
Salvage prostate brachytherapy after definitive external radiation: tried and now tested
Definitive external beam radiation therapy (EBRT) has long been one of the standard treatment modalities for prostate cancer. However, 15–75% of patients will experience a disease recurrence depending on such factors as the risk group, use and length of androgen deprivation therapy (ADT) and radiation dose (1). Approximately 25% of patients with biochemical recurrence will have local clinical disease progression within 5 years (2).
For those opting for salvage therapies, negative metastatic workup and a positive prostate biopsy must be confirmed. Aggressive local salvage therapies include radical prostatectomy, re-irradiation, cryotherapy, and high-intensity focused ultrasound (HIFU). They are associated with significant toxicities although the fistula risk is typically less than 10% (3,4). The option for re-irradiation has mainly been limited to patients initially treated with EBRT salvaged with low dose rate (LDR) or high does rate (HDR) brachytherapy, although repeat EBRT as well as salvage EBRT after brachytherapy have now been described (2,3,5-7). Table 1 summarizes prior experiences of whole gland salvage therapies.
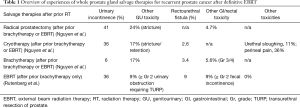
Full table
Unfortunately, most men with biochemically recurrent disease are managed with observation or ADT, and less than 5% of patients are offered curative-intent salvage therapies (8). This is likely from the combination of the lack of expertise and availability of salvage therapies and wanting to avoid the risk of significant toxicities in the elderly population.
RTOG 0526
Despite these challenges the first multicenter, cooperative trial of salvage brachytherapy (SBT) for recurrent prostate cancer after EBRT has now been reported (9). RTOG 0526 was a prospective phase II trial that enrolled 100 patients from 20 centers from 2007–2014. The main eligibility criteria included low- and intermediate-risk patients before EBRT, biopsy-proven disease >30 months after EBRT, prostate-specific antigen (PSA) <10 ng/mL and no nodal or distant disease. The LDR SBT entailed the standard full dose (I-125 to 140 Gy, Pd-103 to 120 Gy) to the whole gland. The primary objective was to evaluate the late gastrointestinal (GI) and genitourinary (GU) adverse events (AEs) for local recurrence after initial EBRT (median =74 Gy; IQR: 70–76 Gy). The late grade ≥3 GI/GU AEs were projected to occur in ≤10% (alternative hypothesis) while ≥20% would be unacceptable (null hypothesis). A sample size of 96 patients was required to detect this effect size with a one-sided significance level of 0.05 and 85% statistical power.
Twelve of the evaluable 87 patients (14%) experienced late grade 3 GI/GU AEs at a median follow-up of 54 months. There were no grade 4 or 5 AEs reported. There were no pretreatment characteristics that predicted for grade 3 AEs. A much larger sample size would have been required to tease out the predictors. Only V100 as a continuous variable was predictive of late GI/GU AEs (P=0.03) and time to first occurrence of late grade ≥3 GI/GU AEs (P=0.02). Post-implant urinary catheterization occurred in 4% (4 patients). The efficacy data is scheduled to be reported later in 2019 with minimum of 5-year follow-up. The investigators should be commended for completing such a challenging trial.
RTOG 0526 proves that SBT is feasible in the multi-institutional, cooperative setting. Furthermore, the grade 3 GI/GU AE rate of 14% with full dose to the whole gland did not exceed pre-specified unacceptable toxicity rate (grade ≥3 GI/GU AEs rate of ≥20%). This toxicity rate is well within the published literature. It has set the standard for full dose LDR SBT when treatment of the entire gland is required. Multiple whole gland HDR SBT experiences with acceptable toxicities have also been reported (10,11).
Focal SBT
While RTOG 0526 was enrolling, significant improvements in MRI-based prostate cancer imaging was occurring. Siddiqui and colleagues at the NCI enrolled 1,003 men from 2007–2014 on a prospective study of targeted prostate biopsies. This study demonstrated that a targeted MRI/ultrasound fusion biopsy was associated with increased detection of high-risk disease and decreased detection of low-risk disease compared to standard ultrasound-guided biopsy in men suspected of prostate cancer (12).
This improvement in MRI has allowed for increasing number of men being treated with focal gland ablation for newly diagnosed prostate cancer. Valerio and colleagues reviewed the literature and described 37 articles with 3,230 men treated focally with modalities such as HIFU, cryotherapy, photodynamic therapy, laser thermotherapy, brachytherapy, electroporation and radiofrequency (13). Similarly, there have been multiple reports on focal salvage therapies with modalities such as cryoablation, SBT with LDR and HDR, HIFU, and stereotactic body radiation therapy (SBRT) (10,14-18). Table 2 summarizes the select focal salvage therapies for MRI visible tumors that have been published.
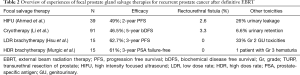
Full table
The rationale for focal salvage therapy is to decrease the toxicity risk by decreasing the prostate volume being treated. This would naturally lead to a lower radiation dose to the urethra, anterior rectal wall and the bladder neck. Focal salvage therapy is possible since the recurrence after EBRT often involves a single focus. Leibovici and colleagues evaluated 50 consecutive salvage prostatectomy specimens after recurrent prostate cancer after radiation (19). A single cancer focus was found in 66% of patients.
The initial experience with focal cryotherapy and HIFU demonstrates a rectourethral fistula rate of 2–3%. This appears not different from whole gland cryotherapy or SBT experiences (15,16). The initial experience with focal LDR and HDR SBT on the other hand seems more encouraging. The efficacy is in line with past whole gland SBT while the toxicity rate seems much lower. Rectourethral fistula was not seen in the prospective trials by Hsu et al. and Murgic et al. (17,18). However, the numbers are small and follow-up periods relatively short.
Future questions
While whole gland therapy remains the standard in multifocal, multicentric recurrent prostate cancer after EBRT, it is hard to justify treating the whole gland in unifocal recurrences. Advancements in prostate MRI imaging has allowed accurate focal salvage therapy delivery, especially LDR and HDR SBT. However, there are many unanswered questions. What margin or volume should be treated? In the trial by Hsu, the recurrent lesion was treated with a tight margin. The whole quadrant of the prostate was treated in the trial by Murgic. In the trial by Hsu recurrences too close to the urethra or anterior rectal wall were not allowed. How close is “too close”? What would be the implications if a second recurrence were to occur close to these structures and the first recurrent focus? Would there be an overlap in SBT doses?
These questions must be answered with well-designed prospective protocols. Long-term follow-up is critical since a second, elsewhere recurrence is always possible and since GU toxicity is notoriously late. Given how difficult it was to complete the RTOG 0526, it is highly unlikely that a randomized trial comparing the different focal salvage therapies will ever be performed. However, a prospective, multi-institutional trial exploring focal LDR or HDR SBT is more feasible and is clearly the next step.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Peters M, Moman MR, van der Poel HG, et al. Patterns of outcome and toxicity after salvage prostatectomy, salvage cryosurgery and salvage brachytherapy for prostate cancer recurrences after radiation therapy: a multi-center experience and literature review. World J Urol 2013;31:403-9. [Crossref] [PubMed]
- Ward JF, Pagliaro LC, Pisters LL. Salvage therapy for radiorecurrent prostate cancer. Curr Probl Cancer 2008;32:242-71. [Crossref] [PubMed]
- Rutenberg MS, Meister M, Amin PP, et al. Salvage external beam radiotherapy for locally recurrent prostate cancer after definitive brachytherapy. Brachytherapy 2016;15:722-9. [Crossref] [PubMed]
- Nguyen PL, D’Amico AV, Lee AK, et al. Patient selection, cancer control, and complications after salvage local therapy for postradiation prostate-specific antigen failure: a systematic review of the literature. Cancer 2007;110:1417-28. [Crossref] [PubMed]
- Burri RJ, Stone NN, Unger P, et al. Long-term outcome and toxicity of salvage brachytherapy for local failure after initial radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 2010;77:1338-44. [Crossref] [PubMed]
- Grado GL, Collins JM, Kriegshauser JS, et al. Salvage brachytherapy for localized prostate cancer after radiotherapy failure. Urology 1999;53:2-10. [Crossref] [PubMed]
- Zilli T, Benz E, Dipasquale G, et al. Reirradiation of Prostate Cancer Local Failures After Previous Curative Radiation Therapy: Long-Term Outcome and Tolerance. Int J Radiat Oncol Biol Phys 2016;96:318-22. [Crossref] [PubMed]
- Tran H, Kwok J, Pickles T, et al. Underutilization of local salvage therapy after radiation therapy for prostate cancer. Urol Oncol 2014;32:701-6. [Crossref] [PubMed]
- Crook JM, Zhang P, Pisansky TM, et al. A Prospective Phase 2 Trial of Transperineal Ultrasound-Guided Brachytherapy for Locally Recurrent Prostate Cancer After External Beam Radiation Therapy (NRG Oncology/RTOG-0526). Int J Radiat Oncol Biol Phys 2019;103:335-43. [Crossref] [PubMed]
- Mbeutcha A, Chauveinc L, Bondiau PY, et al. Salvage prostate re-irradiation using high-dose-rate brachytherapy or focal stereotactic body radiotherapy for local recurrence after definitive radiation therapy. Radiat Oncol 2017;12:49. [Crossref] [PubMed]
- Kollmeier MA, McBride S, Taggar A, et al. Salvage brachytherapy for recurrent prostate cancer after definitive radiation therapy: A comparison of low-dose-rate and high-dose-rate brachytherapy and the importance of prostate-specific antigen doubling time. Brachytherapy 2017;16:1091-8. [Crossref] [PubMed]
- Siddiqui MM, Rais-Bahrami S, Turkbey B, et al. Comparison of MR/ultrasound fusion-guided biopsy with ultrasound-guided biopsy for the diagnosis of prostate cancer. JAMA 2015;313:390-7. [Crossref] [PubMed]
- Valerio M, Cerantola Y, Eggener SE, et al. New and Established Technology in Focal Ablation of the Prostate: A Systematic Review. Eur Urol 2017;71:17-34. [Crossref] [PubMed]
- Duijzentkunst DA, Peters M, van der Voort van Zyp JR, et al. Focal salvage therapy for local prostate cancer recurrences after primary radiotherapy: a comprehensive review. World J Urol 2016;34:1521-31. [Crossref] [PubMed]
- Ahmed HU, Cathcart P, McCartan N, et al. Focal salvage therapy for localized prostate cancer recurrence after external beam radiotherapy: a pilot study. Cancer 2012;118:4148-55. [Crossref] [PubMed]
- Li YH, Elshafei A, Agarwal G, et al. Salvage focal prostate cryoablation for locally recurrent prostate cancer after radiotherapy: initial results from the cryo on-line data registry. Prostate 2015;75:1-7. [Crossref] [PubMed]
- Hsu CC, Hsu H, Pickett B, et al. Feasibility of MR imaging/MR spectroscopy-planned focal partial salvage permanent prostate implant (PPI) for localized recurrence after initial PPI for prostate cancer. Int J Radiat Oncol Biol Phys 2013;85:370-7. [Crossref] [PubMed]
- Murgic J, Morton G, Loblaw A, et al. Focal Salvage High Dose-Rate Brachytherapy for Locally Recurrent Prostate Cancer After Primary Radiation Therapy Failure: Results From a Prospective Clinical Trial. Int J Radiat Oncol Biol Phys 2018;102:561-7. [Crossref] [PubMed]
- Leibovici D, Chiong E, Pisters LL, et al. Pathological characteristics of prostate cancer recurrence after radiation therapy: implications for focal salvage therapy. J Urol 2012;188:98-102. [Crossref] [PubMed]


