The use of a homemade rate adjustment card in patients with continuous bladder irrigation after transurethral resection of the prostate
Introduction
Benign prostatic hyperplasia (BPH) is the most common cause of urination dysfunction in middle-aged and elderly men (1). Patients present atypical clinical symptoms in the early stage and then bladder irritation and obstruction along with their associated complications as the condition progresses (2), which seriously affect the quality of life (3). Transurethral resection of the prostate (TURP) is the gold standard for surgical treatment of BPH (4); its advantages include wide indications, small incision, and good outcomes (5). The most common complications in the early post-TURP stage are postoperative bleeding and bladder spasm (6,7). Clot-related catheter blockage in the early postoperative stage may induce bladder spasm, which in turn aggravates bleeding and blockage. To prevent the vicious cycle of bleeding, catheter blockage, and bladder spasm (8), continuous bladder irrigation (CBI) is routinely performed after operation (9). However, an improper CBI rate is another cause of bladder spasm and bleeding, and the CBI rate can be properly adjusted based on the color of the drainage fluid (10). Most nurses manually adjust the irrigation rate based on their subjective evaluation of the color of the drainage fluid, which may affect clinical outcomes depending on each nurse’s clinical experience and skill level (11). It is difficult to quantify how much to adjust the post-TURP CBI rate based on the color of drainage fluid (12). In this study, we developed and evaluated the effect of a post-TURP CBI rate adjustment card in BPH patients undergoing post-TURP CBI in order to provide a scientific basis for objectively evaluating the color of drainage fluid and precisely adjusting the CBI rate. We present the following article in accordance with the TREND reporting checklist (available at http://dx.doi.org/10.21037/tau-20-1288).
Methods
General information
BPH patients who received post-TURP CBI at our hospital between April and July 2020 were enrolled in this study. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). Inclusion criteria were as follows: (I) 60 to 80 years of age; (II) BPH confirmed by ultrasound B, urodynamics, and serum prostate-specific antigen; (III) normal coagulation before operation; and (IV) elective TURP. Exclusion criteria were as follows: (I) prostate cancer, neurogenic bladder, bladder neck sclerosis, or other urethral conditions; (II) other severe organic disorders; and (III) use of an analgesic pump after operation. Each patient signed the informed consent before the study, which was approved by Medical Ethics Committee, First Affiliated Hospital of Soochow University [(approval No. (2020) EC 017). A total of 103 eligible patients were enrolled in this study and were assigned to the control group (n=49) or the experimental group (n=54) according to the different hospital areas. No significant between-group difference was observed in sex, age, or underlying diseases (P>0.05) (Table 1). All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
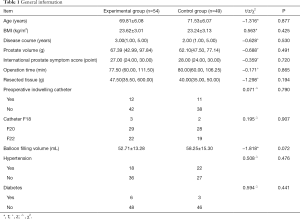
Full table
Study methods
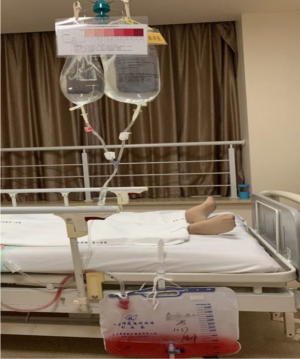
Routine post-TURP CBI
After TURP, all the patients received CBI through an indwelling three-lumen catheter. The bladder irrigation solution was 3 L per bag, which was placed at 60 cm above the bladder for irrigation at room temperature (25 °C). During CBI, the patient was closely monitored for catheter patency. In case of any blockage due to clots, the catheter was gently squeezed and repositioned, or a syringe was used to flush the catheter repeatedly with sterile saline if needed until the blockage was cleared. Urine output, the input of irrigation solution, and liquid output were recorded (urine output = liquid output − the input of irrigation solution); and the color and property of drainage were observed. A gauze was secured at the urethral opening for light traction for 12 h. The patients were instructed to avoid unnecessary changes in position for 24 h after operation; meanwhile, they received passive movement and proper care to prevent pressure sores or lower limb thrombosis. Mental counseling was also provided as needed.
Control group
In the control group, the irrigation rate was adjusted according to the standard of care. Specifically, the nurse evaluated the color of the CBI drainage fluid under bright light and increased the rate if the color was dark, and vice versa (10).
Experimental group
In the experimental group, the irrigation rate was adjusted with the post-TURP CBI rate adjustment card.
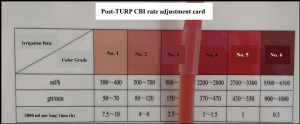
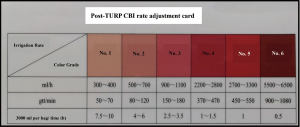
- The card was made of plastic, 15 cm × 10 cm, with two parts: color grade and irrigation rate (Figure 1). Our pilot study demonstrated the consistency of the color grade, which included six colors commonly seen in clinical practice. We applied for a patent for the card in April 2020. The quantitative relationship between the irrigation rate and color grade was validated through clinical experience, expert consultation, and preliminary tests.
- The entire department received relevant training to learn how to use the rate adjustment card. Before surgery, the responsible nurse educated patients and their families on the color of CBI drainage fluid. It is ok if the color is No. 2 or below, but medical attention is required if the color is No. 3 to No. 6. This education promoted understanding and cooperation while reducing unnecessary anxiety among patients and families.
- The rate adjustment card was compared with CBI drainage under bright light to determine the color grade of the drainage. This comparison was the basis for the rate adjustment according to the rate indicated on the card. In the case of between-grade colors, the higher grade was used (Figures 2,3).
Outcome measures
Incidence of bladder spasm
Bladder spasm was evaluated with the bladder spasm symptom scale, in which the content validity ratio (CVR) was greater than 0.6 for each item. Scoring criteria were as follows: 1 point for postoperative urination urgency, defecation urgency, pain in the bladder area, or catheter blockage due to high pressure in the bladder; 2 points for unbearable pain in the bladder area, urine leakage around the catheter, or backflow of irrigation solution. The highest score is 10, and bladder spasm is diagnosed if the score is 4 or more (13). Incidence of bladder spasm = the number of bladder spasm cases (n)/total number of patients (N) × 100%.
Bleeding
Based on a literature review (10) and our clinical experience, we evaluated bleeding with the incidence of postoperative clot-related catheter blockage, the volume of irrigation solution used, and irrigation time.
- Incidence of clot-related catheter blockage: Significant bleeding at the incision surface may promote clotting in the bladder and subsequent catheter blockage. Therefore, clot-related catheter blockage is an indirect indicator of postoperative bleeding. When the patient complained of a “full” bladder with CBI blockage, the condition was considered clot-related catheter blockage if it could be cleared by squeezing the catheter or by negative suction with a syringe, followed by the observation of clots in the catheter. Incidence of clot-related catheter blockage = the number of clot-related blockage cases (n)/total number of patients (N) × 100%.
- Volume of irrigation solution used: CBI is performed to dilute and drain blood from the bladder. More irrigation solution should be used if the drainage fluid is red. Therefore, the volume of irrigation solution used is an indirect indicator of postoperative bleeding. It was defined as the volume of irrigation solution used (3 L/bag) from the start of CBI to the end of CBI.
- Irrigation time: Clear drainage fluid from CBI indicates that the bleeding at the incision surface has stopped, and CBI may be discontinued. Therefore, irrigation time is a direct indicator of postoperative bleeding time. Irrigation time was defined as the time from the start of CBI to the end of CBI.
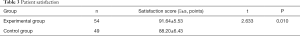
Patient satisfaction
Patient satisfaction was evaluated with the 19-item Newcastle Satisfaction with Nursing Scale (NSNS) (14). The Cronbach’s α of NSNS is 0.96, and the scale can be used for care-specific evaluation of patient satisfaction. The scale is a 5-point scale, where 1 indicates “very dissatisfied” and 5 indicates “very satisfied,” and the total possible score is 19 to 95. A higher score indicates a higher level of patient satisfaction.
Statistical analysis
SPSS 23.0 was used for data analysis. Normally distributed measurement data are expressed as mean ± standard deviation and were analyzed with the t-test. Nonnormally distributed measurement data are expressed as median with interquartile range and were analyzed with Wilcoxon’s rank sum test. Count data are expressed as percentage and rate and were analyzed with the chi-squared test. P<0.05 was considered statistically significant.
Results
Incidence of bladder spasm and bleeding indicators
The incidence of bladder spasm, the incidence of clot-related catheter blockage, the volume of irrigation solution used, and irrigation time were significantly lower or shorter in the experimental group than in the control group (P<0.05) (Table 2).

Full table
Patient satisfaction
Patient satisfaction score was significantly higher in the experimental group than in the control group (P<0.05) (Table 3).
Full table
Discussion
Using the rate adjustment card to effectively reduce the incidence of bladder spasm and improve postoperative bleeding
During CBI, irrigation solution fills the bladder while blood, irrigation solution, and urine were drained from the bladder via a three-lumen catheter. Improper CBI may cause bladder irritation and induce bladder spasm and bleeding (8), which are quite common. According to the literature (10), the incidence of bladder spasm is 15.79% to 55.71%, and the incidence of clot-related catheter blockage is 10.53% to 30.00%. In addition to pain, bladder spasm causes catheter blockage and secondary bleeding at the incision surface, delays postoperative recovery, prolongs hospitalization, and increases medical costs. Bleeding has the same adverse effects. In this study, the incidence of bladder spasm was 28.57% and of clot-related catheter blockage was 22.45% in the control group, which were in line with the literature. High irrigation rates cause mechanical damage to the bladder wall, which increases bladder sensitivity, induces bladder spasm, and even aggravates bleeding. Low irrigation rates can be ineffective and thus lead to inefficient blood drainage from the bladder, which may lead to catheter blockage and then bladder spasm and bleeding. Therefore, proper postoperative irrigation rate helps reduce bladder spasm and bleeding.
Ding et al. (10) developed a wireless sensor-based automated rate adjustment device for post-TURP CBI. In the device, a computer system was used to evaluate the color of drainage fluid and automatically adjust the CBI rate. Their results showed that the device reduced bladder spasm and clot-related catheter blockage relative to the conventional manual method. However, the researchers did not quantify how much to adjust the CBI rate based on the color of the drainage fluid. Moreover, the high cost of the device limited its use. In this study, we quantified the adjustment of the post-TURP CBI rate with a homemade post-TURP CBI rate adjustment card. The results showed that the card reduced the incidence of bladder spasm to 11.11%, which was significantly lower than that in the control group (28.57%). Bleeding indicators were also significantly improved in the experimental group (incidence of clot-related catheter blockage: 7.41% vs. 22.45%; volume of irrigation solution used: 50.66±37.13 vs. 101.55±52.63 L; irrigation time: 46.58±20.01 vs. 63.75±29.65 h). These data indicate that the rate adjustment card reduces postoperative bleeding. Conventional irrigation rates are approximately 120 gtt/min. This study however shows that that rate is too slow and is ineffective in patients with significant bleeding, as it may cause clot-related catheter blockage and subsequent bladder spasm and bleeding and will increase the volume of irrigation solution used and the irrigation time. According to the standard of care, the irrigation rate should be increased if the color of the drainage fluid is dark and decreased if it is light. The color of drainage fluid is a real-time indicator of bleeding, but the evaluation process is different from individual to individual (15,16). This variation may lead to improper adjustment of the irrigation rate, an important cause of bladder spasm and bleeding. In this study, nurses used the rate adjustment card to evaluate the color of drainage fluid and adjust the irrigation rate accordingly in the experimental group, which effectively reduced bladder spasm and postoperative bleeding.
Higher level of patient satisfaction with the rate adjustment card
Patient satisfaction evaluation is a patient-centered evaluation of inpatient experience (17,18). In this study, the homemade post-TURP CBI rate adjustment card significantly improved patient satisfaction. This was likely because the card improved the overall quality of care. Moreover, perioperative patient education on CBI and the use of the rate adjustment card helped answer the patients’ and families’ questions and reduce their anxiety about the color of drainage fluid and irrigation rate adjustments (14). Furthermore, the use of the rate adjustment card standardized the procedures of post-TURP CBI and provided a scientific basis for color evaluation and rate adjustment, which facilitated communication between physicians, nurses, and patients, thereby improving patient satisfaction.
Conclusions
In this study, we evaluated the use of a post-TURP CBI rate adjustment card in patients receiving post-TURP CBI. Its use standardized the procedures of CBI, reduced postoperative CBI-related complications such as bladder spasm and postoperative bleeding, and improved the quality of care. The rate adjustment card is safe, effective, objective, and inexpensive, so it should be used more widely in clinical practice. In the interest of time, this study only enrolled patients receiving post-TURP CBI. Further research is needed to investigate the use of the rate adjustment card in patients receiving CBI for other conditions.
Acknowledgments
The authors gratefully thank Yu-Hua Huang, Li-fen Wu, Chun-Ya Qian, Yu-Hong Zhu, Si-Ni Gu, Qian Yang and Xuan Yao (the Department of Urology, First Affiliated Hospital of Soochow University, Suzhou, China) for their kind help in quality control and data collection.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the TREND reporting checklist. Available at http://dx.doi.org/10.21037/tau-20-1288
Data Sharing Statement: Available at http://dx.doi.org/10.21037/tau-20-1288
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/tau-20-1288). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Each patient signed the informed consent before the study, which was approved by Medical Ethics Committee, First Affiliated Hospital of Soochow University [approval No. (2020) EC 017]. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Blankstein U, Van Asseldonk B, Elterman DS. BPH update: medical versus interventional management. Can J Urol 2016;23:10-5. [PubMed]
- Patel ND, Parsons JK. Epidemiology and etiology of benign prostatic hyperplasia and bladder outlet obstruction. Indian J Urol 2014;30:170-6. [Crossref] [PubMed]
- Stroup SP, Palazzi-Churas K, Kopp RP, et al. Trends in adverse events of benign prostatic hyperplasia (BPH) in the USA, 1998 to 2008. BJU Int 2012;109:84-7. [Crossref] [PubMed]
- Carnevale FC, Iscaife A, Yoshinaga EM, et al. Transurethral Resection of the Prostate (TURP) Versus Original and PErFecTED Prostate Artery Embolization (PAE) Due to Benign Prostatic Hyperplasia (BPH): Preliminary Results of a Single Center, Prospective, Urodynamic-Controlled Analysis. Cardiovasc Intervent Radiol 2016;39:44-52. [Crossref] [PubMed]
- Roehrborn CG, Teplitsky S, Das AK. Aquablation of the prostate: a review and update. Can J Urol 2019;26:20-4. [PubMed]
- Guo RQ, Yu W, Meng YS, et al. A nomogram predicting re-operation due to secondary hemorrhage after monopolar transurethral resection of prostate. Kaohsiung J Med Sci 2018;34:172-8. [Crossref] [PubMed]
- Yates V, Tanner J, Crossley A. Bladder spasm following transurethral surgery. Br J Perioper Nurs 2004;14:259-64. [Crossref] [PubMed]
- Okorie C. Is continuous bladder irrigation after prostate surgery still needed. World J Clin Urol 2015;4:108-14. [Crossref]
- Nojiri Y, Okamura K, Kinukawa T, et al. Continuous bladder irrigation following transurethral resection of the prostate (TURP). Nihon Hinyokika Gakkai Zasshi 2007;98:770-5. [Crossref] [PubMed]
- Ding A, Cao H, Wang L, et al. A novel automatic regulatory device for continuous bladder irrigation based on wireless sensor in patients after transurethral resection of the prostate: A prospective investigation. Medicine (Baltimore) 2016;95:e5721. [Crossref] [PubMed]
- Ng C. Assessment and intervention knowledge of nurses in managing catheter patency in continuous bladder irrigation following TURP. Urol Nurs 2001;21:97-111. [PubMed]
- Ma ZZ, Niu ME. Research Progress on continuous bladder irrigation after transurethral prostatectomy (TURP). J Nurs Sci 2020;35:98-100.
- Baszczuk A, Kopczyński Z, Thielemann A. Endothelial dysfunction in patients with primary hypertension and hyperhomocysteinemia. Postepy Hig Med Dosw (Online) 2014;68:91-100. [Crossref] [PubMed]
- Alasad JA, Ahmad MM. Patients' satisfaction with nursing care in Jordan. Int J Health Care Qual Assur 2003;16:279-85. [Crossref]
- Meagher A, Thompson J, Vanderpuije J. Developing and testing a urine colour reference scale: a practice development project. Int J Urol Nurs 2015;8:122-9. [Crossref]
- Lee JY, Chang JS, Koo KC, et al. Hematuria grading scale: a new tool for gross hematuria. Urology 2013;82:284-9. [Crossref] [PubMed]
- Feldman SF, Lapidus N, Cosnes J, et al. Comparing Inpatient Satisfaction Collected via a Web-Based Questionnaire Self-Completion and Through a Telephone Interview: An Ancillary Study of the SENTIPAT Randomized Controlled Trial. J Med Internet Res 2017;19:e293. [Crossref] [PubMed]
- Li L, Ma Z, Wang W. Influence of transitional care on the self-care ability of kidney transplant recipients after discharge. Ann Palliat Med 2020;9:1958-64. [Crossref] [PubMed]