Management of adults with prior failed hypospadias surgery
Brief introduction of hypospadias surgery
The initial evaluation of individuals with hypospadias involves localizing the meatus, evaluating for chordee, and inspecting the foreskin. The goal of the initial repair is to ensure that the penis is straight for successful intercourse and that the meatus is as distal as possible in order to create a forwardly directed urinary stream. There are five tenets that are used to assist with this: orthoplasty, urethroplasty, meatoplasty/glanuloplasty, scrotoplasty, and finally skin coverage. Hypospadias repairs can generally be categorized into four types of repairs: urethral advancement procedures, tubularization of the urethral plate, substitution or supplementation of the urethral plate with local tissue or skin flaps, and substitution or supplementation of the urethral plate with grafts.
Hypospadias complications
The term ‘hypospadias cripple’ has been coined for individuals with remaining functional complications after multiple attempts at hypospadias repair. This term, however, is somewhat pejorative and should probably be avoided in contemporary discussion of this problem. Men have a very heavy burden of psychological problems related to the complications of failed hypospadias repair. A recent study (1) shows that individuals who underwent a successful hypospadias repair scored more favorably on a psychosexual questionnaire when compared to individuals who did not have a successful outcome from their repair. Terms like ‘hypospadias cripple’ can further undermine men’s feelings of being whole and confidence in their sexual self-perception.
Complications of the initial hypospadias repair vary widely and include urethrocutaneous fistula formation, urethral stricture, persistent hypospadias, hair in the urethra, urethral stones, penile shortening, and penile curvature (2). Based on a large retrospective review (3), adult men presenting for re-operative intervention have, on average, already undergone three prior attempts at repair.
In the pediatric literature the complication rate of initial hypospadias repair varies depending on the type of repair used. Estimated complication rates, in children, are 4% (4) for distally located meatus using tubularization of the urethral plate, 32% (5) for one stage tubularized preputial flap, and 18% (6) for two stage preputial flap. The leading complication was urethrocutaneous fistula. Also, the complication rate has been shown to be directly proportionate to the experience of the surgeon as there is a decrease in the rate of fistula occurrence for each year a surgeon gains from the end of training (7). Volume of hypospadias repairs also plays a role in success rates as there is an almost 2.5-fold improvement (87% versus 33%) in successful outcome when comparing pediatric urologists to other surgeons (8).
The rate of late complications of hypospadias repair has not been well established. The main difficulty is in establishing the number of patients presenting with complications versus the number of patients that had hypospadias repair as a child without delayed complications. In two recent studies (9,10) that evaluated the overall causes of urethral strictures in adults, complications of previous hypospadias repair was the etiology in 11-13% of all anterior urethral strictures and 26-31% of strictures that involved the penile urethra. These findings are similar to our own results where hypospadias complications accounted for 16% of all anterior urethroplasties at the University of Utah.
Complications after failed hypospadias repair are an important topic for discussion in reconstructive urology, because best practices for management of these complications are not established and these men have a greater risk of requiring multiple surgical procedures. A recent retrospective review from Europe demonstrates this high burden of disease. In this series, 1,100 patients presented for surgical intervention for hypospadias repair related complications; in patients who had a planned single operation (for example fistula closure or single-stage urethroplasty) a mean of 1.2 operations were required, and those patients with planned staged operations required a mean of three operations to achieve a successful or improved outcome (3).
Initial evaluation
The initial evaluation of patients with a history of failed hypospadias repair should encompass the range of complications which occur including: stricture, persistent hypospadias, chordee, and fistula. In the office a complete history and physical should be performed. If possible, operative reports should be obtained from prior repairs; however, this is typically difficult as the repairs occurred many years prior. Similarly, determination of the initial location of the hypospadiac meatus may be difficult due to the intervening surgeries and the passage of time. History should include discussion of urine flow (i.e., weak stream, splayed stream, leakage of urine from skin proximal to the meatus, and billowing of the urethra proximal to the meatus), penile curvature during erection, and ability to have intercourse. Physical examination should include evaluation of the external genitalia from the glans to the perineum evaluating for location of the meatus and evidence of fistulas. If the patient has complaints of bothersome penile curvature then patient supplied photographs of the erect phallus from a dorsal and lateral perspective or clinical observation with induction of an artificial erection with pharmacological agents may be helpful in planning plication due to the significant overestimation of curvature by patients obtained with a history alone (11).
If the patient has urinary complaints, history of hematuria, or urinary tract infections then a cystoscopy should be performed to evaluate for stricture, hair, or urethral stones. If a stricture is found then a retrograde urethrogram with a voiding cystourethrogram will assist to determine the length of stricture. These studies will also provide information about any proximal stricture that has arisen in the bulbar urethra (either from manipulation as a child or chronic obstruction) that may need to be addressed at the time of the surgery.
Stricture repair
Surgical options for those presenting with urethral stricture after hypospadias repair are based on several factors including: location of stricture, length of stricture, and expectations of the patient. Individuals with short strictures especially if the stricture lies outside of the area of previous repair are more likely to undergo a single stage repair including excision and primary anastomosis (EPA), and buccal mucosa onlay grafting (Figure 1).
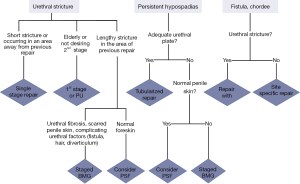
Staged urethroplasty with grafting is appropriate for individuals with a lengthy urethral stricture, persistent hypospadias without an adequate urethral plate, history of multiple failed repairs, and lack of local healthy tissue (Figure 1). The timing between stages varies but is typically between 6 and 12 months. This allows adequate time for graft uptake and allows for the surgeon to evaluate for graft contraction and the need for revision prior to proceeding to the planned final repair.
Surgical options
Single-stage urethroplasty
In studies reporting the use of single-stage urethroplasty, patients underwent repairs with EPA, buccal graft onlay, and a small number with skin graft or skin flap urethroplasty. These repairs are most appropriate in patients with stricture that is proximal to the area of hypospadias repair and well separated from the previous repairs. The reason for more proximal strictures disease in patients with previous hypospadias repair is not well understood. It could be these strictures arise from the manipulation associated with their hypospadias repair, previous treatment with a perineal urethrostomy at some period of the patient’s care, or the effects of chronic obstruction and high pressure voiding from more distal stricture disease. At the University of Utah, we have found concomitant proximal strictures in 16% of patients undergoing repair of failed distal hypospadias repair.
Excision and primary anastomosis (EPA)
EPA is used predominantly in patients with a relatively short stricture lying outside the location of prior hypospadias repair.In general, EPA is felt to have one of the highest success rates of any urethroplasty technique with reports ranging from 90-99% (12-14). Care must be taken in translating these results into patients with hypospadias. Hypospadias will affect the blood supply to the distal urethra by disrupting retrograde arterial flow due to the loss of the distal normal corpora spongiosa tissue. EPA is partially dependent upon this retrograde blood flow from the arborization of the penile arteries with the bulbar arteries within the glans. If EPA is used, it is important to limit the distal mobilization of the urethra in order to preserve perforating vessels that feed the bulbar urethra separate from the more distal blood supply arising from the penile arteries. For this reason, it is worthwhile to use onlay graft urethroplasty liberally in these cases.
Preputial skin flap
The use of preputial skin flaps is uncommon in patients undergoing repair of hypospadias complications due to the lack of adequate foreskin from the initial hypospadias repair or extensive scarring from the previous operations. A retrospective review of 58 patients (15) who underwent single stage preputial flap urethroplasty for strictures measuring on average 4.8 cm (range, 2.6-8.5 cm) reported a success rate of 81% with a 42 month average follow up. Statistically significant predictors of failure in this group were history of smoking and history of diabetes mellitus. Success with single-stage urethroplasty (90%) was reported in a large cohort of men with failed hypospadias repair from Europe, where 20% of the single-stage urethroplasties involved a penile skin flap (PSF) (3). In contrast to these findings, others have found that the utilization of either local penile flaps or penile circular fasciocutaneous flaps have an ultimate failure rate of 42%, with 75% of patients requiring secondary procedures (2,16). Ideally these flaps are best used if there is a recurrent hypospadias rather than stricture disease and the preputial skin shows no evidence of scarring or lichen sclerosis.
Single-stage buccal graft repair
Buccal graft is used for lengthy strictures, measuring over 3 cm, when excision with anastomosis would cause ventral penile curvature or result in an anastomosis on tension. The use of single stage buccal graft urethroplasty in hypospadias failure is limited for several reasons. Most of the strictures recur in the previous repair site in the penile urethra and even under the best of circumstances mobilization of the penile urethra for dorsal placement of a buccal graft is challenging. Other methods of placing the graft are ventral onlay of the buccal mucosa, however, many believe that even normal penile corpora spongiosus lacks the thickness to support a buccal graft and there is no normal surrounding spongiosal tissue in patients with hypospadias. Finally, an ASOPA technique (17) can be used where the graft is placed through a ventral incision in the urethra. However, this technique is not ideal either, as the dorsum of the urethra has to be mobilized significantly to make space for the graft and patients with a ventral incision in the already scarred and ischemic urethra will be prone to fistula or complete breakdown of this incision. In addition, many patients have significant urethral fibrosis and need the entirety of the scarred penile urethra removed and single stage tubularization of a buccal graft has an unacceptably high stenosis rate (18). It is for these reasons that single-stage buccal graft onlay urethroplasty should be reserved for the previously mentioned proximal urethral strictures that can arise in the bulbar urethra separate or contiguous with more distal stricture.
Staged urethroplasty
Patients that undergo a staged urethroplasty usually have significant urethral fibrosis involving the prior area of hypospadias repair and often have a history of multiple failed repairs. Important considerations, in staged repair, are the material to use for urethral substitution, as well as how to place the graft and whether the diseased urethra needs to be removed.
Most recent reports on staged urethroplasty in patients with hypospadias have focused on hairless abdominal skin or buccal mucosa for urethral substitution. In a small series of patients, there was shown to be excellent outcomes using hairless abdominal skin as a full thickness skin graft. The success rate in this series was 87% although only 24% had hypospadias as the etiology of the strictures (19). Despite this, many surgeons worry about the long-term durability of a skin based urethroplasty. The attractive part of this approach is that the abdominal skin is readily available and the harvest of the skin has such low morbidity. Buccal mucosa is a more commonly utilized graft material for urethral replacement in hypospadias salvage (2,3,20,21). A wide graft must be taken, measuring 3 cm in width, to compensate for the estimated 15% contracture in graft width. Once tubularized during the second stage this would yield a urethra measuring 24 French.
Another area of controversy in staged urethroplasty is treatment of the scarred urethral plate. Some argue that the urethral plate should be removed completely since it is often scarred, not usable and frequently histologically has evidence of lichen sclerosis (ballanitis xerotica obliterans) (3). The argument for saving the urethral plate is that in many cases the urethral plate still has some width and the amount of buccal graft can be minimized. A urethral plate that may be worth preserving would likely be 8-12 French in size as this would open to 0.8-1.2 cm in width. If the urethral plate is preserved then the buccal mucosa graft can be split around it with excision of the most distal portion, which is usually the most stenotic segment. This arrangement is like a pair of pants with the seat of the pants oriented at the future meatus and glans. Alternatively, the urethral plate can be split ventrally and dorsally, with placement of the graft dorsally between the two laterally split portions of the urethra. The potential advantage of this approach is that the urethra takes well to the corporal bodies and does not need to be mobilized in a second stage closure.
One important surgical consideration in placement of the graft in the 1st stage is to adequately quilt the graft to the underlying corporal body (Figure 2). Also, it is best if there is tunica dartos or soft tissue to support the lateral edges of the graft material. This will help ensure a good blood supply during mobilization of the edges of the graft for tubularization. A bolster dressing is sewn to the underside of the graft with the Foley catheter running through the dressing (Figure 2). This remains in place for 5-6 days and is kept moist. This is removed along with the Foley catheter. Patients then use a petroleum based moisturizer like Vaseline® or Aquaphor® on the graft (2-3 times per day) until they are ready for 2nd stage urethroplasty. Second stage urethroplasty is performed 6-12 months later. Our personal practice is to wait 12 months prior to closure. It is important to evaluate the proximal urethra, urethrotomy, and graft for contraction prior to second stage urethroplasty. A number of patients will invariably have graft contraction and require revision or replacement of the graft. This complication occurs in 19-22% (21,22) and can be a frustrating situation without easily identifiable causes of the problem. The end graft should be 2.5-3 cm in width to allow for some contraction from healing in the second stage closure. If the bed for the graft is unsuitable, one can consider supporting the graft with a tunica vaginalis flaps affixed to the corporal bodies.

In second stage urethroplasty, care must be taken to mobilize the urethral edges as little as possible in order to prevent devascularization of the graft material (18). This creates a somewhat ovoid cross-section of the final tubularization. The ventral incision should be closed in two layers, minimizing the risk of ventral fistula formation. Adequate coverage of ventral repair in hypospadias surgery has been shown to be critical for prevention of fistula formation (23), which is one of the most common complications of the surgery. Local dartos flaps can provide adequate coverage, but often the penis is lacking this subtle soft tissue due to scarring from previous surgery, or the tissue has already been used to supplement the lateral aspects of the graft in the first stage operation. In these cases a well mobilized tunica vaginalis flap provides very robust tissue for coverage of the ventral incision (Figure 3) (24). It is the ventrum of the urethra, which is most exposed to breakdown in the second stage operation and any pressure can cause this incision to come apart. For this reason we place a suprapubic cystotomy in most cases at the time of second stage repair. The urethral catheter is left but plugged and the suprapubic cystotomy serves to drain the bladder while healing takes place. This strategy avoids any ventral pressure on the incision from a full urinary drainage bag pulling on the catheter. Usually the patient begins to spontaneously void at 3-4 weeks once the Foley is removed. Small fistulas that develop shortly after beginning voiding will often heal with additional catheter drainage (25).
Not all men ultimately elect to undergo second stage urethroplasty closure. The reported rates of men that do not go on to secondary closure are about 30% (2,26). There are multiple reasons for this observation. One explanation is that some men when they experience unobstructed voiding and resolution of urethral pain, urinary tract infections, or hematuria do not want to risk the complications associated with closure of the 1st stage urethroplasty. Another reason that some men do not undergo closure is that they have graft contracture and are facing additional buccal graft revision of the urethral plate and they decide additional surgery is not worth the morbidity, considering that they are voiding without difficulty.
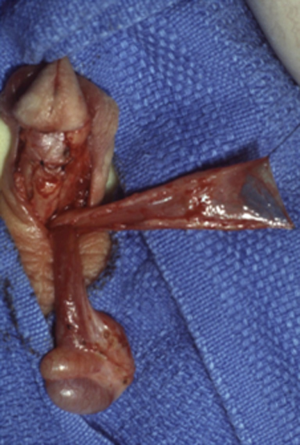
Closure of urethrocutaneous fistula
Of the presenting complications, urethrocutaneous fistula formation is one of the most commonly seen after hypospadias repair. It is reported at about 20-50% of cases (2,20,27-29), depending upon the nature of the repair. Small fistulae that are evident shortly after repair may heal with additional catheter drainage (2); however, persistent fistulae may need to be closed. Identification of fistulae is accomplished by irrigating the meatus in a retrograde fashion with saline. Primary repair of the fistulae is performed by excising the fistulous tract followed by closure of the urethra in two layers with fine absorbable suture. After all fistulae have been excised and the urethra repaired then a tissue interposition flap should be used due to the established ischemia of the surrounding skin, which was presumably the cause of the fistula. This tissue flap will minimize the risk of recurrence. Local dartos tissue or a tunica vaginalis flap (24) usually will make a very healthy flap for this purpose. Harvesting of the flap may be done by making a separate scrotal incision. The flap is then tunneled to the level of the fistula and affixed overlaying the fistula. If a tunica vaginalis flap is used care should be taken to adequately mobilize the flap so tethering the penis does not occur (Figure 3).
Chordee repair
Repair of ventral penile curvature has been described by several methods. Initially repairs were aimed at excising fibrous tissue bands connecting the superficial Dartos fascia to the deep Bucks fascia or excising ventral tissue thought to be fibrous in nature, which acts to tether the penis ventrally. Recent histological studies on these tissues have actually shown them to be normal in appearance and not rich in fibroblasts (30,31). A theory to explain this observation is that there is a developmental disproportionate growth of the dorsal tunica albuginea compared to the ventral side.
When stricture is present as well as chordee it is tempting to assume that release of the scarred urethral plate will restore a straight erection. Unfortunately we have not found this to be the case and in all cases with significant ventral chordee we have had to perform dorsal plication. This observation may further support an inherent disproportion in the corporal bodies rather than ventral tethering from scarring as the main cause of chordee, even when chordee is present in the setting of multiple failed previous operations for hypospadias. We try to fix chordee at the time of first stage urethroplasty if patients have concomitant urethral stricture. The reason for this is that patients will have ample opportunity to evaluate the effect of the straightening surgery and any further problems with erections can be addressed at the second stage closure of the urethra.
In order to repair chordee an artificial erection is induced with papavrine and saline irrigation with a tourniquet. Generally a Lue “dot” plication technique is used dorsally on the tunica albuginea of the corporal bodies (32-34). However, in the presence of micropenis and penile urethra stricture a lengthening procedure may be attempted with grafting of the ventral corporal bodies. The dorsum of the corporal bodies can be approached after degloving the penis with a subcoronal circumcising incision or by inversion of the penis through a low transverse suprapubic incision. However, if the penis has scarring from previous hypospadias repair it may be advisable to make an incision directly over the site of plication on the dorsum of the penis. A counter incision like this will have the least chance of causing ischemia to skin flaps that were used in the hypospadias repair, although it does leave a more visible phallic scar.
Adjuncts to urethroplasty for failed hypospadias
Use of biologically based glue
The use of fibrin sealant has been studied in the application of skin grafts in patients after serious burns. Two recent studies (35,36) have evaluated the use of this strategy and noted significantly better graft uptake parameters in the groups with fibrin sealant including graft adherence, quality of healing, and reduction in hematoma formation. Fibrin sealant has also been used for dorsal buccal grafting and was described as an adjunct in one of the original manuscripts on dorsal buccal graft onlay (37). The sealant was used as a base coating on the tunica albuginea on which the graft was laid upon and then was applied again to the urethra around the location of the graft after it was seated in its anatomical position. Although it would be difficult to study since the power to detect a difference in outcome would necessitate a very large series, anything that can be done to minimize graft contracture, like potentially the use of fibrin sealant on the graft bed, may decrease the number of repeat operations needed after the first stage buccal graft onlay.
Tunica vaginalis flap
Due to the poor surrounding tissue quality in individuals who have undergone multiple hypospadias revision, revascularization of the newly repaired tissue is paramount. The use of tunica vaginalis flaps has been described during fistula repair and as an adjunct ventral closure of hypospadias (24). We utilize tunica vaginalis flaps mostly to cover a lengthy or marginal ventral suture line at the time of second stage urethroplasty. However, we have also used the flap to cover the corporal body and as a bed for the buccal graft if local tissue is too scarred (Figure 3).
Overall success
Urethroplasty in patients with failed hypospadias repair has a very high complication rate. Even in the best of hands, multiple repairs are often needed in order to obtain a “successful” or in reality often an improved outcome. Multiple studies have noted that 24-32%, 7-12%, and 3-4% patients needed approximately two, three and even four repairs respectively (2,3). Successful outcomes, which may occur after multiple surgeries, have been established at around 88%. When repairs that are single-stage are omitted, which we would roughly expect to approximate the outcomes in men without a history of hypospadias, the outcomes are worse. For this reason it is very important to counsel men undergoing repair of failed hypospadias surgery about the multitude of complications that can occur. Urethral fistula, recurrent stricture, chordee, erectile dysfunction, and loss of penile sensation are some of the complications that are entirely common.
The last point worthy of mention is counseling appropriate patients for perineal urethrostomy. Properly performed perineal urethrostomy has a success of >90% in patients without radiation injury (22,26). Many men, when they have had multiple hypospadias surgery failures prefer a simple solution with a high success rate. Most of these men are sitting to void due to spraying at baseline and conversion to a perineal urethrostomy does not change their voiding habits. In addition, there is very low risk of penile complications, such as chordee, pain and loss of erections or sensation with perineal urethrostomy. Recovery is easier and secondary surgeries are not needed other than for rare cases of re-stricture of the perineal urethrostomy. The use of perineal urethrostomy should especially be emphasized in older men that do not care about pregnancy or ejaculation/urination from the meatus. Some of the happiest patients in our practice are those that have dealt with a lifetime of urethral complications like pain, urinary tract infections, and the need for repeated procedures who are cured with a single relatively simple surgery—perineal urethrostomy.
Conclusions
Hypospadias complications in adults are a challenging reconstructive problem. The outcomes are not assured and patients often require multiple surgeries to achieve a satisfactory outcome. There are a multitude of reconstructive options for management of the various complications that adult patients have after failed hypospadias repair. Staged urethroplasty is mostly required when strictures arise in the pendulous urethra at the site of previous hypospadias repairs due to the ischemic and poor quality of the remaining reconstructed urethra.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Kiss A, Sulya B, Szász AM, et al. Long-term psychological and sexual outcomes of severe penile hypospadias repair. J Sex Med 2011;8:1529-39. [PubMed]
- Myers JB, McAninch JW, Erickson BA, et al. Treatment of adults with complications from previous hypospadias surgery. J Urol 2012;188:459-63. [PubMed]
- Barbagli G, Perovic S, Djinovic R, et al. Retrospective descriptive analysis of 1,176 patients with failed hypospadias repair. J Urol 2010;183:207-11. [PubMed]
- Snodgrass WT, Bush N, Cost N. Algorithm for comprehensive approach to hypospadias reoperation using 3 techniques. J Urol 2009;182:2885-91. [PubMed]
- Ghali AM. Hypospadias repair by skin flaps: a comparison of onlay preputial island flaps with either Mathieu’s meatal-based or Duckett’s tubularized preputial flaps. BJU Int 1999;83:1032-8. [PubMed]
- Arshad AR. Hypospadias repair: Byar’s two stage operation revisited. Br J Plast Surg 2005;58:481-6. [PubMed]
- Horowitz M, Salzhauer E. The ‘learning curve’ in hypospadias surgery. BJU Int 2006;97:593-6. [PubMed]
- Titley OG, Bracka A. A 5-year audit of trainees experience and outcomes with two-stage hypospadias surgery. Br J Plast Surg 1998;51:370-5. [PubMed]
- Lumen N, Hoebeke P, Willemsen P, et al. Etiology of urethral stricture disease in the 21st century. J Urol 2009;182:983-7. [PubMed]
- Palminteri E, Berdondini E, Verze P, et al. Contemporary urethral stricture characteristics in the developed world. Urology 2013;81:191-6. [PubMed]
- Bacal V, Rumohr J, Sturm R, et al. Correlation of degree of penile curvature between patient estimates and objective measures among men with Peyronie’s disease. J Sex Med 2009;6:862-5. [PubMed]
- Barbagli G, De Angelis M, Romano G, et al. Long-term followup of bulbar end-to-end anastomosis: a retrospective analysis of 153 patients in a single center experience. J Urol 2007;178:2470-3. [PubMed]
- Eltahawy EA, Virasoro R, Schlossberg SM, et al. Long-term followup for excision and primary anastomosis for anterior urethral strictures. J Urol 2007;177:1803-6. [PubMed]
- Santucci RA, Mario LA, McAninch JW. Anastomotic urethroplasty for bulbar urethral stricture: analysis of 168 patients. J Urol 2002;167:1715-9. [PubMed]
- Mathur RK, Nagar M, Mathur R, et al. Single-stage preputial skin flap urethroplasty for long-segment urethral strictures: evaluation and determinants of success. BJU Int 2014;113:120-6. [PubMed]
- Whitson JM, McAninch JW, Elliott SP, et al. Long-term efficacy of distal penile circular fasciocutaneous flaps for single stage reconstruction of complex anterior urethral stricture disease. J Urol 2008;179:2259-64. [PubMed]
- Asopa HS, Garg M, Singhal GG, et al. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology 2001;58:657-9. [PubMed]
- Andrich DE, Mundy AR. Substitution urethroplasty with buccal mucosal-free grafts. J Urol 2001;165:1131-3. [PubMed]
- Meeks JJ, Erickson BA, Fetchev P, et al. Urethroplasty with abdominal skin grafts for long segment urethral strictures. J Urol 2010;183:1880-4. [PubMed]
- Leslie B, Lorenzo AJ, Figueroa V, et al. Critical outcome analysis of staged buccal mucosa graft urethroplasty for prior failed hypospadias repair in children. J Urol 2011;185:1077-82. [PubMed]
- Kozinn SI, Harty NJ, Zinman L, et al. Management of complex anterior urethral strictures with multistage buccal mucosa graft reconstruction. Urology 2013;82:718-22. [PubMed]
- Myers JB, Porten SP, McAninch JW. The outcomes of perineal urethrostomy with preservation of the dorsal urethral plate and urethral blood supply. Urology 2011;77:1223-7. [PubMed]
- Furness PD 3rd, Hutcheson J. Successful hypospadias repair with ventral based vascular dartos pedicle for urethral coverage. J Urol 2003;169:1825-7; discussion 1827.
- Snow BW, Cartwright PC, Unger K. Tunica vaginalis blanket wrap to prevent urethrocutaneous fistula: an 8-year experience. J Urol 1995;153:472-3. [PubMed]
- Breyer BN, McAninch JW, Whitson JM, et al. Multivariate analysis of risk factors for long-term urethroplasty outcome. J Urol 2010;183:613-7. [PubMed]
- Elliott SP, Eisenberg ML, McAninch JW. First-stage urethroplasty: utility in the modern era. Urology 2008;71:889-92. [PubMed]
- Li Q, Li S, Chen W, et al. Combined buccal mucosa graft and local flap for urethral reconstruction in various forms of hyposapdias. J Urol 2005;174:690-2. [PubMed]
- Snyder CL, Evangelidis A, Hansen G, et al. Management of complications after hypospadias repair. Urology 2005;65:782-5. [PubMed]
- Meeks JJ, Erickson BA, Gonzalez CM. Staged reconstruction of long segment urethral strictures in men with previous pediatric hypospadias repair. J Urol 2009;181:685-9. [PubMed]
- Baskin LS, Erol A, Li YW, et al. Anatomical studies of hypospadias. J Urol 1998;160:1108-15. [PubMed]
- Snodgrass W, Patterson K, Plaire JC, et al. Histology of the urethral plate: implications for hypospadias repair. J Urol 2000;164:988-9. [PubMed]
- Brant WO, Bella AJ, Lue TF. 16-Dot procedure for penile curvature. J Sex Med 2007;4:277-80. [PubMed]
- Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol 2002;167:2066-9. [PubMed]
- Mobley EM, Fuchs ME, Myers JB, et al. Update on plication procedures for Peyronie’s disease and other penile deformities. Ther Adv Urol 2012;4:335-46. [PubMed]
- Foster K, Greenhalgh D, Gamelli RL, et al. Efficacy and safety of a fibrin sealant for adherence of autologous skin grafts to burn wounds: results of a phase 3 clinical study. J Burn Care Res 2008;29:293-303. [PubMed]
- Mittermayr R, Wassermann E, Thurnher M, et al. Skin graft fixation by slow clotting fibrin sealant applied as a thin layer. Burns 2006;32:305-11. [PubMed]
- Barbagli G, De Stefani S, Sighinolfi MC, et al. Bulbar urethroplasty with dorsal onlay buccal mucosal graft and fibrin glue. Eur Urol 2006;50:467-74. [PubMed]


