
Cytomegalovirus infection in kidney allografts: a review of literature
Introduction
Cytomegalovirus (CMV) infection is an important cause of morbidity and mortality and the most important viral pathogen in kidney transplant recipients. Kidney allograft CMV infection is a rare event, but it needs consideration as a differential diagnosis of any seropositive patient with graft dysfunction.
Methods
We performed a systematic literature review on English-language indexed journals from PubMed, Cochrane Library and Mendeley databases. The following terms were employed: cytomegalovirus nephritis, cytomegalovirus transplant and cytomegalovirus kidney. Exclusion criteria were: non-English language studies, not accessible to the University of São Paulo nor “Periódicos CAPES, institutional e-resources and irrelevant manuscripts (e.g., non-human, experimental reports) Eleven CMV nephritis case reports were reviewed. Data was compiled for the following variables: demographics, risk factors, clinical presentation, histopathological aspects, treatment and outcome.
Results
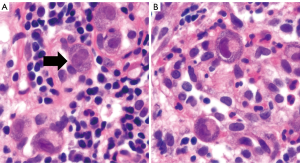
Twelve cases were reviewed and are summarized on Tables 1-4. The most affected kidney transplant group was the recipients (83%, 10/12). The age range varied between 16 and 80 years (Table 1). Nine patients received cadaveric kidneys (75%, 9/12) and three of the allografts originated from living donors (25%, 3/12). All kidney transplant recipients were negative for CMV (100%, 10/10) while all donors had positive viral serology (100%, 10/10). CMV infection was detected between 3 to 58 weeks post transplantation (Table 2). Four patients were asymptomatic (33%, 4/12). The main symptom reported was diarrhoea (33%, 4/12). Conventional bright-field microscopy histological evaluation (Table 3) was suffice to detect viral inclusions by hematoxylin and eosin (H&E) in eleven cases (92%, 11/12), through viral inclusion detection. In one case with normal histological description CMV was not detected on H&E stain, but immunohistochemical positivity confirmed the diagnosis. Five cases showed minimal histological changes besides viral cytopathic inclusions (42%,5/12). One case revealed crescents with glomerular necrosis (8%, 1/12). In terms of treatment and clinical outcomes (Table 4), nine patients used Ganciclovir (75%, 9/12), two received valganciclovir (16%, 2/12) and one used Foscarnet (8%, 1/12). Kidney function was posteriorly improved to normal in five patients (42%, 5/12), four had improvement of renal function, maintaining serum creatinine levels above baseline (33%, 4/12). Four patients had dismal outcomes (33%, 4/12) one developed transplant glomerulopathy one year after transplantation (8%, 1/12), one developed collapsing focal segmental glomerulosclerosis and acute cellular rejection (8%, 1/12), one patient developed transplant glomerulopathy one year after transplantation (8%, 1/12), and one patient developed end-stage renal disease with need for hemodialysis (1/12). No lethal outcomes were reported.
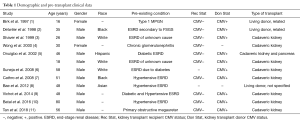
Full table
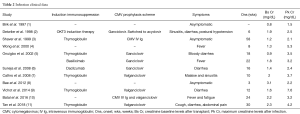
Full table
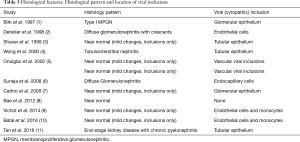
Full table
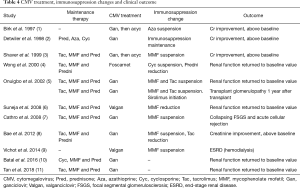
Full table
Discussion
Human CMV is part of the order Herpesvirales, family Herpesviridae, sub-family betaherpesvirinae, genus Cytomegalovirus and species Human Herpesvirus 5 (12). It is one of the most frequent viral pathogens associated with renal transplantation (13). CMV infection is defined as CMV virus isolation in any body fluid or specimen (14). An average of 60% of renal transplant recipients develop active infection and 20% develop symptomatic disease (15). It represents an important cause of opportunistic infections after solid organ transplantation, causing local or disseminated invasive disease. Usually affecting immunocompromised hosts, CMV can cause a myriad of end-organ diseases like pneumonitis, colitis, esophagitis, gastritis, hepatitis, nephritis, among others (16). As other herpes viruses, CMV establishes lifelong latency within the host, with the possibility of reactivation, more common in immunocompromised individuals (16). Risk factors that influence CMV disease after solid organ transplantation include the CMV serostatus of the donor and recipient and the level of immunosuppression (17). There are three paths to CMV infection, each with a different chance of causing clinical disease: primary CMV infection, CMV infection reactivation, and superinfection. In kidney transplantation the source of infection in the majority of allograft recipients (80–90%) is a kidney from a seropositive donor. The remaining infections (10–20%) are due to leukocyte-containing blood products CMV-positive blood donors. Approximately 90% of seronegative kidney transplant recipients that receive kidneys from seropositive cadaveric donors, as opposed to 70% of seronegative recipients of kidneys from seropositive living-related donors, develop laboratory evidence of primary CMV infection after transplantation (18). CMV viremia is defined as the isolation of CMV viral culture. CMV antigenemia is as the detection of CMV pp65 in leukocytes. CMV DNAemia or RNAemia are the detection of the specific nucleic acid through specific diagnostic procedures like PCR, for example (14). The diagnosis of CMV infection is made by detection of the virus in body fluid or tissue specimen in association with a typical clinical manifestation of the disease (19). Tests of antigenemia or DNAemia are preferred over serologic testing or cell cultures (16). Histological examination is useful for differentiating kidney alterations secondary to CMV and allograft rejection. The histological hallmark of CMV infection is the presence of Cowdry Type A viral inclusions, also known as “Owl Eye Inclusions” (20), illustrated in Figure 1. Incidence of primary CMV infections in high-risk patients (patients IgG seropositive for CMV transplant to recipient IgG seronegative) kidney transplants is significantly reduced with valganciclovir prophylaxis (21). Active CMV disease is treated with a combination of antiviral therapy, reduction of immunosuppression and immunomodulation (22). Antivirals (acyclovir, ganciclovir and valganciclovir), have substantially reduced the incidence of CMV-associated disease during early post-transplantation period. Adverse effects, such as neutropenia and impaired cell-mediated immunity are possible (23).
Conclusions
In this systematic literature review, we have summarized the main clinical findings and natural history from 12 CMV kidney allograft infection reported cases in English-language literature. Positive donor serological status was the most influential factor for post-transplant infection, which developed over a wide variety of both clinical and histological presentations. Clinical presentation was mostly symptomatic and clinical outcomes were self-limited in the majority of cases. Prompt pathological diagnosis was a consequence of visualization of viral inclusions in H&E in more than 90% of reports. Awareness as a differential diagnosis in clinical and pathological grounds should be elicited, as in a minority of cases graft failure might be reported.
Acknowledgments
We thank Roberto Silva Costa, pathologist and mentor of our team, and his staff.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Birk PE, Chavers BM. Does cytomegalovirus cause glomerular injury in renal allograft recipients? J Am Soc Nephrol JASN 1997;8:1801-8. [PubMed]
- Detwiler RK, Singh HK, Bolin P. J, et al. Cytomegalovirus-induced necrotizing and crescentic glomerulonephritis in a renal transplant patient. Am J Kidney Dis 1998;32:820-4. [Crossref] [PubMed]
- Shaver MJ, Bonsib SM, Abul-Ezz S, et al. Renal allograft dysfunction associated with cytomegalovirus infection. Am J Kidney Dis 1999;34:942-6. [Crossref] [PubMed]
- Wong KM, Chan YH, Chan SK, et al. Cytomegalovirus-induced tubulointerstitial nephritis in a renal allograft treated by foscarnet therapy. Am J Nephrol 2000;20:222-4. [Crossref] [PubMed]
- Onuigbo M, Haririan A, Ramos E, et al. Cytomegalovirus-induced glomerular vasculopathy in renal allografts: A report of two cases. Am J Transplant 2002;2:684-8. [Crossref] [PubMed]
- Suneja M, Nair R. Cytomegalovirus Glomerulopathy in a Kidney Allograft With Response to Oral Valganciclovir. Am J Kidney Dis 2008;52:e1-4. [Crossref] [PubMed]
- Cathro HP, Schmitt TM. Cytomegalovirus Glomerulitis in a Renal Allograft. Am J Kidney Dis 2008;52:188-92. [Crossref] [PubMed]
- Bae SH, Chung BH, Park YK, et al. Cytomegalovirus induced interstitial nephritis and ureteral stenosis in renal transplant recipient. Korean J Intern Med 2012;27:470-3. [Crossref] [PubMed]
- Vichot AA, Formica RN, Moeckel GW. Cytomegalovirus Glomerulopathy and Cytomegalovirus Interstitial Nephritis on Sequential Transplant Kidney Biopsies. Am J Kidney Dis 2014;63:536-9. [Crossref] [PubMed]
- Batal I, Crew RJ. An 80-year-old kidney transplant recipient with malaise and early allograft dysfunction. Kidney Int 2016;90:455-6. [Crossref] [PubMed]
- Tan SK, Cheng XS, Kao CS, et al. Native kidney cytomegalovirus nephritis and cytomegalovirus prostatitis in a kidney transplant recipient. Transpl Infect Dis 2019;21:e12998. [Crossref] [PubMed]
- Cukuranovic J, Ugrenovic S, Jovanovic I, et al. Viral infection in renal transplant recipients. ScientificWorldJournal 2012;2012:820621. [Crossref] [PubMed]
- Cordero E, Casasola C, Ecarma R, et al. Cytomegalovirus disease in kidney transplant recipients: Incidence, clinical profile, and risk factors. Transplant Proc 2012;44:694-700. [Crossref] [PubMed]
- Ljungman P, Griffiths P, Paya C. Definitions of Cytomegalovirus Infection and Disease in Transplant Recipients. Clin Infect Dis 2002;34:1094-7. [Crossref] [PubMed]
- Sagedal S, Nordal KP, Hartmann A, et al. a Prospective Study of the Natural Course of Cytomegalovirus Infection and Disease in Renal Allograft Recipients1. Transplantation 2000;70:1166-74. [Crossref] [PubMed]
- De Keyzer K, Van Laecke S, Peeters P, et al. Human cytomegalovirus and kidney transplantation: A clinician’s update. Am J Kidney Dis 2011;58:118-26. [Crossref] [PubMed]
- Harvala H, Stewart C, Muller K, et al. High risk of cytomegalovirus infection following solid organ transplantation despite prophylactic therapy. J Med Virol 2013;85:893-8. [Crossref] [PubMed]
- Rubin RH. Impact of cytomegalovirus infection on organ transplant recipients. Rev Infect Dis 1990;12:S754-66. [Crossref] [PubMed]
- Crough T, Khanna R. Immunobiology of Human Cytomegalovirus: from Bench to Bedside. Clin Microbiol Rev 2009;22:76-98. [Crossref] [PubMed]
- Pinkerton H. The morphology of viral inclusions and their practical importance in the diagnosis of human disease. Am J Clin Pathol 1950;20:201-7. [Crossref] [PubMed]
- Paya C, Humar A, Dominguez E, et al. Efficacy and Safety of Valganciclovir vs. Oral Ganciclovir for Prevention of Cytomegalovirus Disease in Solid Organ Transplant Recipients. Am J Transplant 2004;4:611-20. [Crossref] [PubMed]
- Biron KK. Antiviral drugs for cytomegalovirus diseases. Antiviral Res 2006;71:154-63. [Crossref] [PubMed]
- Hodson EM, Ladhani M, Webster AC, et al. Antiviral medications for preventing cytomegalovirus disease in solid organ transplant recipients. Cochrane Database Syst Rev 2013.CD003774. [PubMed]


