Interstitial cystitis/painful bladder syndrome: diagnostic evaluation and therapeutic response in a private urogynecology unit
Background
Interstitial cystitis/painful bladder syndrome (IC/PBS) was defined by The Society of Urodynamics, Female Pelvic Medicine & Urogenital Reconstruction as “an unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder, associated with lower urinary tract symptoms of more than 6 weeks duration, in the absence of infection or other identifiable causes” (1).
This disease has likely a multi-factorial etiology including epithelial dysfunction, subclinical infection, mast cell and vascular abnormalities, neurogenic inflammation, autoimmune phenomena and up regulation of sensory nerves in the bladder (2,3). The current acceptable theory is injury or dysfunction of the glycosaminoglycan layer that covers the urothelium (4). This injury can be caused by bacterial cystitis, childbirth, pelvic surgery or urological instrumentation. These factors provoke sensory nerve activation, neurogenic inflammation, pain and fibrosis (5).
The aim of this study was to describe endoscopic features and our experience on the treatment of IC/PBS in Urodifem de Occidente S.C., a private urogynecology unit.
The diagnosis of IC/PBS can be challenging. Patients present with a wide spectrum of symptoms, physical exam findings and emotional affectation. IC/PBS has the potential to affect the quality of life of these patients with expressions of depressive disorders, anxiety, sleep disturbance and recurrent urinary tract infections. The average time from presentation to the physician ranges from 3 to 7 years (5).
For a correct diagnosis is necessary to practice an orderly and thorough assessment of the patient on the basis of a complete medical history in which the most important symptoms are represented by pain, pressure or pelvic discomfort accompanied by increases day and night urinary frequency, as well as urgency. The urogynecology questionnaire is a powerful aid in this respect. During the gynecologic examination, it is common to detect annoying sensation in the anterior vaginal wall. The physical examination excludes other urinary tract diseases. Urodynamic testing shows low compliance with low values of volume urinated. It is our habit to systematically perform uroflowmetry in all our patients with lower urinary tract symptoms.
Cystoscopy is the test that provides the most relevant information on IC/PBS. Its practice allows differentiation between patients with chronic pelvic pain, those with painful bladder and those who suffer interstitial cystitis (IC). Cystoscopy is essential to detect lesions in the urothelium and distinguish them from those of IC (6). These bladder lesions can be grouped as subepithelial hemorrhagic areas, glomerulations or Hunner’s classic ulcer. It is our costume to practice two bladder distention and asking our patient to tolerate pain as much as she can. If there are not visible epithelial modification during distention, but pain is present, then we diagnose painful bladder. It’s our position that the recognition of IC/PBS can be performed without the need of anesthesia, since this entails an increase in cost for patient. However, we recognize the value of it and the possibility of practicing it in case of doubt.
There is controversy regarding the systematic practice of vesical biopsy. However, we usually propose it to our patient. To avoid increasing costs, our usual practice consists in its performance as an office procedure, without anesthesia, as we described in a prior publication (7).
Methods
We conducted an analytical, descriptive and retrospective study of 33 patients diagnosed of IC/PBS, from a pool of 925 patients attended in Urodifem for some lower urinary tract dysfunction, from January 2001 to March 2015.
Inclusion criteria: (I) complete clinical history and examination; (II) urogynecological questionnaire; (III) absence of malignant or neurological diseases, and acute urinary tract infection; (IV) presence of pelvic pain or discomfort associated to bladder, accompanied by urinary frequency and urgency; (V) uroflowmetry and measurement of post void residual; (VI) urethrocystoscopy; (VII) biopsy of significant bladder lesion; (VIII) objective evaluation of symptoms and quality of life pre- and post-treatment [Interstitial Cystitis Symptom Average Index (ICSI) and Interstitial Cystitis Problem Average Index (ICPI) questionnaires].
In the evaluation of results, we have classified as “remission” when a patient has remained asymptomatic without any medication for a period of at least 6 months; “improvement” if it deprives a decrease of symptoms greater than 50% supported by the patient’s feelings, (subjective evaluation) and by the application of questionnaires ICSI and ICPI. “Failure” if the response to the treatment is negative. The diagnostic criterion used in this study is based on the definition established by the Society of Urodynamics, Female Pelvic Medicine.
Results
From a total of 33 patients diagnosed with IC/PBS, we included 25 which satisfied inclusion criteria and finished at least six dymetilsulfoxido (DMSO) instillations.
The mean of age was 54.1 years (range: 24 to 81 years).
The predominant symptoms were increased day and night urinary frequency in 96% of our patients; pain in 88% and urgency in 80%.
The most frequently described pain site was the suprapubic region in 86%; accompanied by vaginal or urethral pain in 82%.
The uroflowmetry results were as follows: the mean volume urinated was 236.72 mL, (range: 29 to 590 mL). Only one patient urinated more than 400 mL. The mean of post void residual urine was 58.20 mL. The functional bladder capacity had an average of 294 mL with a range of 29 to 780 mL.
As a clinical and lab finding, hematuria (both macro and microscopically), was found in 12 patients (48%).
Cystoscopic findings were: in eight cases, areas of subepithelial haemorrhage (32%), Hunner’s ulcer in seven cases (28%), and glomerulations in seven cases (28%). In three cases no endoscopic lesions were seen, but pain throughout the bladder distention was present and so they were classified as painful bladder.
Biopsy was taken in 12 patients who had significant lesions. In ten of these, the histological evaluation was compatible with the characteristic findings seen in IC. In the other two cases, the diagnosis was ulcerated acute cystitis.
In relation to the treatment, our basic scheme involves 14 bladder instillations of a mixture of dimethyl sulfoxide at a 50% concentration, 10,000 units of heparin, and 8 mg of dexamethasone. We start with one instillation per week for 6 weeks; four instillations every 2 weeks for 2 months and finally monthly for a minimum of 4 months. At the end of the first six instillations, we proceed with the administration of pentosan polysulphate sodium at least during 1 year and according to response.
The basic treatment was applied to 18 patients. In three patients, eight treatments instead of the basic 14 were applied. In two cases just seven instillations, and in two other cases, six instillations were applied. The reasons for an incomplete basic treatment were: significant improvement or personal problems. In 19 cases, pentosan polysulphate sodium was administered by varying periods of time, ranging from 6 months to 9 years, with an average of 2.26 years per patient. Six patients couldn’t obtain this drug because it is not available in our country.
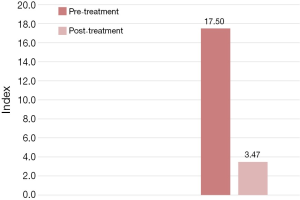
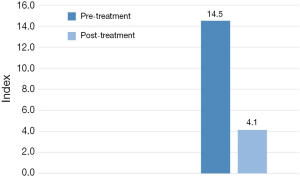
The ICSI and ICPI questionnaires after 3 months follow-up were applied to patients with the following results: ICSI pre-treatment 17.50 (average score, range: 9 to 20) and post-treatment 3.47 (average score, range: 2-20), which means significant symptomatic improvement (Figure 1). In relation to the ICPI average score, pre-treatment was 14.5 (range: 7 to 17) and post-treatment 4.1 (range: 1 to 12) (Figure 2). One single patient did not show improvement objectively with these questionnaires, so that we consign it as failure. There were patients that had some relapses although with slight symptoms, so we had to try new dosages. There was a patient who needed 24 instillations in the course of several years. We have coined the term “remission”, instead of the term “cure” in three cases which have an asymptomatic period without medication.
From the original 33 patients with diagnosis of IC/PBS were excluded eight, two of them rejected the treatment, five because they lived far from our city and the other one abandoned the treatment.
Discussion
IC was described since the beginning of the 19th century (8). However, it continues to be a condition that presents major challenges regarding its diagnosis and treatment. There are few clinical urogynecologic conditions that causes greater frustration than IC/PBS. This is due to its chronicity, serious impairment of quality of life, diagnostic difficulties and unsatisfactory treatment.
It is very common to observe a significant lack of knowledge of this condition in the medical order. The desperate patient because of her ailment wanders from office to office, without finding in the gynecologist or urologist, the expected support. The severity of IC/PBS symptoms and the lack of therapeutic response often cause feelings of frustration, depression and distress, resulting in difficulty in the diagnosis and poor adherence to treatment.
In the last 20 years, several international urogynecological societies have promoted the study of this syndrome, trying to raise awareness in the urologist and gynecologist of its detection and diagnosis. They have also designed clinical guidelines making its management much easier (9).
In the diagnostic order, our position suggests the guidelines from the 1st International Consultation on Incontinence sponsored by the World Health Organization. The medical history consigns the presence of pain, pressure and discomfort for more than 6 months, with urinary frequency and urgency. This is supported by de urogynecology questionnaires.
Conclusions
It is our feeling that although there are not identified issues in the pathophysiology of this syndrome, there are effective treatments that can offer significant improvement or even remission in a high proportion of patients. The good results obtained by this therapeutic scheme, encourages us to continue this line of management as arising in the future new options.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Hanno P, Dmochowski R. Status of international consensus on interstitial cystitis/bladder pain syndrome/painful bladder syndrome: 2008 snapshot. Neurourol Urodyn 2009;28:274-86. [PubMed]
- Hanno P, Lin A, Nordling J, et al. Bladder Pain Syndrome Committee of the International Consultation on Incontinence. Neurourol Urodyn 2010;29:191-8. [PubMed]
- Pang X, Marchand J, Sant GR, et al. Increased number of substance P positive nerve fibres in interstitial cystitis. Br J Urol 1995;75:744-50. [PubMed]
- Harrington DS, Fall M, Johansson SL. Interstitial cystitis: bladder mucosa lymphocyte immunophenotyping and peripheral blood flow cytometry analysis. J Urol 1990;144:868-71. [PubMed]
- Ito T, Ueda T, Honma Y, et al. Recent trends in patient characteristics and therapeutic choices for interstitial cystitis: analysis of 282 Japanese patients. Int J Urol 2007;14:1068-70. [PubMed]
- Parsons CL. The role of the urinary epithelium in the pathogenesis of interstitial cystitis/prostatitis/urethritis. Urology 2007;69:9-16. [PubMed]
- Flores-Carreras O, González-Ruiz MI, Martínez-Espinoza CJ. The Importance of Urethrocystoscopy and Bladder Biopsy in Gynecologic Patients. In: Darwish A, editor. Basic Gynecology - Some Related Issues. 1st ed. InTech, 2012.
- Parsons JK, Parsons CL. The historical origins of interstitial cystitis. J Urol 2004;171:20-2. [PubMed]
- Hanno PM, Erickson D, Moldwin R, et al. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome: AUA guideline amendment. J Urol 2015;193:1545-53. [PubMed]