Pro: endoscopic realignment for pelvic fracture urethral injuries
Background
In patients with pelvic fracture urethral distraction injury, there are two basic methods of early treatment. The first is early realignment over a catheter, usually using gentle blind or endoscopic techniques. The second is placement of a suprapubic tube, and subsequent open urethroplasty after the nearly inevitable urethral stenosis forms.
The benefits of early realignment over a catheter are potentially many. It is generally simple, avoids the need for placement of a suprapubic catheter, may decrease the overall impact of the urethral injury by promoting earlier return to spontaneous voiding, and may decrease the chance and degree of subsequent urethral obliteration.
Realignment method
There are several methods to place a urethral catheter into the bladder across a disrupted urethra. Most experts start with a simple retrograde catheterization attempt (1-3). If this fails, most modern authors choose retrograde flexible cystoscopy next (4,5). Retrograde flexible or rigid urethroscopy through a suprapubic tube can be attempted next (6). This procedure is claimed to require only 5-10 minutes when successful (5,6), while retrograde rigid cystoscopy has been reported to require an average of 22 minutes (7). If this fails, other authors have used two cystoscopes: one rigid one placed anterograde and a second flexible scope placed retrograde to bridge the gap (8,9).
Despite many documented techniques for realignment, our preferred stepwise approach is a single attempt at gentle blind passage of a catheter followed by retrograde flexible cystoscopy then rigid cystoscopy then suprapubic flexible cystoscopy (with or without simultaneous rigid cystoscopy).
Other techniques described involve placing a wire placed anterograde or retrograde across the defect and then placing a Council-tipped Foley catheter over the wire (10) or using a feeding tube placed in the penis which is placed into the bladder and grasped through a cystotomy (11). Direct placement of a Foley catheter anterograde through a cystostomy (1) or urethral cystoscopy towards a Goodwin sound placed through a cystostomy has also been described (12). Two blindly-placed anterograde and retrograde catheters with strong magnets on the end have been used to safely traverse the defect, but unfortunately these catheters are not commercially available (13). Older reports generally report open techniques using Davis interlocking sounds (2) or a metal sound in the urethra guided by a finger in the bladder neck (14), requiring a mean of 80 minutes to complete in one 1,983 study (2). A technique using anterograde or retrograde placement of catheters required less than 75 minutes (1).
Immediate procedural success of realignment and timing of attempts
The published procedural success rate of any realignment technique is variable depending on the author, and ranges from 70-100% (4,13-18). One series where authors gained experience in the technique over a 5 year period showed an increase in successful realignment rates from 80% up to 93% with time (7).
Most surgeons place the catheter as soon as practically possible (10) and this is generally achievable after a mean of 32 hours from injury (10). A single immediate blind placement of a Foley catheter is attempted at most centers soon after the injury is diagnosed (10). Some have delayed realignment up to 7-19 days (11) with good results. Authors have suggested that after initial failure, realignment can be attempted 2-3 days later with some success (4). A single report of a small number of early (72 hours) and more delayed realignment cases were compared and had similar rates of subsequent stenosis (9).
The recommended time that the catheter should be left in is highly variable, ranging from 3-6 weeks (2,4,10-13,19,20) with some recommend longer catheterization up to 8 weeks (9,19). We leave the catheter 6 weeks before voiding cystourethrogram or peri-catheter retrograde urethrogram is attempted. If there is no extravasation the Foley catheter is removed. If a suprapubic tube is also present, it is capped but left in place for at least 4 weeks to ensure there is no interim stenosis prior to removal.
Incidence of stenosis
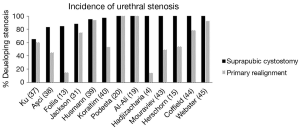
Long term success of realignment is most importantly defined by the incidence of subsequent urethral stenosis; however, stenosis outcomes and the screening and diagnoses of urethral stenosis have been variable. A review of the literature demonstrated a wide rate of stenosis among series of patients undergoing realignment ranging from 14-100%; however, realignment appears to be associated with a lower chance of subsequent urethral obliteration by about 40% when compared to placement of a suprapubic tube alone (Table 1) (Figure 1). These findings are consistent with a recent meta-analysis of studies comparing primary realignment to cystostomy, in which, the authors report a significantly lower rate of stenosis among the primary alignment group with an absolute risk reduction of 37% (46).
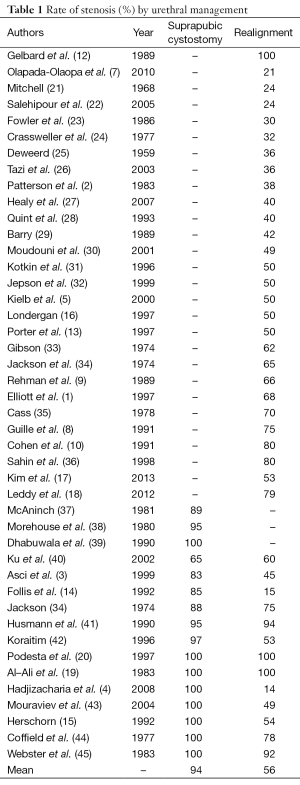
Full table
In a recent case series of 19 patients undergoing primary endoscopic realignment, the authors report a failure rate of 79%, but of those failures three only required a single urethrotomy such that only 58% of the cohort went on to require urethroplasty (18). While we do not advocate for management with repetitive urethrotomies, these data imply that realignment allows for a less severe stenosis in some patients.
Time to voiding and length of stenosis
In one series, the patients who underwent realignment had a significantly shorter time to spontaneous voiding (35 vs. 229 days) than those who had cystostomy (4).
Furthermore, some authors have suggested that realignment also aligns the urethral ends so that any subsequent urethroplasty is technically easier (6). While there is not much evidence to support claims of less severe stenosis, one series did find significantly shorter stenoses among the cohort treated with early realignment as compared to cystostomy (42).
Complications of realignment
While most authors report good results from endoscopic realignment, some studies suggest that they decrease the success of any future urethroplasty. A report of 7 patients reported that in those that required urethroplasty, it was 1/2 as successful (43% for realigned group vs. 85% for uninstrumented group); however, this trend has not been demonstrated in other series. The authors hypothesized that endoscopic realignment causes inflammation and then fibrosis of the torn ends of the urethra, although no proof for this is given (47).
Confirmed early complications from endoscopic realignment are rare and sporadic. Most series that actually analyzed complications report no significant complications from the procedure (1). Attempting and failing to get realignment with a catheter is not believed to harm the patient (14). One series report a 1/34 (3%) incidence of pelvic abscess (2). A single urethro scrotal fistula appeared in a series of 14 (7%) realigned patients (10) and a perineal abscess developed in 1/6 (16%) and1/4 (35%) patients in other studies (22,23). Malposition of the catheter (including inadvertently “jumping” the catheter over the prostate and placing into the bladder via a bladder rupture) is a rare possibility and has been personally witnessed by the authors. Delayed realignment at a mean of 10 days caused septicemia in 15% of cases in one series (7) prompting us to avoid late attempts at realignment.
One series has reported that realignment was associated with increased need for multiple endoscopic procedures (48). Algorithmic approaches to any urethral stenosis/stricture patients should take into account the high likelihood of failure with repeated endoscopic procedures. As urethral disruption is associated with a high rate of stenosis, close follow-up after realignment is essential. If treated with a similar algorithm to any other urethral stenosis/stricture, that is, timely transition to urethroplasty after failed endoscopic management, there should not be a need for multiple interventions among urethral stenosis after realignment.
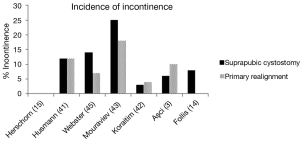
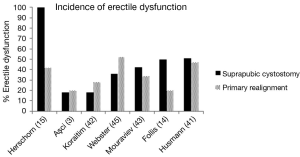
Erectile dysfunction and incontinence have been commonly reported following urethral distraction injuries; however, primary realignment does not appear to increase the baseline incontinence or erectile dysfunction rate (Tables 2,3). Variation seen in a variety of series with regard to erectile dysfunction and continence likely reflects the diversity of the initial injury rather than the method of urethral management (Figures 2,3).
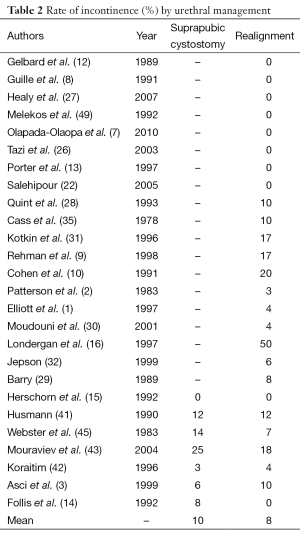
Full table
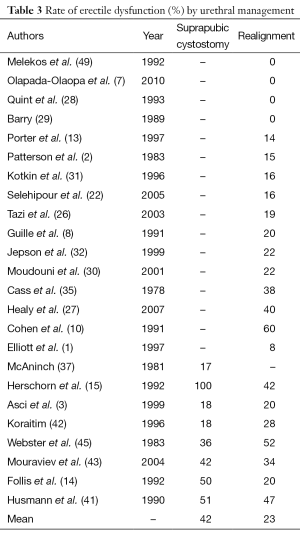
Full table
Limitations
Almost all reports used different methods of achieving urethral alignment, making direct comparisons difficult. Outcomes from old reports describing open, often highly invasive, techniques (e.g., removing hematoma or cutting the puboprostatic ligaments) cannot be properly compared to modern endoscopic techniques.
It is also possible that patients in whom realignment is possible may have less serious injuries that those in which it fails. In some series the patients managed with suprapubic cystostomy had previously failed alignment attempts, and these patients probably have more significant injuries and longer urethral distraction distances than those in whom alignment was successful. One report of 16 patients determined that partial urethral tears as determined by urethrography were present in 33% of those in whom realignment was not possible and 46% of those in whom realignment was possible (15). The incidence of partial versus total urethral disruption found partial injuries to be much more common in the cystostomy group (7%) than the alignment group (39%) (15).
Conclusions
Review of over thirty studies, including at least a dozen that directly compare realignment to suprapubic diversion along, conclude that there is a benefit averaging at least 35% in favor of realignment. Secondary benefits of realignment may include easier subsequent urethroplasty, when necessary, and possibly shorter stenoses. Endoscopic realignment is not associated with a higher rate of immediate or delayed complications. While the rate of subsequent urethral stenosis after realignment remains high, the potential to eliminate the need for complicated urethroplasty in up to a third of patients cannot be ignored.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Elliott DS, Barrett DM. Long-term followup and evaluation of primary realignment of posterior urethral disruptions. J Urol 1997;157:814-6. [PubMed]
- Patterson DE, Barrett DM, Myers RP, et al. Primary realignment of posterior urethral injuries. J Urol 1983;129:513-6. [PubMed]
- Aşci R, Sarikaya S, Büyükalpelli R, et al. Voiding and sexual dysfunctions after pelvic fracture urethral injuries treated with either initial cystostomy and delayed urethroplasty or immediate primary urethral realignment. Scand J Urol Nephrol 1999;33:228-33. [PubMed]
- Hadjizacharia P, Inaba K, Teixeira PG, et al. Evaluation of immediate endoscopic realignment as a treatment modality for traumatic urethral injuries. J Trauma 2008;64:1443-9; discussion 1449-50. [PubMed]
- Kielb SJ, Voeltz ZL, Wolf JS. Evaluation and management of traumatic posterior urethral disruption with flexible cystourethroscopy. J Trauma 2001;50:36-40. [PubMed]
- Gheiler EL, Frontera JR. Immediate primary realignment of prostatomembranous urethral disruptions using endourologic techniques. Urology 1997;49:596-9. [PubMed]
- Olapade-Olaopa EO, Atalabi OM, Adekanye AO, et al. Early endoscopic realignment of traumatic anterior and posterior urethral disruptions under caudal anaesthesia - a 5-year review. Int J Clin Pract 2010;64:6-12. [PubMed]
- Guillé F, Cippola B, el Khader K, et al. Early endoscopic realignment for complete traumatic rupture of the posterior urethra--21 patients. Acta Urol Belg 1998;66:55-8. [PubMed]
- Rehman J, Samadi D, Ricciardi R Jr, et al. Early endoscopic realignment as primary therapy for complete posterior urethral disruptions. J Endourol 1998;12:283-9. [PubMed]
- Cohen JK, Berg G, Carl GH, et al. Primary endoscopic realignment following posterior urethral disruption. J Urol 1991;146:1548-50. [PubMed]
- Balkan E, Kilic N, Dogruyol H. The effectiveness of early primary realignment in children with posterior urethral injury. Int J Urol 2005;12:62-6. [PubMed]
- Gelbard MK, Heyman AM, Weintraub P. A technique for immediate realignment and catheterization of the disrupted prostatomembranous urethra. J Urol 1989;142:52-5. [PubMed]
- Porter JR, Takayama TK, Defalco AJ. Traumatic posterior urethral injury and early realignment using magnetic urethral catheters. J Urol 1997;158:425-30. [PubMed]
- Follis HW, Koch MO, McDougal WS. Immediate management of prostatomembranous urethral disruptions. J Urol 1992;147:1259-62. [PubMed]
- Herschorn S, Thijssen A, Radomski SB. The value of immediate or early catheterization of the traumatized posterior urethra. J Urol 1992;148:1428-31. [PubMed]
- Londergan TA, Gundersen LH, van Every MJ. Early fluoroscopic realignment for traumatic urethral injuries. Urology 1997;49:101-3. [PubMed]
- Kim FJ, Pompeo A, Sehrt D, et al. Early effectiveness of endoscopic posterior urethra primary alignment. J Trauma Acute Care Surg 2013;75:189-94. [PubMed]
- Leddy LS, Vanni AJ, Wessells H, et al. Outcomes of endoscopic realignment of pelvic fracture associated urethral injuries at a level 1 trauma center. J Urol 2012;188:174-8. [PubMed]
- Al-Ali IH, Husain I. Disrupting injuries of the membranous urethra--the case for early surgery and catheter splinting. Br J Urol 1983;55:716-20. [PubMed]
- Podestá ML, Medel R, Castera R, et al. Immediate management of posterior urethral disruptions due to pelvic fracture: therapeutic alternatives. J Urol 1997;157:1444-8. [PubMed]
- Mitchell JP. Trauma to the urethra. Injury 1975;7:84-8. [PubMed]
- Salehipour M, Khezri A, Askari R, et al. Primary realignment of posterior urethral rupture. Urol J 2005;2:211-5. [PubMed]
- Fowler JW, Watson G, Smith MF, et al. Diagnosis and treatment of posterior urethral injury. Br J Urol 1986;58:167-73. [PubMed]
- Crassweller PO, Farrow GA, Robson CJ, et al. Traumatic rupture of the supramembranous urethra. J Urol 1977;118:770-1. [PubMed]
- Deweerd JH. Management of injuries to the bladder, urethra and genitalia. Surg Clin North Am 1959;39:973-87. [PubMed]
- Tazi H, Ouali M, Lrhorfi MH, et al. Endoscopic realignment for post-traumatic rupture of posterior urethra. Prog Urol 2003;13:1345-50. [PubMed]
- Healy CE, Leonard DS, Cahill R, et al. Primary endourologic realignment of complete posterior urethral disruption. Ir Med J 2007;100:488-9. [PubMed]
- Quint HJ, Stanisic TH. Above and below delayed endoscopic treatment of traumatic posterior urethral disruptions. J Urol 1993;149:484-7. [PubMed]
- Barry JM. Visual urethrotomy in the management of the obliterated membranous urethra. Urol Clin North Am 1989;16:319-24. [PubMed]
- Moudouni SM, Patard JJ, Manunta A, et al. Early endoscopic realignment of post-traumatic posterior urethral disruption. Urology 2001;57:628-32. [PubMed]
- Kotkin L, Koch MO. Impotence and incontinence after immediate realignment of posterior urethral trauma: result of injury or management? J Urol 1996;155:1600-3. [PubMed]
- Jepson BR, Boullier JA, Moore RG, et al. Traumatic posterior urethral injury and early primary endoscopic realignment: evaluation of long-term follow-up. Urology 1999;53:1205-10. [PubMed]
- Gibson GR. Urological management and complications of fractured pelvis and ruptured urethra. J Urol 1974;111:353-5. [PubMed]
- Jackson DH, Williams JL. Urethral injury: a retrospective study. Br J Urol 1974;46:665-76. [PubMed]
- Cass AS, Godec CJ. Urethral injury due to external trauma. Urology 1978;11:607-11. [PubMed]
- Sahin H, Bircan MK, Akay AF, et al. Endoscopic treatment of complete posterior urethral obliteration. Acta Urol Belg 1998;66:21-4. [PubMed]
- McAninch JW. Traumatic injuries to the urethra. J Trauma 1981;21:291-7. [PubMed]
- Morehouse DD, Belitsky P, Mackinnon K. Rupture of the posterior urethra. J Urol 1972;107:255-8. [PubMed]
- Dhabuwala CB, Hamid S, Katsikas DM, et al. Impotence following delayed repair of prostatomembranous urethral disruption. J Urol 1990;144:677-8. [PubMed]
- Ku JH, Jeon YS, Kim ME, et al. Comparison of long-term results according to the primary mode of management and type of injury for posterior urethral injuries. Urol Int 2002;69:227-32. [PubMed]
- Husmann DA, Wilson WT, Boone TB, et al. Prostatomembranous urethral disruptions: management by suprapubic cystostomy and delayed urethroplasty. J Urol 1990;144:76-8. [PubMed]
- Koraitim MM. Pelvic fracture urethral injuries: evaluation of various methods of management. J Urol 1996;156:1288-91. [PubMed]
- Mouraviev VB, Coburn M, Santucci RA. The treatment of posterior urethral disruption associated with pelvic fractures: comparative experience of early realignment versus delayed urethroplasty. J Urol 2005;173:873-6. [PubMed]
- Coffield KS, Weems WL. Experience with management of posterior urethral injury associated with pelvic fracture. J Urol 1977;117:722-4. [PubMed]
- Webster GD, Mathes GL, Selli C. Prostatomembranous urethral injuries: a review of the literature and a rational approach to their management. J Urol 1983;130:898-902. [PubMed]
- Barrett K, Braga LH, Farrokhyar F, et al. Primary realignment vs suprapubic cystostomy for the management of pelvic fracture-associated urethral injuries: a systematic review and meta-analysis. Urology 2014;83:924-9. [PubMed]
- Singh BP, Andankar MG, Swain SK, et al. Impact of prior urethral manipulation on outcome of anastomotic urethroplasty for post-traumatic urethral stricture. Urology 2010;75:179-82. [PubMed]
- Tausch TJ, Morey AF, Scott JF, et al. Unintended negative consequences of primary endoscopic realignment for men with pelvic fracture urethral injuries. J Urol 2014;192:1720-4. [PubMed]
- Melekos MD, Pantazakos A, Daouaher H, et al. Primary endourologic re-establishment of urethral continuity after disruption of prostatomembranous urethra. Urology 1992;39:135-8. [PubMed]