Dorsal inlay buccal mucosal graft (Asopa) urethroplasty for anterior urethral stricture
Background and evolution of the Asopa urethroplasty
The Asopa urethroplasty is named after the Indian urologist, Hari Shankar Asopa, who was born on July 7, 1934. He completed his medical and postgraduate education at the Sarojini Maidu Medical College in Agra, India. He is known for several novel techniques in urethral reconstruction, including a one-stage operation for hypospadias using a preputial skin tube (1). He also devised the vascularized double skin island technique (Asopa II) (2). Regarding urethral stricture disease, he invented ‘the dorsal free graft urethroplasty for urethral strictures using ventral sagittal urethrotomy approach’ (3). This has been popularized among reconstructive urologists as the “dorsal inlay” urethroplasty or ‘Asopa’ technique.
In looking at the evolution of urethroplasty, in the 1950s, Sir Denis Browne first described that a buried strip of skin will epithelialize the surrounding tissue into a tube (4). Snodgrass developed a technique in 1994 that involved deep longitudinal incision of the urethral plate, which allowed for tubularization of the urethra without the need for additional flaps for hypospadias repair (5). The key feature to the hypospadias urethral plate is that it is normal, so incising the plate and catheterizing will allow for epithelialization. This is very different from urethral stricture reconstruction, where the plate is scarred and the blood supply compromised, so epithelialization from the edge is typically poor—so incision of the plate alone often fails without an inlay graft (3).
Barbagli introduced the use of dorsally placed onlay grafts in 1998 for urethral stricture reconstruction, suggesting that the corpora provided a superior host bed for underlying support and blood supply for the graft (6). Asopa later described an inlay of a graft into Snodgrass’s longitudinal urethral plate incision using a ventral sagittal urethrotomy approach in 2001. Some colloquially refer to this technique as a ‘Snod-graft’. Asopa stated that this technique was easier to perform and led to less tissue ischemia due to no need for mobilization of the urethra, reporting success rates of 87% (3). Around the same time, Hayes and Malone described a similar approach for use in stenosed hypospadias repair (7).
Asopa urethroplasty technique
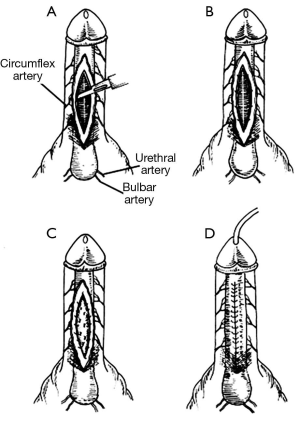
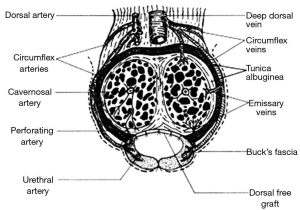
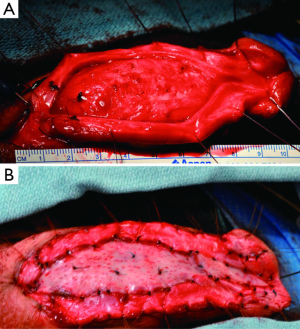
Depending on the location of the stricture, either a subcoronal circumferential incision is made for penile strictures, or a midline perineal incision is made for bulbar strictures. In cases of pan-urethral strictures, both incisions are often made. The penis is then de-gloved and the urethra is split ventrally to exposure the stricture with extension of the incision approximately 1.0-1.5 cm proximally and distally into non-scarred urethra. Through the ventral urethrotomy, the exposed dorsal urethra is incised in the midline down to the tunica. The margins of the incised dorsal urethra are then dissected from the tunica by sharp dissection with the belly of a scalpel—thus creating an elliptical shaped raw area where the graft is placed. Interrupted sutures are used to fix the margins of the graft to the edges of urethra and tunica albuginea. The graft is then quilted in the midline to the underlying corpora with interrupted sutures (Figures 1-3). A 16 Fr Foley catheter is placed and the urethra is retubularized in two layers with special attention to the staggering of suture lines. The skin incision is then closed in multiple layers and a dressing is applied (3). The main advantage of the Asopa technique is that the grafting space is created without lifting the urethral plate halves from the corpora and thus preserves the circumflex and perforating arteries to the spongiosum. The main drawback is that the dorsal augmentation of the Asopa is the graft is less wide than that can be achieved with the Barbagli dorsal technique where the urethral plate is lifted from the corpora.
Types of grafts for dorsal inlay
There are also many variations in the type of graft that can be inlayed using the Asopa technique. Historically, penile skin grafts harvested from the prepuce have been used in dorsal onlay grafts with reasonable success (9). Skin grafts are desirable given the ease of harvest and the large amount of graft that is available if the surgeon considers harvesting from the flank or anterior thigh, rather than only the prepuce. However, outcomes of this technique have been shown to be inferior to buccal mucosal grafting. Thus, the use of buccal mucosa is more widely accepted in contemporary practice, as a more standard of care (10). Oral mucosal grafts are easy to harvest from a well-concealed donor site, have a wet mucosa, are resistant to infection, and provide a thick epithelium, high capillary density, and thin lamina propria. All major advantages to promoting imbibition and graft take (11). Such grafts have a reported long term success rates of up to 87% (3). Oral discomfort and tightness of the mouth are the most reported complications, with very rare reports of peri-oral numbness and motor deficits (12).
Contraindications to oral mucosal grafting, such as oral leukoplakia or prior radiation of the graft sites, can necessitate the use of either skin grafting or newer, less widely accepted techniques (13), such as the use of lip or lingual mucosa, or tissue matrix [small intestinal submucosa (SIS)], tunica vaginalis, or postauricular skin (14,15). SIS is desirable as an off the shelf product, but success rates have been very mixed, with short follow up (16). Lip or lingual mucosa is quite easy to harvest, but there is limited availability of tissue and donor site morbidity is higher than with buccal site harvesting—especially when long grafts are harvested (17). Lingual grafts are often thinner in width and depth (usually 1-1.5 cm at best in width), and rather flimsy compared to buccal grafts. Tunica vaginalis and postauricular skin grafts show promise but there is currently limited data and short follow up (18).
Double overlapping oral grafts
Since the inception of the dorsal inlay graft, several variations in technique have been described. Palminteri and colleagues reported that in addition to placement of a dorsal inlay buccal mucosal graft (BMG) via a ventral sagittal approach (Asopa), a ventral onlay buccal graft could be added as well (Figure 4). Following dorsal augmentation, the urethra is grafted ventrally with another buccal graft, and then covered with the thick ventral spongiosum, as a “spongioplasty”. The main role for double dorsal-ventral grafting is for tight strictures, with a narrow urethral plate, such that a single graft would be insufficient to reconstructing a urethral lumen of reasonable diameter. Potential post-operative sexual side effects are theoretically avoided by not transecting the urethra and preserving the urethral plate and vascularity. Palminteri reported success rates of up to 90% in medium length strictures (14,20,21). Most recently, Chen et al. described the use of a BMG ventral onlay with dorsal full-thickness skin graft inlay urethroplasty to treat strictures greater than 4 cm in length. The skin grafting was used due to limited supply of buccal mucosa available to repair longer strictures. This technique was found to have higher failure rates than double BMGs in shorter strictures, but was felt to be optimal in strictures over 6 cm in length (22).

Treatment algorithm for inlay grafting
An important question to ask is when to perform an Asopa urethroplasty? As mentioned earlier, it is a technique that is used on the anterior urethra (specifically the penile urethra). Options to repair a penile urethral stricture include the Asopa (dorsal inlay urethroplasty), the Barbagli (dorsal onlay urethroplasty), ventral onlay urethroplasty, as well as several staged techniques. Each technique has advantages and disadvantages and the superiority of one approach over another has yet to be clearly defined.
In our experience, the key to when to use the dorsal inlay technique all depends on the width of the urethral plate once the urethrotomy is performed, stricture etiology, and stricture location (penile vs. bulb). We have found that it is best to perform an Asopa urethroplasty when the urethral plate is ≥1 cm in width. When a graft that is 2 cm wide is combined with a urethral plate that is 1 cm wide and the edges are tubularized, a urethral lumen of approximately 24 Fr will be obtained. If the urethral plate is <1 cm in width, a lumen of less than 24 Fr will be obtained. It is nearly impossible to perform an Asopa if the plate is <5 mm wide, since there are no remaining edges to sew to. One way to estimate this preoperatively is by checking to see if the urethral lumen will accommodate an ureteroscope or a pediatric cystoscope. If not, then the urethral lumen is <10 Fr, and depending on stricture length, a double grafting technique, anastomotic or staged urethroplasty should be considered.
Aldaqadossi et al. conducted a prospective randomized trial of 47 patients that compared the dorsal onlay technique of Barbagli and the dorsal inlay technique of Asopa. During their follow-up period, they observed an overall success rate of 88% in the dorsal onlay group and 86.4% success rate in the dorsal inlay group. The two main differences were operative time (205±19.6 vs. 128±4.9 min, P<0.0001) and estimated blood loss (228±5.3 vs. 105±12.0 mL), respectively. They concluded that dorsal onlay and dorsal inlay urethroplasty techniques provide similar success rates, but the Asopa technique is easier to perform, provides a shorter operative time and less blood loss (23). In their editorial comment, Tausch and Morey point out that this is most likely because the Barbagli technique requires more extensive urethral mobilization which can be more time consuming and complicated by spongiofibrosis and corporal adhesions (24). In a similar study, Pahwa et al. randomized 40 patients to undergo either a dorsal onlay BMG urethroplasty vs. a dorsal BMG urethroplasty by ventral urethrotomy. They found that there was no statistically significant difference in final outcome using either method (25). For bulbar urethral strictures, Barbagli et al. found that the placing the BMG on the dorsal, ventral, or lateral surface of the bulbar urethra yielded similar success rates (26).
Wang et al. sought to compare outcomes of dorsal vs. ventral onlay urethroplasty for anterior urethral strictures by conducting a meta-analysis that included 1,263 cases published in 49 studies. They found that the success rates of ventral onlay urethroplasty (750 cases) was 82.5% and that of dorsal onlay urethroplasties (513 cases) was 86.9% (P=0.034). BMG had the highest rate of success and rates were similar between both dorsal and ventral groups (89.2% vs. 87.6%, P=0.472). The dorsal onlay success rate was higher than ventral for the free skin graft technique (84.7% vs. 74.7%, P=0.016). They also found that bulbar urethral stricture repair had an overall higher success rate when compared to penile urethral repairs (87.4% vs. 77.6%, P=0.019) (27).
Pisapati et al. reported an 87% success rate using the Asopa technique with a mean follow-up period of 42 months (28). Selecting when to perform the Asopa technique is an essential key to success. In his editorial comment, Barbagli states that if the urethral plate is too narrow, the midline incision of the plate will damage the urethral mucosa. In this scenario, it is better to perform a dorsal onlay graft. He reports that the dorsal onlay technique usually widens the original urethral plate by 2.5 cm whereas the dorsal inlay technique only provides 1.5 cm widening of the original urethral plate. This is particularly important in patients with lichen sclerosus who have a high stricture recurrence rate. Therefore, the decision to perform a dorsal inlay vs. dorsal onlay should be driven by stricture etiology and width of the original urethral plate (29).
Conclusions
The dorsal inlay urethroplasty also known as the ventral sagittal urethrotomy approach for dorsal free graft urethroplasty (Asopa) can be utilized to repair long and multiple anterior urethral strictures. Depending on the location of the stricture, the approach utilized can be a circumferential or non-circumferential penile incision, a penoscrotal incision, or a perineal incision. The main difference between the Asopa (dorsal inlay technique) and the Barbagli (dorsal onlay technique) is that the Asopa technique preserves the blood supply to the urethral plate (circumflex and perforating arteries) since the urethral plate halves are not dissected off the corpora. If the urethral plate is too narrow (i.e., less than 1 cm), it is better to perform another approach such as the Barbagli (dorsal onlay technique) to help widen the urethral plate. The decision to perform a dorsal inlay vs. onlay should be driven by the width of the urethral plate, stricture location, and stricture etiology.
Acknowledgements
None.
Footnote
Conflicts of Interest: Steven B. Brandes declares conflict of interest with Allergan (investigator), American Medical Systems (lecturer). Stephen D. Marshall and Valary T. Raup have no conflicts of interest to declare.
References
- Asopa HS, Elhence IP, Atri SP, et al. One stage correction of penile hypospadias using a foreskin tube. A preliminary report. Int Surg 1971;55:435-40. [PubMed]
- Asopa R, Asopa HS. One stage repair of hypospadias using double island preputial skin tube. Indian J Urol 1984;1:41-3.
- Asopa HS, Garg M, Singhal GG, et al. Dorsal free graft urethroplasty for urethral stricture by ventral sagittal urethrotomy approach. Urology 2001;58:657-9. [PubMed]
- Patel SR, Caldamone AA. Sir Denis Browne: contributions to pediatric urology. J Pediatr Urol 2010;6:496-500. [PubMed]
- Snodgrass W. Tubularized, incised plate urethroplasty for distal hypospadias. J Urol 1994;151:464-5. [PubMed]
- Barbagli G, Palminteri E, Rizzo M. Dorsal onlay graft urethroplasty using penile skin or buccal mucosa in adult bulbourethral strictures. J Urol 1998;160:1307-9. [PubMed]
- Hayes MC, Malone PS. The use of a dorsal buccal mucosal graft with urethral plate incision (Snodgrass) for hypospadias salvage. BJU Int 1999;83:508-9. [PubMed]
- McClung C, Wessells H. Staged Urethroplasty. In: Brandes SB, Morey AF. eds. Advanced Male Urethral and Genital Reconstructive Surgery. 2nd ed. New York: Humana Press, 2014:289-303.
- Barbagli G, Palminteri E, Lazzeri M, et al. Interim outcomes of dorsal skin graft bulbar urethroplasty. J Urol 2004;172:1365-7; discussion 1367. [PubMed]
- Bhargava S, Chapple CR. Buccal mucosal urethroplasty: is it the new gold standard? BJU Int 2004;93:1191-3. [PubMed]
- Song LJ, Xu YM, Lazzeri M, et al. Lingual mucosal grafts for anterior urethroplasty: a review. BJU Int 2009;104:1052-6. [PubMed]
- Castagnetti M, Ghirardo V, Capizzi A, et al. Donor site outcome after oral mucosa harvest for urethroplasty in children and adults. J Urol 2008;180:2624-8. [PubMed]
- Dalpiaz O, Kerschbaumer A, Pelzer A, et al. Single-stage dorsal inlay split-skin graft for salvage anterior urethral reconstruction. BJU Int 2008;101:1565-70. [PubMed]
- Chapple C, Andrich D, Atala A, et al. SIU/ICUD Consultation on Urethral Strictures: The management of anterior urethral stricture disease using substitution urethroplasty. Urology 2014;83:S31-47. [PubMed]
- Mangera A, Patterson JM, Chapple CR. A systematic review of graft augmentation urethroplasty techniques for the treatment of anterior urethral strictures. Eur Urol 2011;59:797-814. [PubMed]
- Palminteri E, Berdondini E, Colombo F, et al. Small intestinal submucosa (SIS) graft urethroplasty: short-term results. Eur Urol 2007;51:1695-701; discussion 1701.
- Barbagli G, De Angelis M, Romano G, et al. The use of lingual mucosal graft in adult anterior urethroplasty: surgical steps and short-term outcome. Eur Urol 2008;54:671-6. [PubMed]
- Foinquinos RC, Calado AA, Janio R, et al. The tunica vaginalis dorsal graft urethroplasty: initial experience. Int Braz J Urol 2007;33:523-9; discussion 529-31. [PubMed]
- Palminteri E, Berdondini E. Double Overlapping Buccal Grafts. In: Brandes SB, Morey AF. eds. Advanced Male Urethral and Genital Reconstructive Surgery. 2nd ed. New York: Humana Press, 2014:469-79.
- Palminteri E, Manzoni G, Berdondini E, et al. Combined dorsal plus ventral double buccal mucosa graft in bulbar urethral reconstruction. Eur Urol 2008;53:81-9. [PubMed]
- Palminteri E, Berdondini E, Shokeir AA, et al. Two-sided bulbar urethroplasty using dorsal plus ventral oral graft: urinary and sexual outcomes of a new technique. J Urol 2011;185:1766-71. [PubMed]
- Chen ML, Odom BD, Johnson LJ, et al. Combining ventral buccal mucosal graft onlay and dorsal full thickness skin graft inlay decreases failure rates in long bulbar strictures (≥6 cm). Urology 2013;81:899-902. [PubMed]
- Aldaqadossi H, El Gamal S, El-Nadey M, et al. Dorsal onlay (Barbagli technique) versus dorsal inlay (Asopa technique) buccal mucosal graft urethroplasty for anterior urethral stricture: a prospective randomized study. Int J Urol 2014;21:185-8. [PubMed]
- Tausch TJ, Morey AF. Editorial comment to Dorsal onlay (Barbagli technique) versus dorsal inlay (Asopa technique) buccal mucosal graft urethroplasty for anterior urethral stricture: a prospective randomized study. Int J Urol 2014;21:189. [PubMed]
- Pahwa M, Gupta S, Pahwa M, et al. A comparative study of dorsal buccal mucosa graft substitution urethroplasty by dorsal urethrotomy approach versus ventral sagittal urethrotomy approach. Adv Urol 2013;2013:124836.
- Barbagli G, Palminteri E, Guazzoni G, et al. Bulbar urethroplasty using buccal mucosa grafts placed on the ventral, dorsal or lateral surface of the urethra: are results affected by the surgical technique? J Urol 2005;174:955-7; discussion 957-8. [PubMed]
- Wang K, Miao X, Wang L, et al. Dorsal onlay versus ventral onlay urethroplasty for anterior urethral stricture: a meta-analysis. Urol Int 2009;83:342-8. [PubMed]
- Pisapati VL, Paturi S, Bethu S, et al. Dorsal buccal mucosal graft urethroplasty for anterior urethral stricture by Asopa technique. Eur Urol 2009;56:201-5. [PubMed]
- Barbagli G. Editorial comment on: Dorsal buccal mucosal graft urethroplasty for anterior urethral stricture by Asopa technique. Eur Urol 2009;56:205-6. [PubMed]


