The reconstructive urology work force: present and future
How many reconstructive urologists do we have in the US?
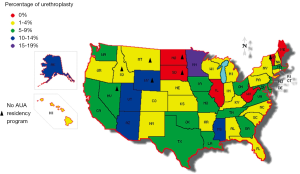
There is no direct way to know how many qualified practitioners are providing reconstructive urology in the USA, or their distribution nationally. However, there are indirect means to estimate the number of active reconstructive urologists, and even estimate their distribution. We performed one revealing analysis using the indirect measure of case number reports by urologists applying for board certification or recertification (1). In that analysis, the number of urethroplasties performed in any given US state varied hugely. The proportion of patients who had urethroplasty (versus dilation or urethrotomy) ranged from 0-17%, depending on the state. Five US states reported no urethroplasties at all, despite the fact that the series contained more than 4,800 urologists reporting over a 5-year period (Figure 1). Eliminating those states with zero urethroplasties, the rate of urethroplasties could vary by as much as 150-fold between geographic areas. There was one hopeful trend: the younger urologists who were certifying had a 300% higher rate of urethroplasty than the older urologists that were recertifying (12% vs. 4%). These data represent only a snapshot in time, and in no way capture the surgical activity of doctors not certifying/recertifying in that 5-year period, but they are useful nonetheless. This dataset shows deep regional deficiencies in the number of reconstructive urologists in the US. Clearly, our population is not being served by adequate numbers of reconstructive urologists. This is no surprise, as the nation is short of urologists in general and there has been a further decreasing supply of urologists in relation to population. In the last decade, 24% of all the counties in the US lost urologists relative to their population growth (2).
Considering that the incidence of urethral stricture rises sharply (6-fold) after age 55 (3), the future should require even more practitioners with knowledge of urethroplasty. Considering that the US will have about 14 million more men age over 60 in 2020 compared to 2010 (http://www.aoa.gov/AoARoot/Aging_Statistics/future_growth/docs/By_Age_and-Gender_Persons_60_and_over.xls), we can expect that over the next decades, the number of patients in need of reconstructive urology will also grow. The problem of inadequate numbers and distribution of reconstructive-trained urologists will worsen further over the next decade.
Why it matters: most patients are getting repeat dilations instead of potentially curative urethroplasties
These data also show that most patients do not get curative reconstructive surgery when they have strictures, proving at least the need for more urologic expertise/training in open urethroplasty. On average in our country, patients with stricture are treated only 6% of the time with urethroplasty and 94% of the time with dilation/DVIU (4). In some series, dilation/DVIU ×2 is 50 times more commonly performed than urethroplasty (5), despite the fact that these procedures were deemed by Anger et al. (5) “neither curative nor cost effective” (6-10). Clearly most US patients are not getting the best treatment for their strictures, and most practitioners do dilation/DVIU, despite that fact that the cure rate for dilation is an appalling 12% (8) and for first urethrotomy is at best 50% (6-8) and may be closer to 0% (4). The cure rate for second urethrotomies is thought, in fact, to approach zero (4) and the cure rate for anything but the shortest strictures <1 cm is very poor. Strictures longer than 1 cm have a 390% higher failure rate after dilation/urethrotomy than short strictures <1 cm long (6). Because most strictures are in fact longer than 1 cm worldwide, the expected cure rate of DVIU is generally poor.
This lack of urologic reconstruction expertise is further proven by the work of Ferguson et al. (11). They showed that the majority of polled urologists (80%) favored repeated “neither curative nor cost effective (5)” dilations for recurrent strictures, instead of doing potentially curative urethroplasty. Too many of the urologist responding to the poll (25%) also did not ascribe to the very concept that initially failed dilation/DVIU ×2 is often best followed by urethroplasty. Clearly, urologic reconstruction expertise and knowledge is lacking in our country.
How many urethral stricture patients are there?
The true number of urethral stricture patients in the US is also unknown. However, the Urologic Diseases in America project used ten public and private patient registries, interpreted by expert health epidemiologists, to estimate the burden of stricture disease (3). In that 2,000 dataset, there were 5,000 inpatient visits and 1.5 million office visits for urethral stricture yearly. For perspective, realize that both of these figures are higher than that for so called “common” urologic problem such as urolithiasis. In fact, outpatient hospital or surgicenter visits for urethral stricture were actually twice as common as those for urinary lithiasis. In 2001, there were almost 20,000 dilations per 100,000 Medicare beneficiaries, a number that exceeded the number of ureteroscopies by almost double. It is a common problem!
Another way to thumbnail estimate the number of urethral stricture patients in the US is to estimate of the number of urethral stricture patients seen by an average urologist. In a 2011 survey, Ferguson et al. (11) determined that the average urologist treated five urethral strictures a year. It is of course unknown how many patients were seen during those five stricture treatment visits, as some patients may present more than once a year. However, if we calculate that there are approximately 9,775 active urologists in the US (2) one can speculate approximately 9,775×5=48,875 urethral strictures visits a year in the US. We are a busy reconstructive urology center, but we tend to perform about 150 urethroplasties a year and maintain a patient load that generally exceeds our capacity by about 10%. Many more busy reconstructive urologists will be needed before this large number of stricture patients can be treated properly.
Other, non-urethral stricture related diseases also require reconstructive expertise
This chapter has discussed the burden of urethral stricture disease, and its urethroplasties common inadequate treatment in the US, partly because of lack of qualified experts. However, the burden of reconstructive urology is not limited to urethral stricture. At our center, we do surgery for many other problems: buried penis, penile trauma, Peyronie’s disease, vesicovaginal fistula, vesicorectal fistula, colovesical fistula, ureteral obstruction, incontinence (artificial urinary sphincter AUS and male sling), post-Fournier’s reconstruction and others. The burdens of these diseases are unknown, but they add to the already significant numbers of patients that require a reconstructive urologist.
Trends in training
The most obvious trend in urologic reconstruction today is an explosion in the number of qualified fellowship training centers nationally and even internationally. When I finished my fellowship in 2000, there were perhaps three bona fide fellowships in reconstructive urology in the country. Now in the Society for Genitourinary Reconstruction match (http://www.societygurs.org/fellowship.html), there are at least 13 fellowship programs in the US, and another notable two in foreign countries (India, England) that can train US urologists—a 500% increase in 13 years. This number should grow modestly in the next years as more programs with high volumes of reconstructive patients and excellent reconstructive skills/training open up even more fellowship programs. While some have worried that this means we may over train reconstructionists and flood the market, it is clear that huge geographic swaths of America lack reconstructive experts and that the risk of this will remain low for the foreseeable future.
At every US reconstruction center, residents are also presumably performing/learning a larger number of cases than in the past. My residents perform about 50 cases a year as primary surgeon. After training, they can reliably perform most urethroplasty, and tend to do so when they are out in practice. (I must editorialize that when our residents do these cases, they make every cut and throw every stitch: they do not merely observe and thus are well-trained in the subtleties of the procedures. Your mileage may vary). Training residents properly should create even more practitioners that can perform urethroplasty. It is my unscientific opinion that a buccal urethroplasty is about 1/3 as difficult as a radical prostatectomy: it is something that can and should be taught widely. In past years, many operations that were the sole territory of “super experts” went mainstream and now are done by many nonspecialty urologists: ureteroscopy, neobladder, laparoscopy, robotics, and more. It is my dream that cases as simple as most anastomotic or buccal urethroplasties can be done by general practitioners, just as many technically demanding surgeries are done by them today.
The future
In summary, there are too many “neither cost effective nor curative” dilations and urethrotomies occurring in the US, and a dearth of potentially curative urethroplasties. There are three major reasons: (I) lack of knowledge of how to do urethroplasty among urologists (12); (II) lack of access to experts to refer patients to (1); and (III) lack of knowledge that urethroplasty is superior than DVIU/dilation for long, or recurrent strictures (12). Recent increases in the number of centers of excellence that are training both residents and fellows in reconstructive techniques should go a long way to remedying this deficiency.
Acknowledgements
None.
Footnote
Conflicts of Interest: The author has no conflicts of interest to declare.
References
- Burks FN, Salmon SA, Smith AC, et al. Urethroplasty: a geographic disparity in care. J Urol 2012;187:2124-7. [PubMed]
- Neuwahl S, Thompson K, Fraher E, et al. HPRI data tracks. Urology workforce trends. Bull Am Coll Surg 2012;97:46-9. [PubMed]
- Santucci RA, Joyce GF, Wise M. Male urethral stricture disease. J Urol 2007;177:1667-74. [PubMed]
- Santucci R, Eisenberg L. Urethrotomy has a much lower success rate than previously reported. J Urol 2010;183:1859-62. [PubMed]
- Anger JT, Buckley JC, Santucci RA, et al. Trends in stricture management among male Medicare beneficiaries: underuse of urethroplasty? Urology 2011;77:481-5. [PubMed]
- Pansadoro V, Emiliozzi P. Internal urethrotomy in the management of anterior urethral strictures: long-term followup. J Urol 1996;156:73-5. [PubMed]
- Greenwell TJ, Castle C, Andrich DE, et al. Repeat urethrotomy and dilation for the treatment of urethral stricture are neither clinically effective nor cost-effective. J Urol 2004;172:275-7. [PubMed]
- Heyns CF, Steenkamp JW, De Kock ML, et al. Treatment of male urethral strictures: is repeated dilation or internal urethrotomy useful? J Urol 1998;160:356-8. [PubMed]
- Rourke KF, Jordan GH. Primary urethral reconstruction: the cost minimized approach to the bulbous urethral stricture. J Urol 2005;173:1206-10. [PubMed]
- Wright JL, Wessells H, Nathens AB, et al. What is the most cost-effective treatment for 1 to 2-cm bulbar urethral strictures: societal approach using decision analysis. Urology 2006;67:889-93. [PubMed]
- Ferguson GG, Bullock TL, Anderson RE, et al. Minimally invasive methods for bulbar urethral strictures: a survey of members of the American Urological Association. Urology 2011;78:701-6. [PubMed]
- Bullock TL, Brandes SB. Adult anterior urethral strictures: a national practice patterns survey of board certified urologists in the United States. J Urol 2007;177:685-90. [PubMed]


