively studied and has a well-established association with disease progression and positive surgical margins (15). However, due to its rarity on biopsy, little is known about biopsy detected EPE as a potential independent predictor of aggressive PCa. In a study by Fleshner et al., 112/19,950 (0.6%) patients with PCa on SB had detection of EPE (1). Overall, we found EPE and/or SVI in 1.5% of patients with PCa who had undergone TB. In addition, of those who underwent both SB and concurrent TB, 75% had EPE identified only on TB. Although the numbers are too small for a definitive conclusion, the data suggests that TB may be detecting EPE at a higher frequency than SB alone.
The tracking of prostatic carcinoma along the perineural space is a known “path of least resistance” for cancer cells to extend beyond the prostate (15,17). Similar to the findings of Fleshner et al., we found that nearly all our patients (4/5, 80%) with EPE/SVI also had concurrent PNI. PNI is believed to not only be a mechanism for PCa extension, but is also considered a marker for more aggressive neoplastic biology (18). Fromont et al. found that cancer cells in areas of PNI exhibited increased proliferation, as well as increased EGFR and CD74 expression (19). Recent radical prostatectomy, brachytherapy, and external beam radiotherapy series have found PNI to be independently associated with increased risk of biochemical relapse (9). In one study, men with low-risk disease and PNI on prostate biopsy were shown to have a 4–5 times greater risk of harboring higher grade and/or higher volume disease than men without PNI on biopsy (15). DeLancey et al. reported on 3,226 patients who underwent radical prostatectomy, of which 20% had PNI on biopsy. Patients with PNI on biopsy were more likely to have EPE (35.9% vs. 12.8%), SVI (14.1% vs. 3.2%), positive surgical margins (26.5% vs. 16.4%), and positive lymph nodes (2.5% vs. 0.5%; all P<0.01) (20). Additionally, it has been found that men with PNI detected on biopsy tend to have more cores with cancer (9). PNI on prostate biopsy is also associated with a shorter time to disease progression on confirmatory biopsy, and failure of active surveillance (9). Although most studies involving PNI have been limited to biopsies obtained via standard techniques, a recent study showed greater detection of PNI by TB compared to SB (7). Another study showed the presence of PNI on TB to be associated with EPE on radical prostatectomy and early biochemical recurrence (6). Despite the association between PNI and high risk features there is still debate over its status as an independent risk factor for adverse pathologic features and worse survival outcomes after radical prostatectomy (18,21).
As might be expected, all five patients in our series with EPE/SVI identified on MRI/US fusion TB had associated preoperative high risk factors. The average PSA for our five patients was 17 ng/mL and 4/5 (80%) patients had Grade Groups 4 or 5 disease, which has a predicted 5-year biochemical risk-free survival of 48% and 26%, respectively (8,22,23). In addition, all patients had a PIRADS score of 4 or 5, indicating a high likelihood of clinically significant cancer (24). One of our patients underwent only TB due to MRI suspicion of SVI. In this case only four targeted cores were obtained and both EPE and SVI were diagnosed. These findings were confirmed on radical prostatectomy. This case illustrates the advantage of TB in diagnosing aggressive diseases while minimizing the number of cores and invasiveness of the biopsy procedure.
Limitations of this study include that it is retrospective in nature and presents data on a very limited number of patients. A multi-institutional study involving a larger cohort of patients who underwent both standard and TB would be ideal to assess the incidence of EPE and SVI detection using an MRI/US targeted technique.
Conclusions
Based on our small series, we hypothesize that MRI/US fusion TB outperforms SB in the identification of EPE and SVI. However, given the small sample size and the overall rarity of these pathologic findings on prostate biopsy, further validation is needed.
Acknowledgements
None.
Footnote
Conflicts of Interest: JW Nix and S Rais-Bahrami serve as consultants for Philips/InVivo Corp.
Ethical Statement: The study was approved by the institutional review board of the University of Alabama at Birmingham (NO. X140724007) with approval of waiver of informed consent.
References
- Fleshner K, Assel M, Benfante N, et al. Clinical Findings and Treatment Outcomes in Patients with Extraprostatic Extension Identified on Prostate Biopsy. J Urol 2016;196:703-8. [Crossref] [PubMed]
- Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015;313:390-7. [Crossref] [PubMed]
- Puech P, Rouvière O, Renard-Penna R, et al. Prostate cancer diagnosis: multiparametric MR-targeted biopsy with cognitive and transrectal US-MR fusion guidance versus systematic biopsy--prospective multicenter study. Radiology 2013;268:461-9. [Crossref] [PubMed]
- Borkowetz A, Platzek I, Toma M, et al. Comparison of systematic transrectal biopsy to transperineal magnetic resonance imaging/ultrasound-fusion biopsy for the diagnosis of prostate cancer. BJU Int 2015;116:873-9. [Crossref] [PubMed]
- Gordetsky JB, Thomas JV, Nix JW, et al. Higher Prostate Cancer Grade Groups Are Detected in Patients Undergoing Multiparametric MRI-targeted Biopsy Compared With Standard Biopsy. Am J Surg Pathol 2017;41:101-5. [Crossref] [PubMed]
- Truong M, Rais-Bahrami S, Nix JW, et al. Perineural invasion by prostate cancer on MR/US fusion targeted biopsy is associated with extraprostatic extension and early biochemical recurrence after radical prostatectomy. Hum Pathol 2017;66:206-11. [Crossref] [PubMed]
- Gordetsky JB, Nix JW, Rais-Bahrami S. Perineural Invasion in Prostate Cancer Is More Frequently Detected by Multiparametric MRI Targeted Biopsy Compared With Standard Biopsy. Am J Surg Pathol 2016;40:490-4. [Crossref] [PubMed]
- Epstein JI, Egevad L, Amin MB, et al. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of Grading Patterns and Proposal for a New Grading System. Am J Surg Pathol 2016;40:244-52. [PubMed]
- Cohn JA, Dangle PP, Wang CE, et al. The prognostic significance of perineural invasion and race in men considering active surveillance. BJU Int 2014;114:75-80. [Crossref] [PubMed]
- Ahmed HU, El-Shater Bosaily A, Brown LC, et al. Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. Lancet 2017;389:815-22. [Crossref] [PubMed]
- Lai WS, Gordetsky JB, Thomas JV, et al. Factors predicting prostate cancer upgrading on magnetic resonance imaging–targeted biopsy in an active surveillance population. Cancer 2017;123:1941-8. [Crossref] [PubMed]
- Raskolnikov D, George AK, Rais-Bahrami S, et al. The Role of Magnetic Resonance Image Guided Prostate Biopsy in Stratifying Men for Risk of Extracapsular Extension at Radical Prostatectomy. J Urol 2015;194:105-11. [Crossref] [PubMed]
- Raskolnikov D, George AK, Rais-Bahrami S, et al. Multiparametric magnetic resonance imaging and image-guided biopsy to detect seminal vesicle invasion by prostate cancer. J Endourol 2014;28:1283-9. [Crossref] [PubMed]
- Siddiqui MM, George AK, Rubin R, et al. Efficiency of Prostate Cancer Diagnosis by MR/Ultrasound Fusion-Guided Biopsy vs Standard Extended-Sextant Biopsy for MR-Visible Lesions. J Natl Cancer Inst 2016;108. [Crossref] [PubMed]
- Cozzi G, Rocco BM, Grasso A, et al. Perineural invasion as a predictor of extraprostatic extension of prostate cancer: a systematic review and meta-analysis. Scand J Urol 2013;47:443-8. [Crossref] [PubMed]
- Amin MB, Edge SB, Greene FL, et al. AJCC Cancer Staging Manual. Chicago: Springer International Publishing, 2016:1024.
- Hassan MO, Maksem J. The prostatic perineural space and its relation to tumor spread: an ultrastructural study. Am J Surg Pathol 1980;4:143-8. [Crossref] [PubMed]
- Feng FY, Qian Y, Stenmark MH, et al. Perineural invasion predicts increased recurrence, metastasis, and death from prostate cancer following treatment with dose-escalated radiation therapy. Int J Radiat Oncol Biol Phys 2011;81:e361-7. [Crossref] [PubMed]
- Fromont G, Godet J, Pires C, et al. Biological significance of perineural invasion (PNI) in prostate cancer. Prostate 2012;72:542-8. [Crossref] [PubMed]
- DeLancey JO, Wood DP Jr, He C, et al. Evidence of perineural invasion on prostate biopsy specimen and survival after radical prostatectomy. Urology 2013;81:354-7. [Crossref] [PubMed]
- Loeb S, Epstein JI, Humphreys EB, et al. Does perineural invasion on prostate biopsy predict adverse prostatectomy outcomes? BJU Int 2010;105:1510-3. [Crossref] [PubMed]
- Gordetsky J, Epstein J. Grading of prostatic adenocarcinoma: current state and prognostic implications. Diagn Pathol 2016;11:25. [Crossref] [PubMed]
- Epstein JI, Zelefsky MJ, Sjoberg DD, et al. A Contemporary Prostate Cancer Grading System: A Validated Alternative to the Gleason Score. Eur Urol 2016;69:428-35. [Crossref] [PubMed]
- Steiger P, Thoeny HC. Prostate MRI based on PI-RADS version 2: how we review and report. Cancer Imaging 2016;16:9. [Crossref] [PubMed]


