Hormonal therapy and chemotherapy in hormone-naive and castration resistant prostate cancer
Introduction
Prostate cancer is the most common tumor in men in industrialized countries and the second cause of death in this population (1). Since the seminal work of Huggins in 1940, castration obtained with androgen deprivation therapy (ADT) has remained the cornerstone of treatment for patients with prostate cancer (2).
ADT comprising orchiectomy or a luteinising hormone-releasing hormone (LHRH) agonist or antagonist, with or without an antiandrogen, is the first line of treatment for men with metastatic prostate cancer (3,4).
ADT is capable of achieving castrate levels of testosterone (≤50 ng/dL), and most patients with metastatic hormone naive prostate cancer initially respond to this treatment, with both tumor and biochemical responses (5). However, the majority of patients will develop resistance to these traditional hormonal approaches and the median time to progression is about 18-24 months (3).
More than 20-40% of prostate tumors that progress on first line ADT may respond to second- and third-line hormonal treatments, suggesting the importance of androgen receptor (AR) signaling in the pathogenesis of prostate cancer (3-7).
AR signaling plays a central role in the biology of prostate cancer and it is necessary for the proliferation and survival of prostate cancer cells (8). The AR is a cytoplasmatic steroid receptor that binds specific ligands, the androgens. Androgenic steroids are the most important AR agonists including testosterone, dehydroepiandrosterone, androstenediol and androstenedione. Testosterone is the major circulating androgen and 90-95% is synthesized in the leydig cells of the testis, while 5-10% is derived from the adrenal glands. In prostate cells, the enzyme 5alfa-reductase converts testosterone to the active hormone, dehydrotestosterone, which binds the AR (9).
In the absence of androgens, the AR is bound to heat-shock proteins and remains primarily in the cytoplasm. Upon activation by androgens, the AR dissociates from heat-shock proteins and translocates into the nucleus, where it binds with co-activators and corepressors to androgen-response elements in the promoter regions of genes to activate their transcription. This interaction determines activation or repression of genes regulating development, differentiation and proliferation of cells (10).
There is increasing preclinical and clinical evidence that the AR remains active in castration resistant prostate cancer (CRPC). The persistence of AR signaling is key to prostate cancer progression and the AR represents the most important therapeutic target in the treatment of this disease, both in hormone sensitive and in castration resistant disease (11-13). The AR binds androgens activating specific DNA sequences with the transcription of androgen correlated genes determining the physiological effects of androgens.
The aim of this review is to summarize the current knowledge concerning both hormonal therapy and chemotherapy in hormone naive and CRPC patients.
Hormonal therapy and chemotherapy in hormone naive patients
Chemotherapy treatment with taxanes is known to improve survival in metastatic disease in prostate cancer (14,15). Under investigation is whether the addition of hormonal therapies and chemotherapy to local treatments with radiotherapy or surgery, could improve outcomes in the management of high-risk localized prostate cancer.
Hormone chemotherapy in localized disease
High risk prostate cancer is a potentially lethal disease accounting for approximately 15% of all new diagnoses. Despite local treatments, one third of patients with high risk prostate cancer can experience a recurrence of disease and death from prostate cancer (16,17).
Even though the definition of high risk varies widely, the most significant validated predictive factors of disease relapse are clinical tumor stage, PSA level, Gleason score of the diagnostic biopsy specimen and nodal status (18-20).
There is growing interest in a multimodal approach to high risk localized prostate cancer combining local and systemic therapies and in this context chemotherapy may play an important role in disease control. Specifically, the benefit in overall survival in metastatic prostate cancer, has led to evaluation of the use of docetaxel in early stages of disease.
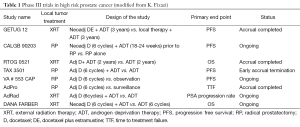
Multiple phase III trials are ongoing to investigate the impact of chemotherapy in the neoadjuvant and adjuvant settings of prostate cancer with or without hormonal therapy. Long term follow-up is required to assess the outcome of patients with localized prostate cancer and just a few of these trials have completed their planned accrual. We report the most important trials investigating the role of docetaxel in the neoadjuvant and adjuvant settings. Additional details about these trials are shown in Table 1.
Full table
Neoadjuvant trials
The use of neoadjuvant chemotherapy has been evaluated for high-risk prostate cancer. The combination of hormonal therapy and chemotherapy with docetaxel appears to be associated with downstaging of disease and is well tolerated.
There have been several phase III trials evaluating the benefit of chemotherapy prior to surgery associated with hormonal therapy, but currently results of these trials have not yet been reported. Two important current trials evaluating neoadjuvant docetaxel based (and estramustine) chemotherapy is described.
The Cancer and Leukemia Group B is currently conducting a phase III randomized trial (CALGB 90203) which is evaluating neoadjuvant chemotherapy and ADT prior to radical prostatectomy versus immediate radical prostatectomy in patients with high risk localized prostate cancer (stage T1 to T3a NX M0). In this trial 750 patients have been treated with 6 months of androgen deprivation plus eight cycles of neoadjuvant taxane based chemotherapy followed by radical prostatectomy with lymph node dissection compared to surgery alone. The primary end point of the trial is progression-free survival at 5 years (21).
The GETUG 12 trial, a French randomized phase III study, compared four cycles of neoadjuvant treatment with docetaxel and estramustine prior to local therapy plus ADT for 3 years versus local therapy and ADT for 3 years. In this trial 413 patients were included with locally advanced or high-risk prostate cancer treated locally with radiotherapy, in most cases (87%). The study showed a borderline significant improvement in progression free survival (PFS) in the combination arm compared with ADT alone (HR =0.75, 95% CI, 0.55-1.01; P=0.06). Another benefit was shown in PSA response that was significantly higher in the group treated with chemotherapy than in the patients treated with ADT alone. The combination of docetaxel and estramustine had an acceptable l toxicity profile (22).
Adjuvant trials
There are several large trials assessing adjuvant docetaxel based chemotherapy in patients with high risk localized prostate cancer treated with radical prostatectomy. None of the phase III trials available investigating the use of docetaxel-based chemotherapy after surgery, have reported mature results because longer follow-up is required (Table 1).
A prospective phase III RTOG 0521 trial was designed to assess the efficacy of adjuvant chemotherapy with docetaxel combined with ADT and radiotherapy. This study is investigating high-risk patients receiving ADT for a total of 2 years plus radiotherapy with or without adjuvant docetaxel chemotherapy for six cycles. The primary endpoint is overall survival (ClinicalTrials.gov; Identifier: NCT00288080).
TAX 3501 was a phase III trial evaluating immediate adjuvant therapy or active surveillance with therapy at the time of biochemical progression. High risk patients were randomly assigned to receive observation, androgen therapy with leuprorelin acetate for 18 months or leuprorelin acetate plus docetaxel 75 mg/m2 every 3 weeks for six cycles. The primary end point was progression-free survival. This trial was prematurely closed due to enrollment difficulties, leaving results insufficient and underpowered to detect significant differences in PFS (23).
A multi arm and multicenter trial conducted by the Medical Research Council called the Systemic Therapy in Advanced or Metastatic Prostate Cancer: Evaluation of Drug Efficacy (STAMPEDE) trial is the largest trial with a multistage design which is evaluating several drugs in combination with hormonal therapy in patients with high-risk localized or metastatic prostate cancer (ClinicalTrials.gov identifier NCT00268476). The purpose of the trial is to compare further treatments, including docetaxel, zoledronic acid, celecoxib, abiraterone, enzalutamide and radiotherapy (only among the patients with metastatic disease) in combination with ADT vs. ADT alone. Moreover the study is evaluating whether these second line treatments should be included earlier in the management of prostate cancer. The primary objective of the STAMPEDE trial is overall survival. The intermediate primary outcome is failure-free survival. The study started in October 2005 with five original experimental arms compared to the control arm.
In November 2011 a new arm was introduced assessing abiraterone, prednisone and ADT and accrual was completed in January 2014. Another new arm evaluating radiotherapy to the prostate for newly diagnosed metastatic patients was initiated in January 2013. Recently, in January 2014 a new arm evaluating the combination of enzalutamide, abiraterone, and prednisone with ADT was initiated (24). The celecoxib arm was closed for lack of sufficient activity at the second interim analysis (25). The arms with zoledronic acid, docetaxel, and zoledronic acid with docetaxel have closed successfully their enrollment in March 2013.
Currently the total number of arms in the STAMPEDE trial is eight.
An interim analysis on survival outcomes in the control ADT arm showed an improvement in overall survival in this cohort of patients with newly diagnosed metastatic disease receiving standard of care therapy compared to previous reports in literature (26).
The final comparative survival results should emerge in mid-2015 and are eagerly anticipated.
Hormonal therapy and chemotherapy in metastatic disease
It has been recently demonstrated that the use of chemotherapy can improve outcomes in patients with metastatic hormone naive prostate cancer. It appears that some patients initiating hormonal therapy may actually be better candidates for cytotoxic therapy at this stage of disease than when their disease becomes castration resistant (27,28).
It has been controversial as to whether or not early chemotherapy in hormone naive patients would be beneficial. There have been arguments for and against this approach. In favor is the idea that attacking de novo testosterone independent clones early should allow ADT to keep prostate cancer in remission longer. In addition, there is the possibility that some patients at the time of progression may be too frail to receive chemotherapy.
Alternatively, ADT may take cells out of cycle and make them less responsive to cytotoxics. The fact that some patients respond for long periods to ADT and never need chemotherapy is the other argument against early chemotherapy.
Since the early 80’s several studies tried to clarify these differing viewpoints, investigating the addition of chemotherapy with hormonal therapy in patients with metastatic prostate cancer (29-34).
None of the trials reported positive results, concluding that androgen suppression remains the preferred first line treatment in metastatic prostate cancer and that there was no cytotoxic regimen with consistent activity against hormone-sensitive prostate cancer.
Over the years it has been noted that none of these trials included cytotoxic therapy shown to prolong overall survival in the setting of metastatic CRPC. The availability of active chemotherapy for CRPC has led to renewed interest and investigation of this topic with different agents in hormone sensitive disease.
The trial by Millikan et al. included 286 patients and compared ketoconazole and doxorubicin alternating with vinblastine and estramustine in addition to ADT vs. standard ADT. They showed no differences in time to progression to CRPC and in median survival between the two groups (35).
Another study conducted by Wang et al. compared the combination of mitoxantrone and ADT with ADT alone in 93 patients with locally advanced or metastatic prostate cancer. Overall survival and responses were significantly improved in patients with locally advanced disease treated with mitoxantrone, but patients with metastatic disease did not show benefit (36).
A French trial, GETUG-15, conducted by Gravis and colleagues investigated 385 patients affected by metastatic hormone sensitive prostate cancer with the combination of docetaxel and ADT (28). This study was the first to investigate an agent shown to prolong overall survival in CRPC and the rationale was that this agent should have more efficacies in men with initial metastatic prostate cancer than in patients with the castration resistant disease. Patients received up to nine cycles of docetaxel. At median follow-up of 50 months the majority of patients had what is today considered “low volume” disease and the results showed a significantly improvements in clinical PFS (cPFS) and biochemical PFS without a significant difference in overall survival.
At ASCO GU 2015 updated results have been presented with a longer follow-up, of some 80 months, showing that the median overall survival was 46.5 months in the ADT arm and 60.9 months in the ADT + D arm (HR =0.9, 95% CI, 0.7-1.2). In a retrospective analysis using the same definition of high volume disease (HVD) as in the CHAARTED trial discussed below, the subgroup of patients with HVD showed a median overall survival of 35.1 months in the ADT alone arm compared to 39 months in the ADT plus chemotherapy arm (HR =0.8, 95% CI, 0.6-1.2). The outcomes in HVD patients were similar to those in the CHAARTED trial, however the trial showed a non-significant improvement in overall survival with ADT + D of about 4 months (37).
An important trial regarding the combination of chemotherapy and hormonal therapy in patients affected by metastatic prostate cancer is the CHAARTED trial (ChemoHormonal Therapy vs. Androgen Ablation Randomized Trial for Extensive Disease in Prostate Cancer), the ECOG-led phase III trial presented by Sweeney et al. at ASCO in 2014 (27). In this trial, early chemotherapy with docetaxel in combination with ADT in hormone naive metastatic prostate cancer patients was compared to ADT alone. In the study 790 patients received chemotherapy with docetaxel 75 mg/m2 every 21 days for a maximum of six cycles plus ADT or ADT alone. Twice daily prednisone was not used. This trial emphasized the concept of HVD, in fact patients were stratified as high-volume or low-volume according to the extension of metastatic disease. High volume was defined as visceral metastasis (lung or liver) and/or four or more bone metastases (with at least one beyond the pelvis and vertebral column). At study initiation, only patients with high-volume disease were to be accrued, but the study was amended to also include low volume disease patients. Unlike the GETUG-15 trial, approximately two-thirds of patients in CHAARTED had HVD. The primary endpoint was overall survival while secondary endpoints were time to progressive disease and time to symptomatic progressive disease.
The association of chemotherapy and ADT in this trial was motivated by the hypothesis that testosterone independent cellular clones would be best treated early with cytotoxic chemotherapy (27). Moreover it has been reported in several studies, including that of the SWOG trial of intermittent vs. continuous therapy that the presence of high tumor burden with visceral disease and bone involvement beyond the axial skeleton is correlated with poor prognosis and shorter survival (35,36,38).
In the CHAARTED study, the combination of docetaxel and ADT showed a benefit in overall survival of 14 months compared to ADT alone, with a median overall survival of 57.6 vs. 44 months (HR =0.61, 95% CI, 0.47-0.80; P=0.0003). In the HVD group, median overall survival was 49.2 months with docetaxel plus ADT compared with 32.2 months with ADT (HR =0.60, 95% CI, 0.45-0.81; P=0.0006), a 17-month difference in overall survival. In patients with low-volume disease, median overall survival has not yet been reached at the time of the analysis, at a median follow-up of 29 months. The CHAARTED trial results also demonstrated improvement in median time to clinical progression and in median time to the development of castration resistant status.
Of special interest, the median time to clinical progression in the docetaxel plus ADT group was 32.7 months as compared to 19.8 months in the ADT arm (HR =0.49, 95% CI, 0.37-0.65; P<0.0001). In addition, the median time to CRPC was 20.7 months in the combination arm compared with 14.7 in the ADT alone arm (HR =0.56, 95% CI, 0.44-0.70; P<0.0001). Of note, 129/174 (74%) of patients who progressed on ADT subsequently received docetaxel.
The adverse event profile was favorable and lower than previously seen in CRPC trials, reporting 6% of febrile neutropenia in patients receiving the chemo-hormonal regimen. There was one sudden death in the chemotherapy arm. Grade 3 non-hematologic toxicity was low, with 2% allergic reactions and 4% having fatigue. A total of 1% of patients experienced G3 toxicity of sensory nerves and 1% of motor nerves.
There are several critical points about this trial. First of all, the concept of high and low volume disease should be more profoundly considered, as there is evidence of this also from earlier studies from the SWOG (SWOG trials S8894 and S9346) and from the MD Anderson Hospital (35,36,38). This can dramatically change our first line treatment choices for patients with metastatic prostate cancer. Final publications of these data are awaited.
Hormonal therapy and chemotherapy in CRPC patients
CRPC is an aggressive disease that contains heterogeneous types of cells developing a variety of abnormal pathways to survive in a castrate environment. The biological heterogeneity of prostate cancer cells has become clear as there are different clinical subsets of patients, from indolent tumors to those that are aggressive and lethal with multiple metastases. The biological and clinical heterogeneity dictates the different therapeutic options in the management of CRPC.
Heterogeneity of castration resistance prostate cancer
Even though the AR plays a major role in the progression to CRPC, alternative pathways can have a role in stimulating prostate cancer cells, confirming the cellular heterogeneity in prostate cancer (39,40).
Prostate cancer cells can develop alternative AR independent molecular pathways for survival that bypass AR activation, including cancer stem cells, receptor tyrosine kinases and neuroendocrine differentiation (NE) (41). A potential mechanism for survival in the castrate environment is the presence of prostate cancer stem cells that continually supply the cancer cell population, despite therapy. These cells are not affected by ADT and can differentiate into androgen dependent and independent cells, leading to a heterogeneous phenotype of AR (42,43).
Activation of the PI3 kinase signaling pathway is critical for the survival of prostate cancer cells. PTEN is a tumor suppressor and has lipid phosphatase activity that metabolizes PIP3 (phosphatidylinositol triphosphate). The PTEN function is expressed primarily through negative regulation of the PI3K/Akt pathway. PTEN is inactivated in several types of cancers, including prostate cancer. Loss of PTEN function in prostate cancer can occur through several mechanisms, including deletion, mutation and methylation. These events can cause tumor cell survival through selective pressure caused by ADT (44-46).
Another potentially relevant pathway is NE of tumor cells in prostate cancer. The prevalence of NE cells in prostate adenocarcinoma varies from 30% to 100% and they do not express the AR. These cells may develop from a predominantly adenocarcinoma PSA secreting environment under the pressure of ADT. NE cells may contribute to the progression to CRPC through the production of neurosecretory products, such as parathyroid hormone-related protein, the neurotransmitter serotonin, the neuropeptide hormone bombesin, calcitonin, chromagranin A, neurotensin, and thyroid-stimulatory hormone (6,44,45). Patient with predominantly NE or small cell carcinoma should be treated with cisplatin based chemotherapy (47).
Chemotherapy treatment in CRPC
Systemic chemotherapy is one of the options for the treatment of metastatic CRPC. Taxanes represent the class of chemotherapeutic agents that have shown a benefit in terms of overall survival. In particular, docetaxel and recently cabazitaxel have become the currently standard first and second-line chemotherapy agents for the treatment of metastatic prostate cancer patients after ADT failure (14,15,45).
SWOG 99-16 and TAX327 trials are the most important randomized studies showing the benefit of chemotherapy with docetaxel in metastatic prostate cancer.
In the TAX327 trial, 1,006 patients were randomized to receive docetaxel (30 mg/m2 weekly or 75 mg/m2 every 3 weeks) plus prednisone or mitoxantrone 12 mg/m2 every 3 weeks plus prednisone. This trial demonstrated a significant improvement in overall survival in the patient group treated with every 3 weeks docetaxel compared to mitoxantrone, leading also to an advantage in other secondary endpoints such as pain and quality of life (14).
In the SWOG 99-16 trial, patients with metastatic CRPC were randomized to receive estramustine, the combination of non-nitrogen mustard and estradiol and docetaxel vs. mitoxantrone and prednisone. This trial confirmed that docetaxel was associated with a significant benefit in overall survival. However, there was significant myelosuppression, DVTs and gastrointestinal toxicities correlated with the combination of docetaxel and estramustine. Thus, docetaxel plus prednisone has become the standard of care for the first-line treatment of progressive CRPC (15).
Cabazitaxel is a new taxane approved as a second-line treatment in metastatic CRPC following docetaxel therapy with a significant survival benefit compared to mitoxantrone. The TROPIC trial evaluated 755 patients treated with cabazitaxel plus prednisone compared to mitoxantrone plus prednisone. The primary endpoint was overall survival, which was 15.1 months in the cabazitaxel plus prednisone arm and 12.7 months in the mitoxantrone plus prednisone arm. Other secondary endpoints such as progression-free survival, safety, tumor response, time to tumor progression and PSA response rate were all improved in the cabazitaxel plus prednisone arm (48). An ongoing phase III study (Cabazitaxel vs. Docetaxel Both With Prednisone in Patients With Metastatic CRPC, FIRSTANA) is evaluating cabazitaxel as first-line cytotoxic therapy, randomizing patients with metastatic CRPC to receive docetaxel vs. cabazitaxel (ClinicalTrials.gov; Identifier: NCT01308567).
At the cellular level taxanes stabilize microtubules. The microtubules are dynamic elements of the cytoskeleton necessary for the many cellular events, such as mitotic synthesis and intracellular protein transportation (49,50). There is preclinical evidence that treatment with taxanes can interfere with AR activity in addition to blocking cell division, evidence that enables new insights into the therapeutic efficacy of microtubule-targeting drugs in prostate cancer. In prostate cancer cells, taxanes inhibit AR nuclear signaling binding cellular microtubules, blocking AR nuclear translocation and consequently transcriptional activity. Microtubules facilitate AR nuclear translocation and enhance downstream AR transcriptional activity in prostate cancer cells. Microtubule targeting chemotherapy blocks this pathway and suppresses AR signaling, through a negative feedback mechanism; AR signaling inhibits tubulin expression thus impairing the cytoskeleton structure and organization.
Despite the efficacy of taxanes in CRPC, the real benefit can vary according to the clinical setting and host factors. Clinical resistance often occurs and can be explained by various mechanisms. Some of these are the presence of p-glycoprotein or other drug transporters that impair the uptake of the drug, the presence of tubulin mutations or the overexpression of the βIII tubulin isotype that impairs the binding to β-tubulin and the presence of AR mutations or splice variants that do not require microtubule-based transport (51-54).
Hormonal treatments in CRPC
Novel approaches that target the AR signaling axis in CRPC patients are hormonal agents. Some of the most important hormonal agents that have demonstrated improved overall survival in CRPC are abiraterone and enzalutamide (55-57).
Abiraterone is a potent and specific steroidogenic inhibitor that irreversibly inhibits the enzyme CYP17A1, the most important enzyme that catalyzes two essential steroidogenic reactions, the 17α-hydroxylase and 17,20-lyase responsible for converting pregnenolone to 17-OH-pregnenolone and subsequently 17-OH-pregnenolone to DHEA and androstenedione (58).
Abiraterone at 1,000 mg daily with prednisone 5 mg twice daily has demonstrated an overall survival benefit in patients with metastatic CRPC who have progressed before and after docetaxel treatment.
The phase III COU-AA-301 trial evaluated abiraterone and prednisone (2:1) vs. placebo and prednisone in 1,195 patients with metastatic CRPC pretreated with docetaxel and up to two lines of chemotherapy. Abiraterone was the first novel hormonal therapy to demonstrate a significant improvement in overall survival, with a 26% reduction in the risk of death (HR =0.74, 95% CI, 0.638-0.859; P<0.0001), and significant improvements in radiographic progression-free survival, time to PSA progression and PSA responses (54-56).
The phase III COU-AA-302 trial compared (1:1) abiraterone plus prednisone with placebo plus prednisone in asymptomatic or mildly symptomatic chemo-naive and ketoconazole-naive metastatic CRPC patients without visceral disease and with only bone or lymph node metastases. This trial showed that abiraterone was associated with delays in disease progression and a significant improvement in overall survival at 49 months of follow-up, despite the fact that 44% of patients in the placebo arm crossed over to active abiraterone (59).
Enzalutamide is a novel AR inhibitor that binds to the AR with eight times more affinity than bicalutamide. This hormonal agent possesses three mechanisms of action in blocking the AR. It blocks testosterone binding to the AR, impairs nuclear translocation of the AR and inhibits association of the AR with DNA (57,60). This drug is administered without corticosteroids and has shown an improvement in overall survival in both the pre and post chemotherapy settings.
The phase III AFFIRM trial was a randomized (2:1) study in 1,190 patients that investigated enzalutamide 160 mg/d or placebo in patients with metastatic CRPC who had previously received docetaxel. This study demonstrated a median benefit in overall survival of 4.8 months and a 37% reduction in the risk of death (HR =0.631, 95% CI, 0.529-0.752; P<0.0001) with enzalutamide vs. placebo in patients with progressive CRPC (61).
The randomized PREVAIL study evaluated (1:1) enzalutamide vs. placebo in 1,717 chemo-naive patients affected by metastatic CRPC. This trial showed that enzalutamide decreased the risk of death by 29% (HR =0.19, 95% CI, 0.15-0.23; P<0.0001), the risk of radiographic progression by 81% and delayed the initiation of chemotherapy in patients with metastatic CRPC (62).
Despite these excellent results, many patients treated with abiraterone and enzalutamide develop resistance to these therapies and our knowledge of the pathogenesis of resistance to these agents is improving but extremely limited.
It has been recently demonstrated that the presence of AR splice variants is correlated with resistance to abiraterone and enzalutamide. Antonarakis et al. utilized a quantitative reverse-transcriptase-polymerase-chain-reaction assay to assess AR-V7 splice variants in circulating tumor cells (CTCs) from 62 prospectively enrolled patients with metastatic CRPC who were initiating treatment with either enzalutamide or abiraterone. This study showed that the presence of the AR-V7 splice variant derived from the RNA in the CTCs of these patients was associated with an absolute absence of response to abiraterone or enzalutamide and poor survival. The AR-V7 splice variant may be one of the first biomarkers to individualize patients who respond to these hormonal agents, but these data must to be validated (63,64).
Conclusions
The treatment paradigm of prostate cancer is continuously evolving and increasing knowledge about the pathogenesis and heterogeneity of this disease is leading to new approaches that include both old and new agents. Both hormonal therapy and chemotherapy target AR signaling have been shown to corroborate the importance of the AR axis in the treatment of prostate cancer.
Despite the improved knowledge of prostate cancer molecular biology, the absence of adequate biomarkers hinders our abilities in selecting patients who may derive the most benefit from hormonal or chemotherapy treatments. Apart from molecular classification, the correct timing, optimal sequencing and the association of these therapies are all subjects of ongoing and future study.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Schröder FH, Hugosson J, Roobol MJ, et al. Prostate-cancer mortality at 11 years of follow-up. N Engl J Med 2012;366:981-90. [PubMed]
- Huggins C, Hodges CV. Studies on prostatic cancer: I. The effect of castration, of estrogen and of androgen injection on serum phosphatases in metastatic carcinoma of the prostate. 1941. J Urol 2002;168:9-12. [PubMed]
- Denis LJ, Keuppens F, Smith PH, et al. Maximal androgen blockade: final analysis of EORTC phase III trial 30853. EORTC Genito-Urinary Tract Cancer Cooperative Group and the EORTC Data Center. Eur Urol 1998;33:144-51. [PubMed]
- Singer EA, Golijanin DJ, Miyamoto H, et al. Androgen deprivation therapy for prostate cancer. Expert Opin Pharmacother 2008;9:211-28. [PubMed]
- Feldman BJ, Feldman D. The development of androgen-independent prostate cancer. Nat Rev Cancer 2001;1:34-45. [PubMed]
- Debes JD, Tindall DJ. Mechanisms of androgen-refractory prostate cancer. N Engl J Med 2004;351:1488-90. [PubMed]
- Scher HI, Buchanan G, Gerald W, et al. Targeting the androgen receptor: improving outcomes for castration-resistant prostate cancer. Endocr Relat Cancer 2004;11:459-76. [PubMed]
- Gelmann EP. Molecular biology of the androgen receptor. J Clin Oncol 2002;20:3001-15. [PubMed]
- Labrie F. Adrenal androgens and intracrinology. Semin Reprod Med 2004;22:299-309. [PubMed]
- Trapman J, Cleutjens KB. Androgen-regulated gene expression in prostate cancer. Semin Cancer Biol 1997;8:29-36. [PubMed]
- Chen Y, Sawyers CL, Scher HI. Targeting the androgen receptor pathway in prostate cancer. Curr Opin Pharmacol 2008;8:440-8. [PubMed]
- Edwards J, Krishna NS, Grigor KM, et al. Androgen receptor gene amplification and protein expression in hormone refractory prostate cancer. Br J Cancer 2003;89:552-6. [PubMed]
- Mostaghel EA, Page ST, Lin DW, et al. Intraprostatic androgens and androgen-regulated gene expression persist after testosterone suppression: therapeutic implications for castration-resistant prostate cancer. Cancer Res 2007;67:5033-41. [PubMed]
- Tannock IF, de Wit R, Berry WR, et al. Docetaxel plus prednisone or mitoxantrone plus prednisone for advanced prostate cancer. N Engl J Med 2004;351:1502-12. [PubMed]
- Petrylak DP, Tangen CM, Hussain MH, et al. Docetaxel and estramustine compared with mitoxantrone and prednisone for advanced refractory prostate cancer. N Engl J Med 2004;351:1513-20. [PubMed]
- Pound CR, Partin AW, Epstein JI, et al. Prostate-specific antigen after anatomic radical retropubic prostatectomy. Patterns of recurrence and cancer control. Urol Clin North Am 1997;24:395-406. [PubMed]
- D’Amico AV, Whittington R, Malkowicz SB, et al. Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 1998;280:969-74. [PubMed]
- D'Amico AV, Cote K, Loffredo M, et al. Determinants of prostate cancer-specific survival after radiation therapy for patients with clinically localized prostate cancer. J Clin Oncol 2002;20:4567-73. [PubMed]
- Bastian PJ, Boorjian SA, Bossi A, et al. High-risk prostate cancer: from definition to contemporary management. Eur Urol 2012;61:1096-106. [PubMed]
- Kattan MW, Eastham JA, Stapleton AM, et al. A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst 1998;90:766-71. [PubMed]
- Eastham JA, Kelly WK, Grossfeld GD, et al. Cancer and Leukemia Group B (CALGB) 90203: a randomized phase 3 study of radical prostatectomy alone versus estramustine and docetaxel before radical prostatectomy for patients with high-risk localized disease. Urology 2003;62:55-62. [PubMed]
- Fizazi K, Lesaunier F, Delva R, et al. A phase III trial of docetaxel-estramustine in high-risk localised prostate cancer: a planned analysis of response, toxicity and quality of life in the GETUG 12 trial. Eur J Cancer 2012;48:209-17. [PubMed]
- Schweizer MT, Huang P, Kattan MW, et al. Adjuvant leuprolide with or without docetaxel in patients with high-risk prostate cancer after radical prostatectomy (TAX-3501): important lessons for future trials. Cancer 2013;119:3610-8. [PubMed]
- Attard G, Sydes MR, Mason MD, et al. Combining enzalutamide with abiraterone, prednisone, and androgen deprivation therapy in the STAMPEDE trial. Eur Urol 2014;66:799-802. [PubMed]
- James ND, Sydes MR, Mason MD, et al. Celecoxib plus hormone therapy versus hormone therapy alone for hormone-sensitive prostate cancer: first results from the STAMPEDE multiarm, multistage, randomised controlled trial. Lancet Oncol 2012;13:549-58. [PubMed]
- James ND, Spears MR, Clarke NW, et al. Survival with Newly Diagnosed Metastatic Prostate Cancer in the “Docetaxel Era”: Data from 917 Patients in the Control Arm of the STAMPEDE Trial (MRC PR08, CRUK/06/019). Eur Urol 2015;67:1028-38. [PubMed]
- Sweeney C, Chen YH, Carducci MA, et al. Impact on overall survival (OS) with chemohormonal therapy versus hormonal therapy for hormone-sensitive newly metastatic prostate cancer (mPrCa): An ECOG-led phase III randomized trial. J Clin Oncol 2014;32:abstr LBA2.
- Gravis G, Fizazi K, Joly F, et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): a randomised, open-label, phase 3 trial. Lancet Oncol 2013;14:149-58. [PubMed]
- Fontana D, Bertetto O, Fasolis G, et al. Randomized comparison of goserelin acetate versus mitomycin C plus goserelin acetate in previously untreated prostate cancer patients with bone metastases. Tumori 1998;84:39-44. [PubMed]
- Murphy GP, Beckley S, Brady MF, et al. Treatment of newly diagnosed metastatic prostate cancer patients with chemotherapy agents in combination with hormones versus hormones alone. Cancer 1983;51:1264-72. [PubMed]
- Murphy GP, Huben RP, Priore R. Results of another trial of chemotherapy with and without hormones in patients with newly diagnosed metastatic prostate cancer. Urology 1986;28:36-40. [PubMed]
- Osborne CK, Blumenstein B, Crawford ED, et al. Combined versus sequential chemo-endocrine therapy in advanced prostate cancer: final results of a randomized Southwest Oncology Group study. J Clin Oncol 1990;8:1675-82. [PubMed]
- Pummer K, Lehnert M, Stettner H, et al. Randomized comparison of total androgen blockade alone versus combined with weekly epirubicin in advanced prostate cancer. Eur Urol 1997;32:81-5. [PubMed]
- Janknegt RA, Boon TA, van de Beek C, et al. Combined hormono/chemotherapy as primary treatment for metastatic prostate cancer: a randomized, multicenter study of orchiectomy alone versus orchiectomy plus estramustine phosphate. The Dutch Estracyt Study Group. Urology 1997;49:411-20. [PubMed]
- Millikan RE, Wen S, Pagliaro LC, et al. Phase III trial of androgen ablation with or without three cycles of systemic chemotherapy for advanced prostate cancer. J Clin Oncol 2008;26:5936-42. [PubMed]
- Wang J, Halford S, Rigg A, et al. Adjuvant mitozantrone chemotherapy in advanced prostate cancer. BJU Int 2000;86:675-80. [PubMed]
- Gravis G, Boher JM, Joly F, et al. Androgen deprivation therapy (ADT) plus docetaxel (D) versus ADT alone for hormone-naïve metastatic prostate cancer (PCa): Long-term analysis of the GETUG-AFU 15 phase III trial. J Clin Oncol 2015;abstr 140.
- Eisenberger MA, Blumenstein BA, Crawford ED, et al. Bilateral orchiectomy with or without flutamide for metastatic prostate cancer. N Engl J Med 1998;339:1036-42. [PubMed]
- Hussain M, Tangen CM, Berry DL, et al. Intermittent versus continuous androgen deprivation in prostate cancer. N Engl J Med 2013;368:1314-25. [PubMed]
- Hoimes CJ, Kelly WK. Redefining hormone resistance in prostate cancer. Ther Adv Med Oncol 2010;2:107-123. [PubMed]
- Attar RM, Takimoto CH, Gottardis MM. Castration-resistant prostate cancer: locking up the molecular escape routes. Clin Cancer Res 2009;15:3251-5. [PubMed]
- Collins AT, Berry PA, Hyde C, et al. Prospective identification of tumorigenic prostate cancer stem cells. Cancer Res 2005;65:10946-51. [PubMed]
- Shah RB, Mehra R, Chinnaiyan AM, et al. Androgen-independent prostate cancer is a heterogeneous group of diseases: lessons from a rapid autopsy program. Cancer Res 2004;64:9209-16. [PubMed]
- Craft N, Chhor C, Tran C, et al. Evidence for clonal outgrowth of androgen-independent prostate cancer cells from androgen-dependent tumors through a two-step process. Cancer Res 1999;59:5030-6. [PubMed]
- Zhu ML, Kyprianou N. Androgen receptor and growth factor signaling cross-talk in prostate cancer cells. Endocr Relat Cancer 2008;15:841-9. [PubMed]
- Whang YE, Wu X, Suzuki H, et al. Inactivation of the tumor suppressor PTEN/MMAC1 in advanced human prostate cancer through loss of expression. Proc Natl Acad Sci U S A 1998;95:5246-50. [PubMed]
- Beltran H, Tomlins S, Aparicio A, et al. Aggressive variants of castration-resistant prostate cancer. Clin Cancer Res 2014;20:2846-50. [PubMed]
- de Bono JS, Oudard S, Ozguroglu M, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. Lancet 2010;376:1147-54. [PubMed]
- Torres K, Horwitz SB. Mechanisms of Taxol-induced cell death are concentration dependent. Cancer Res 1998;58:3620-6. [PubMed]
- Jordan MA, Wilson L. Microtubules as a target for anticancer drugs. Nat Rev Cancer 2004;4:253-65. [PubMed]
- Darshan MS, Loftus MS, Thadani-Mulero M, et al. Taxane-induced blockade to nuclear accumulation of the androgen receptor predicts clinical responses in metastatic prostate cancer. Cancer Res 2011;71:6019-29. [PubMed]
- Gan L, Chen S, Wang Y, et al. Inhibition of the androgen receptor as a novel mechanism of taxol chemotherapy in prostate cancer. Cancer Res 2009;69:8386-94. [PubMed]
- Zhu ML, Horbinski CM, Garzotto M, et al. Tubulin-targeting chemotherapy impairs androgen receptor activity in prostate cancer. Cancer Res 2010;70:7992-8002. [PubMed]
- Kavallaris M. Microtubules and resistance to tubulin-binding agents. Nat Rev Cancer 2010;10:194-204. [PubMed]
- de Bono JS, Logothetis CJ, Molina A, et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364:1995-2005. [PubMed]
- Fizazi K, Scher HI, Molina A, et al. Abiraterone acetate for treatment of metastatic castration-resistant prostate cancer: final overall survival analysis of the COU-AA-301 randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 2012;13:983-92. [PubMed]
- Scher HI, Beer TM, Higano CS, et al. Antitumour activity of MDV3100 in castration-resistant prostate cancer: a phase 1-2 study. Lancet 2010;375:1437-46. [PubMed]
- Jarman M, Barrie SE, Llera JM. The 16,17-double bond is needed for irreversible inhibition of human cytochrome p45017alpha by abiraterone (17-(3-pyridyl)androsta-5, 16-dien-3beta-ol) and related steroidal inhibitors. J Med Chem 1998;41:5375-81. [PubMed]
- Ryan CJ, Smith MR, de Bono JS, et al. Abiraterone in metastatic prostate cancer without previous chemotherapy. N Engl J Med 2013;368:138-48. [PubMed]
- Tran C, Ouk S, Clegg NJ, et al. Development of a second-generation antiandrogen for treatment of advanced prostate cancer. Science 2009;324:787-90. [PubMed]
- Scher HI, Fizazi K, Saad F, et al. Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 2012;367:1187-97. [PubMed]
- Beer TM, Armstrong AJ, Rathkopf DE, et al. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014;371:424-33. [PubMed]
- Antonarakis ES, Lu C, Wang H, et al. AR-V7 and resistance to enzalutamide and abiraterone in prostate cancer. N Engl J Med 2014;371:1028-38. [PubMed]
- Sun S, Sprenger CC, Vessella RL, et al. Castration resistance in human prostate cancer is conferred by a frequently occurring androgen receptor splice variant. J Clin Invest 2010;120:2715-30. [PubMed]


