Management of the devastated posterior urethra and bladder neck: refractory incontinence and stenosis
Introduction
Patients with a devastated posterior urethra and/or bladder neck (BN) typically include those with refractory stenosis, incontinence or both. The devastated outlet can result from neurogenic dysfunction, trauma, or more commonly from complications from prostate cancer therapy. Reconstructive solutions that allow successful restoration of urethral patency and continence are feasible in most neurogenic and external trauma patients. Webster, Turner-Warwick, McAninch and others have widely published their positive experience with reconstruction of the posterior urethra in these patient groups (1-3). This is covered in a separate chapter in this publication. In this review we focus on the devastated outlet that is refractory to reconstruction.
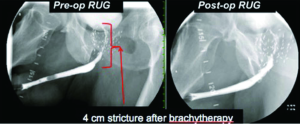
Posterior urethral stenosis (PUS) is an encompassing term that would include bulbomenbranous urethral stricture (BMUS), prostatic urethral stricture, bladder neck contracture (BNC), and patients with vesicourethral anastomotic stricture (VUAS) following radical prostatectomy (RP). The vesicourethral anastomosis (VUA) is the most common site of stenosis after RP, whereas urethral stricture development following RT typically involves the bulbomembranous and anterior urethra (4). In a review of the CapSURE database, the diagnosis of urethral stenosis was identified in 1-8% of patients following treatment of prostate cancer with increased risk present in those receiving prostatectomy or brachytherapy (Figure 1) plus external beam radiotherapy. The majority of post-RP BNC can be successfully treated by well-described techniques such as transurethral incision or dilation (5-7). However, there are a number of patients that require open reconstruction to restore the posterior urethra following complications from prostate cancer therapy. Traditionally open repair has been discouraged, however, more recently our group and others have reported encouraging results with VUA reconstruction due to VUAS following RP. In 2006, Elliot et al. reported successful reconstruction even in the most difficult cases leading to a renewed interest in open repair (8). In 2014, Nikolavsky and Flynn published a single surgeon’s encouraging experience (BJF) of open reconstructions of recalcitrant VUAS following RP in men with a minimum 1-year follow-up (9).
Despite advances in posterior urethral reconstruction, there is a subset of patients who are not candidates for major reconstructive surgery or fail repair and have a devastated outlet. These challenging patients with PUS and incontinence typically have complicating factors such as radiation, fistula and necrosis. These adverse features make successful repair of the posterior urethra less likely resulting in continued obstruction, incontinence and pain. Additionally, there is a subset of patients with refractory urinary incontinence from neurogenic causes and patients with a devastated urethra from multiple AUS erosions. These patients are generally are not amenable to successful anti-incontinence surgery. Unfortunately, the posterior urethra cannot be successfully restored in all patients. For these patients, the goal is simply to resolve incontinence and provide a reliable means of urinary drainage. In this article, we will discuss the role of urethral ligation and BN closure with urinary diversion in patients with a devastated posterior urethra and/or BN due to refractory incontinence and stenosis.
Patient evaluation and decision making
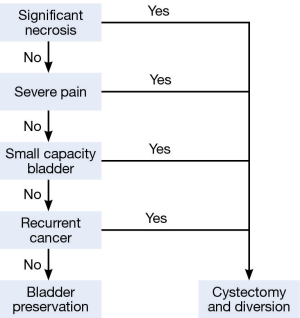
The goal of the patient evaluation and decision-making is to determine if bladder preservation is possible (Figure 2). Patient evaluation begins with a detailed history noting the presence of comorbid conditions including diabetes, steroid usage, performance status, prior radiation, cardiovascular risk factors, and cancer status. Review of the surgical history including prior endoscopic procedures, stenting, and chronic catheterization is important. In patients with >3 failures at endoscopic management of BN stenosis, we advocate for open surgical repair of the proximal urethra when possible. Open repair, covered elsewhere, is technically demanding but at experienced centers has achieved success rates >90% in the absence of prior radiation (4). Physical exam includes examination of the genitalia, perineum, and rectum to evaluate for concomitant fistula, tumor, necrosis and pain. During rectal exam, it is important to assess the prostate and rectal adherence to the prostate as this can aid in decision making if the rectum and prostate are densely adherent. Radiographic examination includes simultaneous antegrade and retrograde urethrography, commonly referred to as the up-and-down o’gram, to demonstrate the length of defect and possible presence of fistula. Similarly, simultaneous cystoscopy can be performed retrograde or antegrade with injection of dye for direct visualization during urethrography. Cystoscopy is important to evaluate for presence of stone, tumor and especially necrosis. Some patients will not tolerate cystoscopy awake and will require exam under anesthesia (EUA). Typically, these patients have a significant amount of necrosis and pain. We have found these patients are not good candidates for reconstruction but rather cystectomy with urinary diversion. Pelvic magnetic resonance imaging (MRI) aids in the evaluation of the rectal-prostatic interface, tumor and peri-vesical cavities. This is useful in estimating risk of rectal injury and the need for flap interposition.
In addition to patient history, physical and imaging, it is important to understand the competency of the sphincter and the bladder capacity. We find urodynamic evaluation is not routinely helpful in patients with severe disease, as catheter placement is not always possible or reliable. However, bladder capacity may be determined by having the patient cap the suprapubic catheter (SPC) and periodically empty while recording output. Assessment of pain during SPC capping is also important to determine if patients would tolerate bladder filling in the future. Additionally, in patients with a SPC, if the BN and sphincter were functional, one would expect the patient to be dry even with capping of the SPC. If this is not the case, if can be reasonable concluded that the sphincter is not adequate.
Finally, a realistic discussion with the patient must occur to overview management options including non-operative, endoscopic, reconstruction and diversion. It is important to extensive counsel patients about the risks and benefits of the surgery and to describe a realistic outcome in order to optimize patient satisfaction.
Non-surgical management
Non-surgical options for incontinence include penile clamp, condom catheter, use of sanitary pad, and fluid restriction. Surprisingly, many of the patients that have severe stricture still have incontinence. In cases of complete outlet obliteration, surgical correction of the outlet would be unnecessary if the patient was content with SPC. This would be a suitable form of treatment, particularly for the frail patient. However, most patients with severe incontinence do not develop obliterative stricture. Therefore, they may require SPC as well as penile clamp in order to empty the bladder and stay dry. There is no medical therapy for this condition. We have not found hyperbaric oxygen useful for patients with stricture and necrosis, despite what some have reported (10).
Surgical management
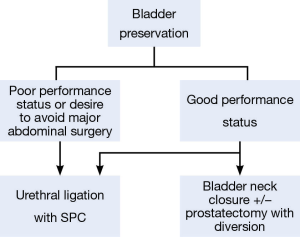
Surgical management should address both the bladder outlet as well as the diversion of urine. These can be managed by a perineal, abdominal, or combined abdomino-perineal approach. We will discuss surgical options for each approach and our algorithm for surgical management for urinary diversion with or without bladder preservation (Figure 3).
Perineal approach
Urethral ligation can be accomplished via a transperineal approach in a select population. In females, BN closure from a transvaginal approach has been well described, however, there are few reports of transperineal urethral ligation in the male population (11,12).
In our experience, transperineal ligation of the urethra is typically reserved for patients with refractory incontinence following prior treatment failure for incontinence. Higuchi et al. reviewed their experience with urethral ligation in six patients with refractory incontinence following SPC placement or urinary diversion. The urethral dissection is carried to the level of the perineal membrane and the urethra is transected near the bulbomembranous junction. The spongiosum is preserved distal to the urethral transection and used as a rotation flap to cover the ligated urethral stump (Figure 4). Additional coverage is obtained with the bulbospongiosus muscle. Five patients had restoration of continence after a single operation with the one failure occurring in a patient with prior radiation for prostate cancer (13). In a separate study, Meeks et al. reported similar success with transperineal urethral ligation of the bulbar urethral in men with a history of neurogenic bladders secondary to myelomeningocele. All four patients included in the review had persistent urinary incontinence following urinary diversion with continent catheterizable channels with three of the patients having had prior BN sling placement with autologous rectus fascia (14). All four patients remained continent at a mean f/u of 49 months.

In our patient population, perineal closure of the urethra is typically reserved for a very small subset of patients with persistent incontinence despite urinary diversion or in those with a devastated urethra who are unwilling or unable to undergo a major abdominal operation.
Abdominal approach
BN closure can be accomplished with or without prostatectomy. Pisters et al. described their method of salvage prostatectomy and BN closure in 13 patients. In addition to prostatectomy and BN closure, concomitant appendico- or ileovesicostomy was utilized for urinary diversion. An omental flap was then mobilized and placed over the site of BN closure. Four of 13 patients required additional operation for wound dehiscence, small bowel anastomotic leak, vesicourethral fistula, and stomal stenosis. The authors recognized the challenging nature of surgical repair in a previously irradiated field and concluded that salvage prostatectomy with BN closure and continent diversion is a reasonable option in this highly selected group (15).
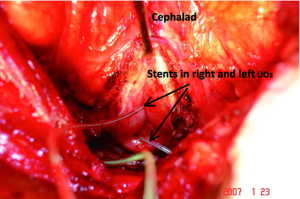
BN closure with or without prostatectomy may also include incorporation of augmentation in efforts to eliminate tension on the closure. Ullrich and Wessells described a method of urinary diversion and BN closure in patients with unsalvageable urethral disease. Following retropubic prostatectomy, the BN is opened transversely in a clamshell fashion while preserving the trigone. The selected segment of bowel is then anastomosed to the bladder and the appendix or ileum is brought to the skin for creation of the continent catheterizable stoma (16). The choice of bowel segment may include large or small bowel. We have found this technique to be useful in those with necrosis of the prostate and BN that requires significant BN debridement (Figure 5). In these patients, direct BN closure is tenuous. Hence, incorporation of the augmented segment is paramount to allow a tension free closure. Additionally, the mesentery of the bowel creates a natural interposition from the BN to the urethral stump avoiding the need for flap insertion. Spahn et al. have advocated for bladder augmentation to be performed in all patients undergoing continent diversion due to devastated outlet. They contend that without augmentation, there is possible loss of bladder capacity during BN closure that can increase the risk of incontinence per stoma (17).
For those not desiring continent diversion, a portion of the ileovesicostomy can be used to close the BN. This is a minor modification of the well described McGuire ileovesicostomy performed primarily in patients with neurogenic bladder (18). We believe this is a reasonable option for the male patient with a devastated outlet.
Finally, cystectomy with urinary diversion may be used and is described by Chrouser et al. in patients with refractory rectourethral fistula and necrosis (19). We believe the same approach may be used in patients without fistula but severe bladder necrosis, contracture, hematuria and pain (Figure 2). In our experience, we have observed that patients with both brachytherapy and XRT frequently have small contracted bladders and are poor candidates for reconstructive procedures. Rather, they are more appropriate for cystectomy and diversion. Patients are consented for both procedures and if necrosis is severe and the bladder is contracted, we elect to remove the bladder and perform supravesical urinary diversion.
Summary
Patients with refractory PUS and devastated outlet, typically following radiation therapy (RT), are a complex group of patients that require a multidisciplinary approach, including reconstructive urology and urologic oncology. Unfortunately not all patients are amenable to definitive urethral reconstruction. Options for the truly devastated urethra and/or outlet range from non-operative management to cystectomy with supravesical diversion. However, there is a subset of patients that have preserved bladder capacity despite severe stricture and prostate necrosis that are appropriate for bladder preservation. In this highly selected group BN closure with diversion allows an intermediary option that would avoid ureteral re-implantation. Additionally, the refractory neurogenic patient with severe incontinence may be suitable for urethral ligation. Timely investigation, careful patient selection, and judicious follow-up are essential to optimize surgical outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Flynn BJ, Delvecchio FC, Webster GD. Perineal repair of pelvic fracture urethral distraction defects: experience in 120 patients during the last 10 years. J Urol 2003;170:1877-80. [PubMed]
- Turner-Warwick R. Urethral stricture surgery. In: Mundy A. eds. Current operative surgery—urology. London: Bailliere Tindall, 1988:160-218.
- Morey AF, McAninch JW. Reconstruction of posterior urethral disruption injuries: outcome analysis in 82 patients. J Urol 1997;157:506-10. [PubMed]
- Mundy AR, Andrich DE. Posterior urethral complications of the treatment of prostate cancer. BJU Int 2012;110:304-25. [PubMed]
- Carr LK, Webster GD. Endoscopic management of the obliterated anastomosis following radical prostatectomy. J Urol 1996;156:70-2. [PubMed]
- Park R, Martin S, Goldberg JD, et al. Anastomotic strictures following radical prostatectomy: insights into incidence, effectiveness of intervention, effect on continence, and factors predisposing to occurrence. Urology 2001;57:742-6. [PubMed]
- Ramirez D, Simhan J, Hudak SJ, et al. Standardized approach for the treatment of refractory bladder neck contractures. Urol Clin North Am 2013;40:371-80. [PubMed]
- Elliott SP, McAninch JW, Chi T, et al. Management of severe urethral complications of prostate cancer therapy. J Urol 2006;176:2508-13. [PubMed]
- Nikolavsky D, Blakely SA, Hadley DA, et al. Open reconstruction of recurrent vesicourethral anastomotic stricture after radical prostatectomy. Int Urol Nephrol 2014;46:2147-52. [PubMed]
- Theodorescu D, Gillenwater JY, Koutrouvelis PG. Prostatourethral-rectal fistula after prostate brachytherapy. Cancer 2000;89:2085-91. [PubMed]
- Rovner ES, Goudelocke CM, Gilchrist A, et al. Transvaginal bladder neck closure with posterior urethral flap for devastated urethra. Urology 2011;78:208-12. [PubMed]
- Zimmern PE, Hadley HR, Leach GE, et al. Transvaginal closure of the bladder neck and placement of a suprapubic catheter for destroyed urethra after long-term indwelling catheterization. J Urol 1985;134:554-7. [PubMed]
- Higuchi T, Yamaguchi Y, Wood H, et al. 238 Transperineal closure of the male urethra in the setting of suprapubic diversion–an alternative management for urinary incontinence. J Urol 2012;187:e98.
- Meeks JJ, Hagerty JA, Chaviano AH. Bulbar urethral ligation for managing persistent urinary incontinence in young men with myelomeningocele. BJU Int 2009;104:221-4. [PubMed]
- Pisters LL, English SF, Scott SM, et al. Salvage prostatectomy with continent catheterizable urinary reconstruction: a novel approach to recurrent prostate cancer after radiation therapy. J Urol 2000;163:1771-4. [PubMed]
- Ullrich NF, Wessells H. A technique of bladder neck closure combining prostatectomy and intestinal interposition for unsalvageable urethral disease. J Urol 2002;167:634-6. [PubMed]
- Spahn M, Kocot A, Loeser A, et al. Last resort in devastated bladder outlet: bladder neck closure and continent vesicostomy--long-term results and comparison of different techniques. Urology 2010;75:1185-92. [PubMed]
- Leng WW, Faerber G, Del Terzo M, et al. Long-term outcome of incontinent ileovesicostomy management of severe lower urinary tract dysfunction. J Urol 1999;161:1803-6. [PubMed]
- Chrouser KL, Leibovich BC, Sweat SD, et al. Urinary fistulas following external radiation or permanent brachytherapy for the treatment of prostate cancer. J Urol 2005;173:1953-7. [PubMed]