
Using retroperitoneal laparoscopic ureterolithotomy in the treatment of impacted upper ureteric calculi
Introduction
The ideal treatment for upper ureteric calculi is still being debated, particularly for patients with large, impacted calculi (1,2). The conventional treatments include extracorporeal shock wave lithotripsy (ESWL), transurethral ureteroscopy lithotripsy (URL), flexible ureteroscopy (FURS), percutaneous nephrolithotomy (PCNL), retroperitoneal laparoscopic ureterolithotomy (RLU).
ESWL is a common treatment, but it is affected by the limitations of diffusion space, inflammatory polyp and tortuous ureter, which often make the effect of crushing and removing stones unsatisfactory (3). ESWL may not be effective because impacted calculi are usually wrapped around or adhere to ureteral polyps. When this happens, URL or FURS are options for treatment, but they can have a lower clearance rate and greater risk of complications (3-5). When URL treats the upper ureteral stones, the incidence of the stones moving up to the kidney can be as high as 25–40% (6). Another treatment option is PCNL. The advantages of PCNL are simple operation, no need to establish pneumoperitoneum, and avoid pneumoperitoneum related complications. But serious bleeding and infection are unavoidable risks of PCNL (7). The main cause of PCNL bleeding is the damage of renal parenchyma and the intraoperative injury. In recent years, the incidence of renal artery embolism in PCNL is 0.80–2.74% (8). Serious infection was related to the amount of perfusion fluid and the pressure of perfusion during surgery (9). To avoid these complications, the laparoscopic approach may be a worthwhile alternative to open surgery. The laparoscopic approach of RLU was reported by Wickham in 1979. After Gaul described an innovative retroperitoneal laparoscopic balloon dissection technique did laparoscopic urology become established as a minimally invasive therapeutic method. The advantage of RLU is that there is no need to establish renal parenchymal channel and perfusion during stones removal. But RLU can cause stones displacement, postoperative leakage of urine and ureteral stricture. In this paper, we present our experience in avoiding migration of the stones using RLU in the treatment of impacted upper ureteric calculi. We present the following article in accordance with the STROBE reporting checklist (available at https://tau.amegroups.com/article/view/10.21037/tau-21-1155/rc).
Methods
Patients
The medical records of 64 patients were retrospectively reviewed. These patients underwent RLU between April 2018 and January 2020 at Department of Urology, People’s Hospital of Dongxihu District, Wuhan, China, to treat large impacted upper ureteric calculi. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Dongxihu District People’s Hospital of Wuhan (No. DXHRM 2020-10) and informed consent was taken from all the patients.
Case screening
Patients were included in the study if they had large impacted upper ureteric calculi located from the ureteropelvic junction to the upper edge of the pelvis in one side of the ureter for more than 4 weeks. A stone was considered large if its longest diameter was greater than 1.5 cm. Stones were observed by computed tomography urography (CTU) or a plain X-ray of the kidney, ureter, and bladder (KUB) (10-13). Patients, who had abnormal coagulation, serious internal diseases such as heart disease and diabetes, pyohydronephrosis, abdominal trauma, or a history of operations were excluded from the study. We performed RLU only when the patients provided written consent. Each patient was fully explained the nature of RLU and the possible complications, including adjacent organ injury and unrecognized bowel injury and conversion to open surgery. After following the exclusion criterion and after receiving informed consent, 64 patients underwent RLU. All 64 patients had received a definite diagnosis from the results of their CTU scans.
The data is presented as mean ± standard deviation (SD), as appropriate. The size of the ureteral stone was evaluated as the largest diameter of the stone as identified by unenhanced multidetector computed tomographic (MDCT) scan. The scans were evaluated on Picture Archiving Computer System with a reformatted 3-mm coronal sections (14). The mean degree of hydronephrosis was considered to be the extended of the renal pelvis and was examined by ultrasonography.
Operation and technique
To avoid stone migration, KUB was taken at 1 hour before the operation to confirm that the stone had not moved at that time. The patient was initially positioned in supine position for intravenous access, the induction of general anesthesia, endotracheal intubation, and bladder catheterization. Then, the patient was positioned in a 90° lateral decubitus position prior to the procedure. RLU was performed by using a typical three-port retroperitoneal approach. The ureter was found by taking the psoas as the base and dissecting the Gerota’s fascia to the ventral abdomen. Subsequently, we freed the upper ureter. The ureteric calculi were identified rapidly below the dilated proximal ureter.
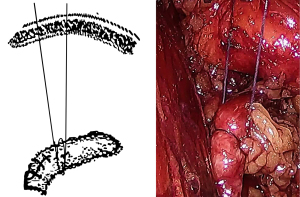
After this, we used a percutaneous suture-wrapping method. Under vision, an absorbable suture was inserted using a 2-0 puncture needle through the abdominal wall to the lower edge of the dissected ureter. Pull the suture out of the tissue after wrapping the ureter 1.5 times. Then, the assistant tightened the suture extracorporeally. With this method, the dissected ureter cannot only be easily elevated, but can also be tightened to reduce urine outflow, which can shorten the suturing time. In addition, when FURS was needed to treat migrated stones, this method can help to reduce leakage of irrigation fluid by narrowing the gap between the ureteral wall and the FURS (Figure 1).
The next issue was how to make sure that the Double J (DJ) tube was placed properly. Before surgery, the urethral catheter was inserted into the bladder, and 50ml of diluted vigorous iodine solution or methylene blue solution was injected into the catheter. Then, the catheter was clamped. After placing the DJ stent [size: 4F-6F (Cook Medical)], we pressed the bladder area. When stained urine flowed to the incision of the ureter, this indicated that the stent had been placed successfully. Then, the ureteral incision could be closed using 4-0 absorbable sutures with a needle spacing of 2 mm, using an interrupted suture. A retroperitoneal drain was inserted and removed 3 days later, and the urethral catheter was removed 5 days after surgery. KUB was performed at 1 month postoperatively. Stone-free status was defined as complete stone clearance in KUB. After the patient was stone-free, the DJ stent was extracted by cystoscopy.
Follow-up
The patients involved in this study were followed up for 12 months after surgery. In this time, a urologic ultrasound was performed every 3 months and CTU was performed every 6 months.
Statistical analysis
Data was analyzed for statistical significance using SPSS software version 19.0 (SPSS Inc., Chicago, USA). The data is presented as mean ± SD, as appropriate. Continuous variables were examined using Student’s t-test and categorical variables were examined using Chi-square. A P value of <0.05 was considered statistically significant.
Results
The mean age of the patients was 50.8±25.4 years. A total of 38 patients were male and 26 were female. The mean largest stone diameter was 1.8±0.3 cm. The mean stone retention time was 42±11 days. The mean degree of hydronephrosis was 2.8±1.2 cm. The patient characteristics are presented in Table 1.
Table 1
| Gender (male/female) | Age (years) | Stone largest diameter (cm) | Stone retention time (day) | Degree of hydronephrosis (cm) |
|---|---|---|---|---|
| 38/26 | 50.8±25.4 | 1.8±0.3 | 42±11 | 2.8±1.2 |
Data are displayed as mean ± standard deviation.
Data are displayed as n or mean ± SD (range). Stone retention time was defined as the duration (days) that a patient had an impacted upper ureteric calculi located from ureteropelvic junction to the upper edge of the pelvis in one side of the ureter.
The mean operative time was 85.4±18.3 minutes. The mean hospital duration was 7.5±1.8 days. The stone-free rate was 98.4%. Two patients required additional intervention because of migration of the stone into the kidney. Laparoscopic guided flexible ureteroscopic extraction of the kidney stone was carried out as an adjuvant procedure. One succeeded and the other failed because the patient’s renal pelvic was inconspicuously dilated. The failed case was then changed to an open procedure. Postoperative fever developed in 3 patients. The decrease in hemoglobin levels was 7.8±3.6 g/L. The increase in procalcitonin (PCT) level was 3.7±1.8 ng/mL. No major complications, for example, sepsis, bleeding, bowel injury, or cardiopulmonary morbidities, were reported. The perioperative records are presented in Table 2.
Table 2
| Operative time (min) | Hospitalization days (d) | Stone-free status | Add operation | Post-operative fever | Decrease in hemoglobin level (g/L) | Increase in PCT level (ng/mL) |
|---|---|---|---|---|---|---|
| 85.4±18.3 | 7.5±1.8 | 63 (98.4) | 2 (3.1) | 3 (4.7%) | 7.8±3.6 | 3.7±1.8 |
Data are displayed as n (%) or mean ± standard deviation (range). PCT, procalcitonin.
Discussion
As the laparoscopic surgeries in urology involve increasingly difficult and technique-dependent operations, documentation and analysis of experience is important for the development of this surgical modality (15,16). The current study aimed to share our experience and the lessons we learnt from RLU procedures, which we have been performing for more than 6 years. From our experience, we recommend RLU be the procedure of choice in large (>1.5 cm) ureteral stones impacted in the mucosa, for which previous research has shown that ESWL and endourological techniques were less effective(3,4). When a skilled surgeon performs RLU for an upper ureteral stone larger than 1.5 cm, our results showed that the operation can have a high success rate, a low complication rate, and a short length of operative time and hospital duration.
The most significant difficulty in the retroperitoneal approach was finding the ureter within the fat tissue of the Gerota’s fascia. In our experience, we looked for the ureter out of the Gerota’s fascia, close to the psoas muscle, without removing the retroperitoneal fat or dissecting the renal pelvis. By doing this, the operation time could be reduced, and more retroperitoneal fat could be retained that helped absorb urine leakage.
KUB was taken at 1 hour preoperatively to ensure the stone does not migrate at that time. Dissection of the ureter from the bulge to the stone site should be performed carefully. Then, the dilated proximal ureter above the ureteral stone should be clamped by non-crushing grasping forceps or laparoscopic vascular forceps. Furthermore, the suture-banding method that we outlined in the results can also avoid migration of the stone into the kidney. We believe that this method can try to be popularization and application to promote the further update of the surgical techniques, because compared with the traditional method, this method has two novelties: 1. Use of laparoscopic vascular forceps; 2. The suture-banding method that we outlined in the results can also avoid migration of the stone into the kidney (Figure 1)
A major complication of laparoscopic ureterolithotomy is ureteral stricture (17), which did not occur in our study. Ureteral stricture can be caused by opening the ureter using a diathermy hook electrode. To avoid this, our experience showed that laparoscopic vascular scissors or a laparoscopic scalpel to open the ureter should be used as often as possible. If the ureter was dilated, or the ureteral wall was thick, the diathermy hook electrode could be used by lowering the energy. In addition, cutting the ureter at the upper part of the stone where it is dilated can also reduce the occurrence of ureteral stricture.
Our experience showed that placement of a DJ stent in the ureter through the laparoscope before suturing was also an effective way to avoid postoperative ureteral stricture and urinary leakage. To do this, make sure the lower part of the DJ stent was inserted in the bladder, and have a sense of smoothness when placing the stent. If there is any resistance, a surgeon can replace the stent with a smaller DJ stent and try again.
Among the 3 patients who had a postoperative fever, 2 occurred because of pulmonary infection caused by endotracheal intubation, while the other was due to a retroperitoneal infection caused by long-term urinary leakage and poor drainage after the operation. This case of urinary leakage occurred in early surgical cases and was related to the rough suture technique used during surgery. Being highly skilled in suture technique can avoid long-term urinary leakage.
Conclusions
Our empirical method can increase the success rate, reduce the complication rate, shorten the length of operative time and hospital duration, making RLU become an excellent first line treatment modality for impacted upper ureteric calculi (>1.5 cm).
Acknowledgments
Funding: This work was supported by the Health Science Foundation of Wuhan City (No. WZ20B03).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://tau.amegroups.com/article/view/10.21037/tau-21-1155/rc
Data Sharing Statement: Available at https://tau.amegroups.com/article/view/10.21037/tau-21-1155/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tau.amegroups.com/article/view/10.21037/tau-21-1155/coif). All authors report funding from the Health Science Foundation of Wuhan City (No. WZ20B03). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Dongxihu District People’s Hospital of Wuhan (No. DXHRM 2020-10) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Mugiya S, Ozono S, Nagata M, et al. Retrograde endoscopic management of ureteral stones more than 2 cm in size. Urology 2006;67:1164-8; discussion 1168. [Crossref] [PubMed]
- Simforoosh N, Basiri A, Danesh AK, et al. Laparoscopic management of ureteral calculi: a report of 123 cases. Urol J 2007;4:138-41. [PubMed]
- Lopes Neto AC, Korkes F, Silva JL 2nd, et al. Prospective randomized study of treatment of large proximal ureteral stones: extracorporeal shock wave lithotripsy versus ureterolithotripsy versus laparoscopy. J Urol 2012;187:164-8. [Crossref] [PubMed]
- Kaygısız O, Coşkun B, Kılıçarslan H, et al. Comparison of ureteroscopic laser lithotripsy with laparoscopic ureterolithotomy for large proximal and mid-ureter stones. Urol Int 2015;94:205-9. [Crossref] [PubMed]
- Kallidonis P, Kalogeropoulou C, Kyriazis I, et al. Percutaneous Nephrolithotomy Puncture and Tract Dilation: Evidence on the Safety of Approaches to the Infundibulum of the Middle Renal Calyx. Urology 2017;107:43-8. [Crossref] [PubMed]
- Desai MR, Patel SB, Desai MM, et al. The Dretler stone cone: a device to prevent ureteral stone migration-the initial clinical experience. J Urol 2002;167:1985-8. [Crossref] [PubMed]
- Li Q, Wan L, Liu S, et al. Clinical efficacy of enhanced recovery after surgery in percutaneous nephrolithotripsy: a randomized controlled trial. BMC Urol 2020;20:162. [Crossref] [PubMed]
- Chen L, Li JX. Prevention of complications after percutaneous nephrolithotripsy. Journal of Modern Urology 2013;18:527-531.
- Wollin DA, Preminger GM. Percutaneous nephrolithotomy: complications and how to deal with them. Urolithiasis 2018;46:87-97. [Crossref] [PubMed]
- Sarica K, Kafkasli A, Yazici Ö, et al. Ureteral wall thickness at the impacted ureteral stone site: a critical predictor for success rates after SWL. Urolithiasis 2015;43:83-8. [Crossref] [PubMed]
- Elibol O, Safak KY, Buz A, et al. Radiological noninvasive assessment of ureteral stone impaction into the ureteric wall: A critical evaluation with objective radiological parameters. Investig Clin Urol 2017;58:339-45. [Crossref] [PubMed]
- Yoshida T, Inoue T, Omura N, et al. Ureteral Wall Thickness as a Preoperative Indicator of Impacted Stones in Patients With Ureteral Stones Undergoing Ureteroscopic Lithotripsy. Urology 2017;106:45-9. [Crossref] [PubMed]
- Wang Y, Zhong B, Yang X, et al. Comparison of the efficacy and safety of URSL, RPLU, and MPCNL for treatment of large upper impacted ureteral stones: a randomized controlled trial. BMC Urol 2017;17:50. [Crossref] [PubMed]
- Nazim SM, Ather MH, Khan N. Measurement of ureteric stone diameter in different planes on multidetector computed tomography--impact on the clinical decision making. Urology 2014;83:288-92. [Crossref] [PubMed]
- Demirci D, Gülmez I, Ekmekçioğlu O, et al. Retroperitoneoscopic ureterolithotomy for the treatment of ureteral calculi. Urol Int 2004;73:234-7. [Crossref] [PubMed]
- Fan T, Xian P, Yang L, et al. Experience and learning curve of retroperitoneal laparoscopic ureterolithotomy for upper ureteral calculi. J Endourol 2009;23:1867-70. [Crossref] [PubMed]
- Ercil H, Altunkol A, Kuyucu F, et al. Experience and learning curve of retroperitoneal laparoscopic ureterolithotomy. Asian J Surg 2015;38:91-5. [Crossref] [PubMed]
(English Language Editor: C. Mullens)


